Diabetes: a therapeutic framework
DIABETES MELLITUS
Understanding Type 1 and Type 2
Diabetes and Disease Progression
Buge Apampa PhD MRPharmS
Some Questions to start off!
1. How many people are expected to have diabetes
in the UK by 2025? [5m]
2. What is the estimated hourly cost of diabetes to
3. How many diabetic patients are dying avoidably
each year? [24,000]
4. How many parameters must be checked annually
in diabetic patients? [9]
5. What % of patients treated with insulin for < 2y
reported a hypoglycaemic episode? [51%]
Objectives
•Burden of Diabetes Mellitus •Refresher of Type 1 & Type 2 DM
•Evidence base for management •Optimising your professional role
Burden of Diabetes Mellitus
Commonest
amputations
Single largest cause
Depression
of blindness
Kidney Disease
Diabetes
Stroke – 2-4 x
Heart attack: 2-4 x death
increased risk
• 10% of NHS budget
• 2002- NHS spend of £1.3 billion
• 2011- NHS spend on diabetes nearly £10
• Net ingredient cost of £760.3m (9% of all
total cost of Rxs)
NICE 2008 Targets
Average 6.5% 48 mmol/mol
Total Cholesterol
Nine Diabetes Checks
1. Blood pressure
2. Weight and waist circumference
4. HbA1C 5. Urinary albumin
6. Serum creatinine
7. Foot & leg check
8. Smoking status
9. Eyes- retinal screening
National Diabetes Audit
• Reviewed records of 1.7m diabetics in England &
Wales for 9 recommended checks
• 50% of Type 2 DM received the checks
• 33% of Type 1 DM received the checks
• Completion influenced by ethnicity & age
• Younger people less likely to receive checks
Preventing additional deaths in people
with Diabetes
(Diabetes health Intelligence YHPHO)
• England 2011, diabetics
had 39.9% greater risk of dying compared to general population
• Over 20,000 additional
deaths among diabetics
• If all PCTs with highest
additional risk of diabetics dying reduced the risk to the England ave 2150 fewer deaths in 2011


Preventing Disease Progression: Is there a Role for Pharmacists?
Some Facts about Diabetes
• About 3 million people with diabetes in UK • Represents 72% of estimated prevalence • 12 times more type 2 than type 1 • Prevalence increasing- ageing population and obesity • 8% Type 1 diabetes - can occur at any age after 18m
but has peak incidence in children aged10-15y
• 92% Type 2 diabetes • 850,000 thought to be undiagnosed • 40% increased prevalence among people in deprived
• Prevalence of diabetes nearly 4 times higher than
prevalence of all cancers combined
Possible signs/symptoms of diabetes
• Increased thirst • Polyuria • Recurrent infection • Diabetic complication • Weight loss • Extreme tiredness or lethargy • Slow wound healing • Itchy skin rash • Blurred vision • Tingling pain & numbness in feet, legs or hands
WHO diagnostic thresholds for venous plasma
glucose (mmol/l)
Diabetes ≥ 7.0
≥11.1 ≥11.1
mellitus
Impaired N/A
< 11.1 ≥7.8
<11.1
Impaired 6.1-<7.0
affected
48 mmol/mol by food
Type 1 vs. Type 2 diabetes
Lambert P, et al. Medicine 2006; 34(2): 47-51
Nolan JJ. Medicine 2006; 34(2): 52-56
Features of type 1 diabetes
Features of type 2 diabetes
• Usually presents in over-30s (but
also seen increasingly in younger
childhood/adolescence
• Lean body habitus
• Associated with overweight/obesity
• Acute onset of osmotic
• Onset is gradual and diagnosis
often missed (up to 50% of cases)
• Ketosis-prone
• Not associated with ketoacidosis,
though ketosis can occur
• High levels of islet
• Immune markers in only 10% • Family history is often positive with
• High prevalence of genetic
almost 100% concordance in
1. Gestational diabetes: Diabetes first
diagnosed in pregnancy irrespective of cause
2. Latent autoimmune diabetes of adults (slowly
progressing type 1?)
3. Type 2 diabetes presenting with diabetic
ketoacidosis (common in UK black population; acute partial temporary β-cell failure; complete remission)
4. Type 2 diabetes presenting in children and
Complications of Diabetes
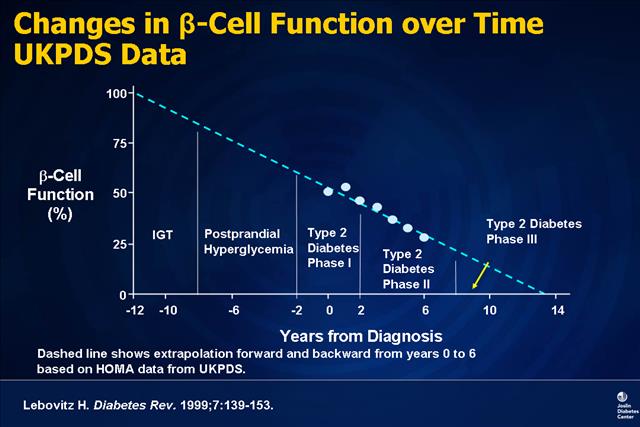
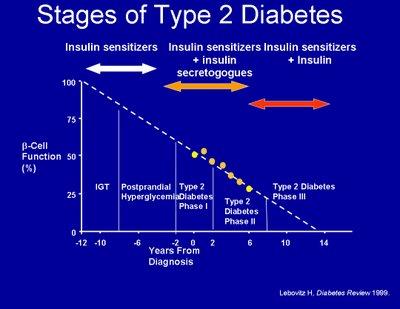
Disease Progression
• In the late 80s, 44% o f patients in the West with
type 2 DM, died within 10 years of diagnosis mostly due to macrovascular disease
• Incidence & mortality from CVD 2-3 x greater
than the general population
• Complications present in up to 50% at
• Other risk factors for CVD (hypertension,
hyperlipidaemia) present
• Long term damage of eyes, kidney, nerves,
heart and blood vessels
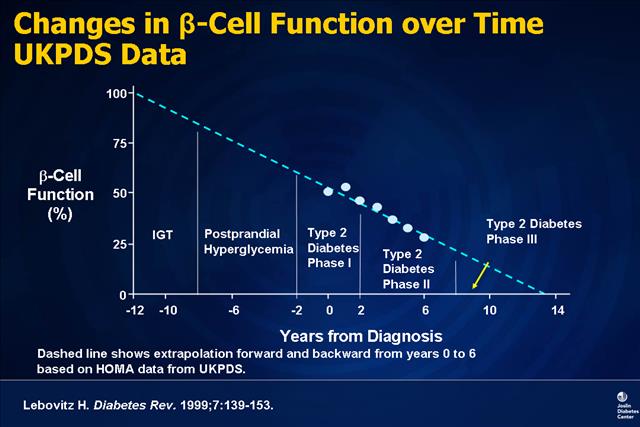
UKPDS: Progressive Deterioration in
Glycemic Control Over Time
Macrovascular Complications
• More common in Type 2
• Myocardial infarction
• Ischaemic heart disease
• Cerebrovascular disease
• Peripheral vascular disease
Microvascular Complications
• More common in Type 1
• Retinopathy present in all patients after 20
years. Can lead to blindness
• Nephropathy accounts for 1 in 4 kidney
• 40% Type 1 and 20% Type 2 develop end
stage renal disease
• Neuropathy (nerve pain, amputation, ED)
Type 1 Diabetes - A Refresher
Type 1 Diabetes
• Autoimmune destruction of pancreatic β cells
(viral or autoimmune)
• Immediate and permanent requirement for
• Insulin requirement may be minimal during
‘honeymoon' period (6-18 months after diagnosis)
• Fatal if not treated
Clinical presentation
• Rapid/abrupt onset of acute osmotic symptoms • Ketonuria and / or metabolic acidosis at presentation
• Unintentional weight loss which may or may not be
accompanied by ketoacidosis
• Vascular complications not evident at presentation
Pharmacotherapy-Type 1 DM
• Insulin: all Type 1 DM will require insulin • Subcutaneous route is preferred however
intravenous route is used (soluble insulin) in emergencies
• 3 main types of insulin available: • Short acting - soluble insulin, lispro and aspart,
• Intermediate - isophane zinc and insulin zinc susp. • Slower onset and longer acting - crystalline insulin
zinc susp, detemir, glargine
Goals of Insulin Treatment
• To mimic both types of insulin secretion • Require basal insulin and meal-related insulin
• General requirements: 1unit/kg/24h in type 1 • Insulin analogues e.g. Humalog, NovoRapid →
better mimic physiological profile of insulin, improved control
• More convenient for patients, can be used
15mins before to immediately after a meal
• Reduced frequency of "hypos" due to shorter
Approximate pharmacokinetic profiles of
human insulin and insulin analogues
Hirsch IB. N Engl J Med 2005; 352: 174-83
N.B. Duration of action will vary widely between and within people
NPH = neutal protamine hagedorn/isophane insulin
Insulin choices in adults:
• Meal time insulin
– soluble – rapid acting analogues where "hypos" a
• Basal Insulin
– Isophane (NPH) at bedtime or bd – Long acting analogues (glargine) where
night time "hypos" or morning "hypers" a problem with NPH or rapid acting meal time analogues used
NICE Insulin Regimens
• Multiple insulin injections: for adults who prefer
them as part of an integrated package of education, food, skills training and self-monitoring
• Twice-daily insulin regimens:
1. for those who find adherence difficult
2. adults with learning difficulties who may require
3. where no of injections is a quality of life issue 4. Biphasic insulin preparations are often the
preparation of choice
5. Biphasic rapid-acting insulin analogue premixes may
give an advantage to those prone to hypoglycaemia at
Supporting Evidence Base: DCCT 1993
• Intensive treatment vs conventional
• 1,441 patients with Type 1 diabetes, mean age 27
• Active group- insulin 3-4 times a day with >4 blood
tests a day supported by monthly clinics
• Control group received twice daily insulin and
standard monitoring
• 60% reduction in microvascular complications
• 44% reduction in macrovascular complications
• Conclusion: Tight control with intensive insulin therapy
reduces development & progression of microvascular outcomes
Factors affecting insulin requirements
Increased insulin
Decreased insulin requirements
• Renal failure
• Adrenal insufficiency
• Increased exercise
• Inactivity • Hyperthyroidism • Cushing disease
Type 2 Diabetes - A Refresher
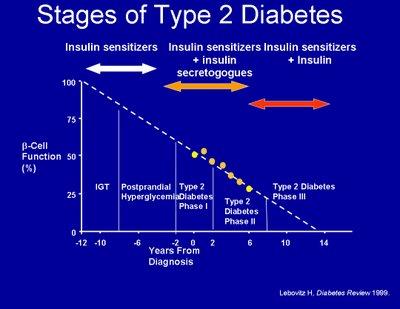
Type 2 Diabetes
• Relative insulin deficiency due to disorders of insulin action
(insulin resistance) or secretion
• Progressive disease; β cell dysfunction to IGT to T2DM • β cell dysfunction starts before blood glucose rises and
worsens after diabetes develops
• Failure of β cell to adequately compensate for insulin
• Strong genetic basis for β cell failure (Asians, Middle Eastern,
African-Caribbeans & Africans)
• Linked to hypertension and obesity (most common cause of
insulin resistance)
Risk factors for Type 2 diabetes
• Obesity, BMI > 30; 47% of Type 2 DM in England (NAO)
• Age (> 40 if white; > 25 if black, asian)
• Waist measurement > women 31.5in; 35in Asian men;
37in white or black men
• Sedentary lifestyle – 30-40% increased risk
• Ethnicity: African-Caribbean, South Asian, Middle
• Family history – 1st degree relative
Other Risk Factors for Type 2 diabetes
• Social deprivation- diabetes-related mortality
higher in lower SEGs
• Large birth weight baby > 4.5kg
• Previous gestational diabetes • Hypertension or dyslipidaemia (metabolic
• Impaired fasting glycaemia and impaired
glucose tolerance
Clinical Presentation
• Onset of osmotic symptoms over a variable period • Positive family history- 1st degree relatives
• Variable weight loss
• Glucose excellent medium for microbial growth -
presenting symptoms may include recurrent vaginal, respiratory infections
• Hypergylcaemia – 7-10 years pre-diagnosis
• 20% have microvascular or macrovascular complications
Selected evidence base for Type 2
• Finnish, DPP, Da Qing: Intensive lifestyle
intervention studies
• UKPDS: Blood glucose and BP in patients with
• ACCORD & ADVANCE: Impact of intensive
glucose lowering in patients with high cardiovascular risk
• VADT: Impact of intensive glucose lowering in
patients with low cardiovascular risk
• HOPE: (Ramipril) • HPS (Simvastatin)
1. Lifestyle intervention
• Intensive lifestyle interventions prevent or
delay risk of progression to diabetes
• 42% reduction in Da Qing Study (China, 1997)
• 58% reduction in Finnish Diabetes Prevention
• 58% reduction Diabetes Prevention Program
2. UKPDS, 1998
• 20 year multi-centre RCT involving 5102 patients with
type 2 diabetes aged 25-65 years
• Randomised to intensive treatment or diet only therapy
• Research question:
1. Would intensive glycaemic control &/or tight BP control
reduce the risk of complications?
2. Does any specific treatment for blood sugar or blood
pressure control confer particular benefit?
2.1 UKPDS findings: Blood
• SU/Insulin vs conventional treatment lasted
• Lowering blood glucose reduced risk of;
– Eye disease by 25% – Kidney disease by 25%
• Every 1% reduction in HbA1c reduced;
– Retinopathy, neuropathy & nephropathy by
2.2 UKPDS findings: Metformin
• Median follow up was 10.7 years • Metformin compared with conventional treatment
(diet) reduced the risk of:
• Any diabetes-related endpoint by 32%
• Diabetes –related death by 42%
• All cause death by 36%
• Myocardial infarction by 39%
• Conclusion: MTF decreases the risk of death and
of having an MI, but not the risk of microvascular
complications
• ACCORD study: Intensive therapy (A1c < 6%) led to
increased mortality
• No effect on primary endpoint (MI, stroke or CV death)
• ADVANCE study: Intensive therapy (A1c < 6.5%) had no
significant effect on macrovascular events or all-cause mortality, but it did reduce nephropathy
• VADT study, 2009:Tight control of glucose did not reduce
the risk of major CV events, microvascular complications or death
• Patients in the intensive treatment arm were more likely to
experience hypoglycaemic episodes
5. UKPDS: Blood Pressure
• UKPDS: Tight BP control decreased the risk of diabetes
related death, stroke and microvascular disease
• Lowering blood pressure reduced
– Any diabetes related end point by 24% – Diabetes-related deaths by 32% – Strokes by 44% – Diabetes-related microvascular end points by 37%
• HOPE study: Ramipril significantly reduced the risk of MI,
stroke or CV death cf placebo
– MI 33% – Stroke 33% – CV death 37%
• HPS: In high-risk patients with a wide range of
baseline cholesterol values
• Simvastatin 40mg reduced:
• All-cause mortality • Coronary deaths • Major vascular events
7. Diastolic BP and Aspirin
• HOT trial: In patients with diabetes • Lowering DBP to 80mmHg
– Reduced risk of major CV events by 51%
• Aspirin 75mg
– Reduced major cardiovascular events by
– Reduced MI by 36% (P=0.002) – no effect on stroke incidence
Pharmacotherapy of Type 2
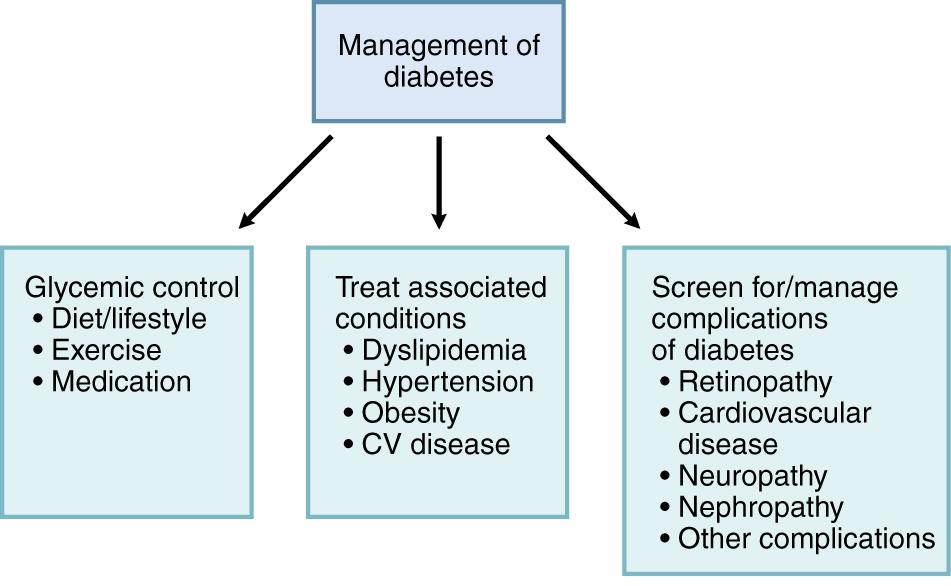
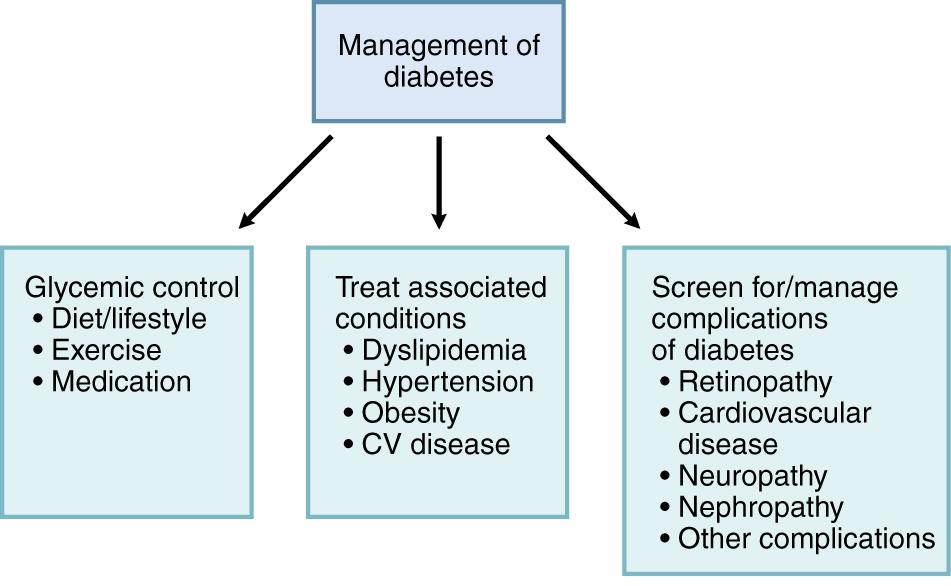
Goals of management www.npci.org.uk
• Manage symptoms • Prevent acute and late complications • Improve quality of life • Avoid premature diabetes-associated death • An individualised approach
(e.g. diet & exercise)
Microalbuminuria
Key Actions to Prevent
progression of Type 2 diabetes
1. Intensive lifestyle intervention
3. Statin therapy
4. Metformin and aspirin
5. Blood glucose control
3 Add statin
4 Add metformin
2 Control BP
(and aspirin if
5 consider
tight glucose
control
1 Lifestyle
(exercise, diet,
stop smoking)
Let's give our diabetic
patients a hand!

Lifestyle modification
• Weight reduction (5-10%) if
• Low GI CHO - pasta, basmati,
oats, beans, peas, lentils, seeds
• Replace saturated fats with
mono-unsaturated fats
• Fruits & vegetables- 5 portions
• Regular intake of fish • Less than 6g salt/day • Portion control • Control alcohol intake: 3u/2u

Lifestyle modification:
Activities of daily living
• Moderate intensity
exercise 150 min / 5 days
• More walking, cycling,
swimming, gardening
• Reduce sedentary
• Stop Smoking
2. BP: Choice of antihypertensive
NICE Diabetes Clinical Guideline 66;May 2008. NICE Full Diabetes
• BP target: <140/80 or <130/80 if complications • First-line BP lowering therapy should be a once-daily,
generic ACE inhibitor
• Exceptions to this are:
– People of African / African-Caribbean descent – Who should receive an ACE inhibitor plus either a
diuretic or a calcium-channel blocker (CCB)
• Women for whom there is a possibility of becoming
pregnant, who should receive a CCB
• Intolerance in the form of troublesome cough, substitute
an angiotensin-II receptor antagonist for the ACE inhibitor
Most patients will be on ACEI, diuretic and one other BP drug
3. Management of blood lipids
NICE Diabetes Clinical Guideline 66;May 2008. NICE Full Diabetes
• Overwhelming evidence that statins prevent CV events • Generic simvastatin (to 40mg) or a statin of similar efficacy and cost
should be initiated in people:
Aged under 40 years with poor CV risk factor profile
Aged 40+ years with low CV risk for someone with type 2 diabetes but CV risk assessed as > 20% over 10 years using UKPDS risk engine
Aged 40+ years and normal to high CV risk for someone with type 2 diabetes
Increase dose to simvastatin 80mg daily unless total cholesterol <4.0mmol/L or LDL-cholesterol <2.0mmol/L
Management of blood lipids
NICE Diabetes Clinical Guideline 66;May 2008. NICE Full Diabetes
• Intensify therapy with a more effective statin or
ezetimibe if existing or newly diagnosed CV disease or increased albumin excretion rate
• To achieve a total cholesterol level below 4.0mmol/L
or LDL-cholesterol level below 2.0mmol/L
• If TG levels remain above 4.5 mmol/L despite attention
to other causes, prescribe a fibrate
• Fibrate may be added to statin therapy if TG levels
remain in the range 2.3–4.5 mmol/L despite statins
3. Statin Therapy
• Not in patients considered at low CV risk
• Not overweight • No microalbuminuria • No history of CVD • No family history of CVD • Normotensive (BP<140/80) • No high-risk lipid profile • At high risk unless all above apply
4. Antithrombotic Therapy
NICE Diabetes Clinical Guideline 66;May 2008. NICE Full Diabetes
• Aspirin 75mg or if intolerance, clopidogrel should be
initiated in people:
1. Aged 50+ years with BP < 145/90 mmHg
2. Aged < 50 years with significant CV risk factors such
features of metabolic syndrome, strong early family history of CV disease, receiving treatment for hypertension, smokers
Antithrombotic Therapy
• Aspirin is not licensed for the primary prevention
of vascular events
• If used in primary prevention, the balance of
benefits and risks should be considered for each individual
• Presence of risk factors for vascular disease
(including conditions such as diabetes) and the risk of gastrointestinal bleeding
5. Pharmacotherapy:
Blood Glucose
• OHAs may be classed according to their mode of
1. Improve sensitivity to insulin: Biguanides & glitazones
2. Insulin secretagogues: Sulphonylureas & meglitinides
3. Reduce glucose absorption: Acarbose
4. Incretins: GLP-1 analogues & DPP4 inhibitors
5. Sodium- glucose co-transporter 2 (SGLT2) inhibitor:
Dapagliflozin - reversible inhibitor (monotherapy and in combination with insulin and other antidiabetics except PIO)
6. Insulin: commonly used in combination with OHA
Strongly preferred when dual therapy fails
Drug treatment for blood glucose control Based on NICE Clinical Guideline 87;
May 2009 and MeReC Bulletin Vol. 21, No. 5,
Third-line
NPH insulin*
or other higher level
Safety and
Second-line
metformin plus
(48mmol/mol) or other higher level
First-line
metformin*
*other options are available in specific circumstances
UKPDS: Progressive Deterioration in
Glycemic Control Over Time
Newer agents: Incretins
• Dual & Triple Therapy • GLP-1 agonists & DPP-4 inhibitors • Clinical Effects: • Reduce post-prandial hyperglycaemia • Increase glucose-mediated insulin secretion • Suppress glucagon secretion, slow gastric emptying • Decrease appetite • DPP-4 inhibitors (sitagliptin, vildagliptin): continue use
only if HbA1c lowered by ≥ 0.5% in 6 months
• Exenatide: continue use only if HbA1c lowered by ≥ 1.0%
& ≥ 3% initial body weight in 6 months
GLP-1 agonist: Exenatide 5-10ug bd
Dual therapy with MTF, SU or PIO
• Triple therapy with MTF + SU if BMI ≥35 or BMI < 35 and
insulin not acceptable or weight loss necessary
• Practice points: 1. s.c.injection within 60 min before meals
2. Missed doses must not be compensated • Safe in liver impairment & renal impairment where eGFR
3. Enteric coated formulations, OC, antibiotics- to be taken
1hour before or 4h after exenatide
• Advantages: Weight loss, low risk of hypos except when
used with SU or SU/MTF
• Adverse effects: Nausea in 60% of patients; rarely acute
pancreatitis (persistent severe abdominal pain)
GLP-1 agonist: Liraglutide 0.6mg-1.2mg OD
• Once daily administration independent of meals • Dual therapy with MTF or SU • Triple therapy with MTF & SU or MTF & PIO • Not recommended in hepatic impairment • Renal impairment: use only if eGFR>60ml/min • Adverse effects: Nausea • Liraglutide 1.8mg not recommended
Insulin Therapy in T2DM
• Persistent symptoms -
hyperglycaemia, lethargy,
muscle weakness despite maximal dual therapy or during intercurrent illness
• Known safety profile, superior glycaemic control not
proven in trials or often evident in practice
• Similar glycaemic benefits as non-insulin combination
• Does not improve microvascular/macrovascular
outcomes compared with other agents with similar A1C effects
Insulin initiation in type 2 diabetes
• Preferred 3rd line (after MTF + SU)
• NPH insulin- preferred basal insulin; at bedtime or bd
• To start:
• Continue with optimised MTF or SU
• Start fixed dose basal insulin (10-16units) at bedtime
• Insulin titrated at a fixed rate (e.g. 2 units/week) or a %
(e.g. 10% of existing dose)
• Individualised fasting glucose targets (e.g. 5.5 – 6.0
• Low starting dose but will increase with time (up to
• Weight gain (4-6kg) over 3-6 years • A1c lowering of 1.5% (17mmol/mol)
Other Insulin Regimens in T2DM
Once daily long acting insulin analogue (detemir or glargine )
for patients :
– Help with injecting
– Recurrent symptomatic hypos which severely affects their
– Unable to use the Isophane injection device – Require basal insulin injections BD as well as oral therapy
Biphasic human insulin (biphasic isophane insulin) once or
twice daily (if HbA1c ≥9%) is another option
Biphasic insulin analogues (e.g. biphasic insulin aspart):
– If immediate injection before meal is preferred
– Hypos are a problem
– Post prandial hyperglycaemia is an issue
Preventing Disease Progression: Optimising your professional role
– Identifying the estimated 850,000+ undiagnosed, health
checks, spreading awareness
• Adherence support:
– 73.3% increase in diabetes Rx items over the last 6 years – 30-50% of dispensed items not taken as intended – OHA: 70% of people do not take them as prescribed – MURs, NMS, what else?
• Structured Education: Signposting, enhanced service • Smoking: Status checks & support • PHARMACEUTICAL CARE???
– DTPs: Appropriateness, effectiveness, safety
Diabetes Care: The Alphabet Strategy
(George Elliot Hospital NHS Trust)
• Advice- smoking, diet, alcohol, exercise, weight,
education, driving
• Blood Pressure - <130/80 • Cholesterol – TC <4; HDL normal • Diabetes Control – A1c < 6.5%; avoid hypos • Eye Screening - annual • Feet Screening - annual
Guardian Drugs – ACEI, ARB, Cholesterol lowering

Thank You, Any Questions?
Source: http://www.eastsussexlpc.co.uk/wp-content/uploads/sites/14/2014/03/Brighton-Forum-DIABETES-Explained-Feb-2014.pdf
HHS Public AccessAuthor manuscript Eur J Pharm Biopharm. Author manuscript; available in PMC 2016 May 09. Published in final edited form as: Eur J Pharm Biopharm. 2015 September ; 95(Pt B): 239–249. doi:10.1016/j.ejpb.2015.02.013. Intracellular delivery of dendrimer triamcinolone acetonide conjugates into microglial and human retinal pigment epithelial
Effectiveness of policy Chapter 7 – The effectiveness of alcohol policy Alcohol policies can be grouped within five headings: (i) policies that reduce drinking and driving; (ii) policies that support education, communication, training and public awareness; (iii) policies that regulate the alcohol market; (iv) policies that support the reduction of harm in drinking and surrounding environments; and (v) policies that support interventions for individuals. Since the 1970s, considerable progress has been made in the scientific understanding of the relationship between alcohol policies, alcohol consumption and alcohol-related harm. The drinking-driving policies that are highly effective include unrestricted (random) breath testing, lowered blood alcohol concentration (BAC) levels, administrative license suspension, and lower BAC levels for young drivers. The limited evidence does not find an impact from designated driver and safe drive programmes. Alcohol locks can be effective as a preventive measure, but as a measure with drink driving offenders only work as long as they are fitted to a vehicle. The World Health Organization has modelled the impact and cost of unrestricted breath testing compared with no testing; applying this to the Union finds an estimated 111,000 years of disability and premature death avoided at an estimated cost of €233 million each year. The impact of policies that support education, communication, training and public awareness is low. Although the reach of school-based educational programs can be high because of the availability of captive audiences in schools, the population impact of these programs is small due to their current limited or lack of effectiveness. Recommendations exist as to how the effectiveness of school-based programmes might be improved. On the other hand, mass media programmes have a particular role to play in reinforcing community awareness of the problems created by alcohol use and to prepare the ground for specific interventions. There is very strong evidence for the effectiveness of policies that regulate the alcohol market in reducing the harm done by alcohol, including taxation and managing the physical availability of alcohol (limiting hours and days of sale and raising the minimum drinking age). Alcohol taxes are particularly important in targeting young people and the harms done by alcohol. If alcohol taxes were used to raise the price of alcohol in the EU15 by 10%, over 9,000 deaths would be prevented during the following year and an approximate estimate suggests that €13bn of additional excise duty revenues would also be gained. The evidence shows that if opening hours for the sale of alcohol are extended more violent harm results. The World Health Organization has modelled the impact of alcohol being less available from retail outlets by a 24 hour period each week; applying this to the Union finds an estimated 123,000 years of disability and premature death avoided at an estimated implementation cost of €98 million each year. Restricting the volume and content of commercial communications of alcohol products is likely to reduce harm. Advertisements have a particular impact in promoting a more positive attitude to drinking amongst young people, and, even in advertisements that do not portray drinking of alcohol, young people perceive the characters as heavy drinkers. Self-regulation of commercial communications by the beverage alcohol industry does not have a good track record for being effective. The World Health Organization has modelled the impact of an advertising ban; applying this to the Union, finds an estimated 202,000 years of disability and premature death avoided, at an estimated implementation cost of €95 million each year.