Microvide.com

Temporally and Regionally Disparate Differences inPlasmin Activity by Tranexamic Acid
Daryl L. Reust, MD,* Scott T. Reeves, MD,* James H. Abernathy, III, MD,* Jennifer A. Dixon, MD,‡William F. Gaillard, II, BS,‡ Rupak Mukherjee, PhD,‡ Christine N. Koval, BS,‡ Robert E. Stroud, MS,‡and Francis G. Spinale, MD, PhD†‡
BACKGROUND: A major complication associated with cardiac surgery is excessive and pro-longed bleeding in the perioperative period. Improving coagulation by inhibiting fibrinolysis,primarily through inhibition of plasmin activity (PLact) with antifibrinolytics such as tranexamicacid (TXA), has been a pharmacological mainstay in cardiac surgical patients. Despite its almostubiquitous use, the temporal and regional modulation of PLact profiles by TXA remainsunexplored. Accordingly, we developed a fluorogenic-microdialysis system to measure in vivodynamic changes in PLact after TXA administration in a large animal model.
METHODS: Pigs (25–35 kg) were randomly assigned to receive TXA (30 mg/kg, diluted into 50mL normal saline; n ⫽ 9) or vehicle (50 mL normal saline; n ⫽ 7). Microdialysis probes wereplaced in the liver, myocardium, kidney, and quadriceps muscle compartments. The microdialy-sate infusion contained a validated plasmin-specific fluorogenic peptide. The fluorescenceemission (standard fluorogenic units [SFU]) of the interstitial fluid collected from the microdialy-sis probes, which directly reflects PLact, was determined at steady-state baseline and 30, 60,90, and 120 min after TXA/vehicle infusion. Plasma PLact was determined at the same timepoints using the same fluorogenic substrate approach.
RESULTS: TXA reduced plasma PLact at 30 min after infusion by ⬎110 SFU compared withvehicle values (P ⬍ 0.05). Specifically, there was a decrease in liver PLact at 90 and 120 minafter TXA infusion of ⬎150 SFU (P ⬍ 0.05) and 175 SFU (P ⬍ 0.05), respectively. The decreasein liver PLact occurred 60 min after the maximal decrease in plasma PLact. In contrast, kidney,heart, and quadriceps PLact transiently increased followed by an overall decrease at 120 min.
CONCLUSIONS: Using a large animal model and in vivo microdialysis measurements of PLact,the unique findings from this study were 2-fold. First, TXA induced temporally distinct PLactprofiles within the plasma and selected interstitial compartments. Second, TXA causedregion-specific changes in PLact profiles. These temporal and regional differences in the effectsof TXA may have important therapeutic considerations when managing fibrinolysis in theperioperative period. (Anesth Analg 2010;110:694 –701)
tion associated with cardiothoracic, major vascular,
become the major class of pharmacological intervention in
liver transplantation, orthopedic spine, and trauma
which antifibrinolytic therapy is indicated for the manage-
surgeries. Blood products and antifibrinolytics have been
ment of excessive perioperative bleeding and has likely re-
effectively used to achieve needed hemostasis in these clinical
sulted in an increased use of TXA for this purpose. However,
scenarios.1–6 Antifibrinolytics have been the pharmacological
the basic regional and temporal PLact profiles after TXA
mainstay with proven efficacy in reducing blood loss and
administration remain unexplored. Accordingly, the primary
blood product transfusion requirements, particularly in rela-
goal of this study was to characterize the effects of TXA on the
tion to cardiac surgery.1,3 Common clinically used antifibrino-
regional and temporal PLact profiles in plasma and selected
lytics affect plasmin activity (PLact) primarily by inhibiting
the enzymatic interaction of plasminogen/plasmin with
Common clinically implemented weight-based TXA
fibrinogen/fibrin and can be classified as either serine pro-
dosing regimens are largely empirically derived and, as
tease inhibitors or lysine analogues.7 The serine protease
such, there is no consensus as to appropriate dosing to
inhibitor aprotinin significantly inhibits fibrinolysis, but this
provide optimal perioperative control of fibrinolysis.8 This
drug has been removed from clinical use.7 As a consequence,
lack of established clinical dosing regimens suggests thatthe modulation of fibrinolysis by TXA may be enhanced byregional and temporal measurements of PLact. Accord-
From the *Department of Anesthesiology and Perioperative Medicine,Medical University of South Carolina; ‡Ralph H. Johnson Veterans Affairs
ingly, we used a common weight-based TXA dosing
Medical Center; and †Division of Cardiothoracic Surgery, Medical Univer-
scheme to investigate the effects of TXA on regional and
sity of South Carolina, Charleston, South Carolina.
temporal PLact profiles.9 To explore the regional dynamics
Accepted for publication September 27, 2009.
of PLact, we used a large animal model using established
Supported in part by NIH grants HL059165 and HL078650 and a MeritAward form the Veterans' Affairs Health Administration.
microdialysis techniques.10,11 Such microdialysis tech-
Address correspondence and reprint requests to Francis G. Spinale, MD,
niques, utilizing a fluorogenic substrate, allowed the detec-
PhD, Department of Cardiothoracic Surgery, Strom Thurmond Research
tion of interstitial enzymatic activity, such as plasmin.12
Building, 114 Doughty St., Room 625, Medical University of South Carolina,
Accordingly, the objectives of this study were 2-fold. The
Charleston, SC 29403. Address e-mail to [email protected].
first objective was the validation and calibration of a
Copyright 2010 International Anesthesia Research SocietyDOI: 10.1213/ANE.0b013e3181c7eb27
fluorogenic peptide that could be used to assess PLact in
March 2010 • Volume 110 • Number 3

vivo. The second objective was the development of aporcine model to measure PLact in plasma and interstitialregions of clinical relevance using this validated fluoro-genic approach.
METHODSThis study was conducted in 2 stages. First, in vitro validationstudies were performed to develop a PLact measurementsystem using a plasmin-specific fluorogenic substrate.12 Thisvalidated PLact measurement system was used to performin vivo PLact measurements, via microdialysis probes, withintargeted regions. TXA was then infused IV and PLact wascontinuously monitored within these regions. Finally, plasmaTXA and d-dimer concentrations were measured.
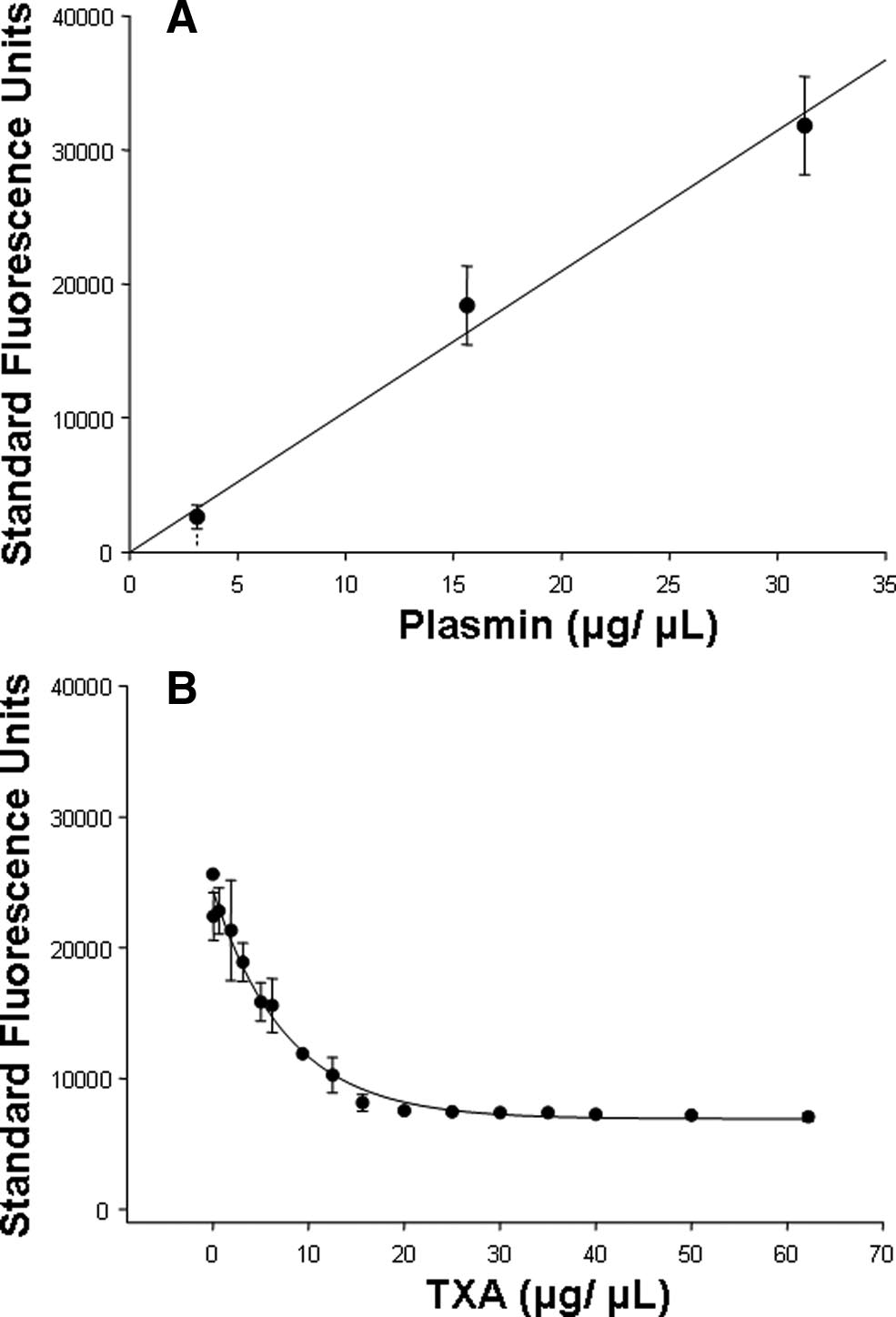
In Vitro ValidationsSeveral in vitro validation studies were performed using aplasmin-specific fluorogenic substrate12 (Cat. #A8171, Sigma-Aldrich, St. Louis, MO). In particular, this substrate containeda validated fluorogenic peptide that, when specificallycleaved by plasmin, yielded a coumarin fluorescent moietywith excitation/emission wavelengths of 365/440 nm, respec-tively.12 The first in vitro validation study determined theresponse of the fluorogenic substrate to increasing concentra-tions of plasmin. Briefly, 6.25 M of plasmin substrate wasinjected into a 96-well polystyrene plate (Nalge Nunc, Roch-ester, NY) with increasing concentrations of plasmin (0–31.25
g/mL; Cat. #P1867, Sigma-Aldrich). After a 5-min incuba-tion at 37°C, the plate was placed into a fluorescence micro-plate reader (FLUOstar Galaxy, BMG LABTECH, Offenburg,Germany) and the fluorescence emission was recorded. Flu-orescence emission, reflective of PLact, increased with increas-ing concentrations of plasmin (Fig. 1A).
Figure 1. A, Fluorescence emission of the plasmin-specific substrate
Next, a series of in vitro experiments was performed
(6.25 g/mL), reflective of plasmin activity (PLact), increased with
using a solution of reference normal porcine plasma, which
increasing concentrations of plasmin (0 –31.25 g/mL) in a linearconcentration-dependent manner (n ⫽ 3, plotted values are mean ⫾
determined the TXA plasma concentration inhibition curve.
SEM; linear regression, y(x) ⫽ 1048.8 ⫻ x, r2 ⫽ 0.996, P ⫽ 0.002).
Specifically, plasmin (31.25 g/mL) and diluted control
B, Fluorescence emission of the plasmin-specific substrate (6.25
porcine plasma (1:32) were incubated with increasing con-
g/mL), reflective of PLact, in the presence of plasmin (31.25
centrations of TXA (0 – 62.2 mg/mL) and subjected to the
g/mL) and control porcine plasma (1:32) decreased in response toincreasing concentrations of tranexamic acid (TXA) (0 – 62.2 mg/mL) in
same fluorescence measurement procedure previously de-
a classic logarithmic concentration-dependent manner13 (n ⫽ 3, plotted
scribed. As shown in Figure 1B, the fluorescence emission,
values are mean ⫾ SEM, regression, y(x) ⫽ 23,280 ⫻ e⫺0.063 ⫻ x, r2 ⫽
reflective of PLact, decreased in response to increasing con-
0.964, P ⬍ 0.001).
centrations of TXA in a classic, logarithmic, concentration-dependent manner.13 A logarithmic equation was matched tothese data using regression analysis.
After sedation with diazepam (100 mg per os, Elkins-
Therefore, these in vitro studies established the optimal
Sinn, Cherry Hill, NJ), general inhaled anesthesia was
substrate concentration, demonstrated specificity of the
induced using isoflurane (3%, Baxter Healthcare, Deerfield,
substrate for plasmin, and determined the fluorescence
IL) mixed with oxygen and nitrous oxide (67%:33%) and
emission inhibition curve for TXA in porcine plasma. The
peripheral IV access was obtained. A stable surgical plane
development of this PLact measurement system was then
of anesthesia was established and maintained throughout
translated to the in vivo PLact studies described below.
the protocol using sufentanil (2 g/kg IV, Elkins-Sinn),etomidate (0.1 mg/kg IV, Elkins-Sinn), vecuronium (10 mg
Animal and Surgical Preparation
IV bolus, 0.5 mg 䡠 kg⫺1 䡠 h⫺1 IV infusion, Ben Venue Labo-
Yorkshire pigs (n ⫽ 16, male, 25–35 kg; Hambone Farms,
ratories, Bedford, OH), morphine sulfate (3 mg 䡠 kg⫺1 䡠 h⫺1
Reevesville, SC) were instrumented to measure plasma and
IV, Elkins-Sinn), and isoflurane (1%, Baxter Healthcare).
interstitial PLact. All animals were treated and cared for in
Tracheal intubation was achieved via tracheostomy, and
accordance with the National Institutes of Health Guide for
mechanical ventilation was established (Narkomed 2B,
the Care and Use of Laboratory Animals (National Institutes
North American Drager, Telford, PA). Intravenous fluids
of Health, 1996). Approval of all animal care and use protocols
(lactated Ringer's solution) were administered per estab-
was obtained from the Medical University of South Carolina
lished weight-based protocols for maintenance fluids and
Institutional Animal Care and Use Committee (AR# 2786).
estimated blood loss replacement. A single-lumen catheter
March 2010 • Volume 110 • Number 3

Plasmin Activity and Tranexamic Acid
(8F) was placed into the right external jugular vein for fluid
over 5 min, and the mobile phase consisted of 10% aceto-
and drug administration. An arterial line catheter (7F) was
nitrile in 2 mM ammonium acetate (pH 3.5) with a flow rate
placed into the right carotid artery to continuously monitor
of 0.15 mL/min. The mass spectrometer was operated in
systemic blood pressures and obtain blood samples. After a
positive ion mode with a capillary voltage of 3.1 kV, source
60-min baseline and stabilization period, each pig was
temperature of 120°C, desolvation temperature of 400°C,
assigned to receive TXA (30 mg/kg, diluted into 50 mL
and nitrogen gas flow at 700 L/h. Data acquisition was
normal saline; Pharmacia & Upjohn, New York, NY) or
performed using MassLynx 4.1 and quantification using
vehicle (50 mL normal saline) over a 10-min period using a
QuanLynx 4.1 (Waters). TXA plasma concentrations were
prespecified randomization protocol. This anesthesia regi-
determined from precalibrated TXA standards (0.5– 40
men and surgical preparation provided a physiologically
and hemodynamically stable experimental model for up to6 h as previously reported.11
D-Dimer Measurementsd-dimer measurements were made on plasma collected at
Microdialysis Techniques
baseline (time 0) and 120-min time intervals for vehicle and
Microdialysis probes (CMA Microdialysis, North Chelms-
TXA treatment groups using an enzyme-linked immu-
ford, MA) with a molecular weight cutoff of 20 kDa and an
nosorbent assay (Cat. #602, American Diagnostics, Stam-
outer diameter of 0.5 mm were surgically placed interstitially
in the anterior myocardium of the left ventricle, right lobe ofthe liver, lower pole of the right kidney, and left quadriceps
muscle compartments. Placement of the microdialysis probes
Comparisons for baseline steady-state as well as for net
required a median sternotomy, a subxiphoid intraabdominal
change in fluorescence for all time points within each
incision, a subcostal flank incision, and a medial midthigh
region were made using an analysis of variance followed
incision with associated tissue dissections, respectively.
by pairwise tests of individual time points means using
The microdialysis probes were connected to precision
Bonferroni bounds. The net change in fluorescence com-
infusion pumps and controller system (BASi, West Lafayette,
pared with baseline for all time points within each region
IN). A flow rate of 6.0 L/min was established and an
was determined using a 2-sample t-test. Comparisons of
isoosmotic dialysis was performed. Dialysate was infused for
d-dimer concentrations at baseline (time 0) and 120-min
30 min to allow for equilibration with each of the respective
intervals were performed using a 2-sample t-test. All statisti-
tissue compartments. The microdialysate infusion contained
cal procedures were performed using STATA statistical soft-
the validated fluorogenic peptide (10 M, Cat. #A8171,
ware (Intercooled STATA 8.0, StataCorp, College Station, TX).
Sigma-Aldrich). Preliminary studies demonstrated that this
Results are presented as mean ⫾ sem with P values ⬍0.05
microdialysate concentration yielded a steady-state fluores-
considered to be statistically significant.
cence emission within 30 min of the initiation of dialysis,indicative of equilibration with the interstitial space of the
target tissue. The fluorescence emission of the interstitial
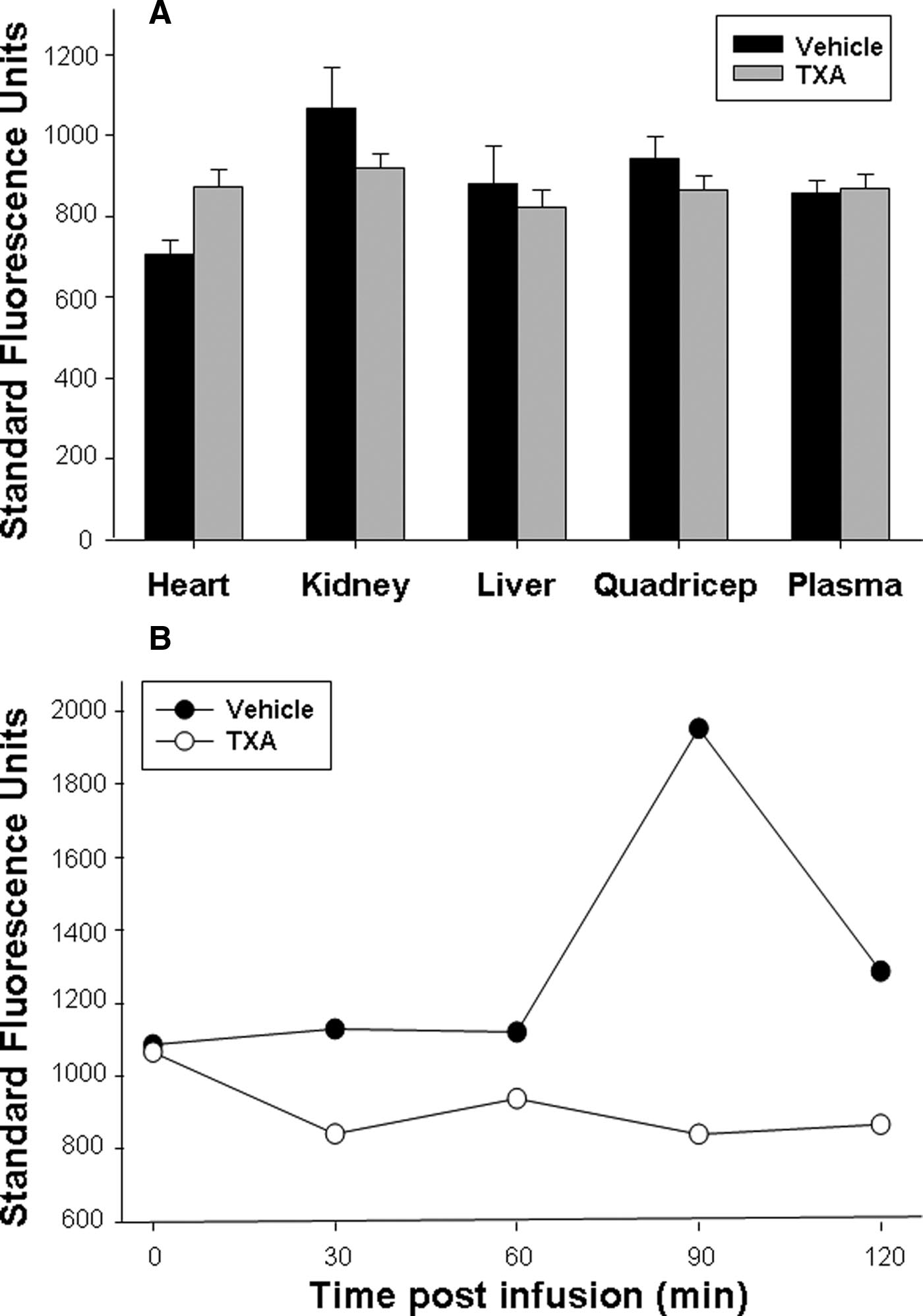
After successful placement of microdialysis probes in all
fluid collected from each of the microdialysis probes, which
tissue compartments, respective steady-state baseline fluores-
directly reflected PLact, was determined at steady-state
cence emission measurements, reflective of PLact within each
baseline and 30, 60, 90, and 120 min after TXA/vehicle
compartment, were obtained (Fig. 2A). There was no signifi-
infusion, using fluorescence measurement techniques as
cant difference in baseline fluorescence emissions between
groups, randomized to either vehicle or TXA treatment, foreach tissue compartment, reflective of equivalent PLact before
initiation of treatment. Figure 2B illustrates the representative
Arterial blood samples (50 mL) were collected immediately
fluorescence emission for a selected tissue compartment (i.e.,
after a 30-min stabilization period. The plasma from these
the liver) for both a representative vehicle and TXA pig
blood samples was used to develop a reference normal
preparation. Respective fluorescence emission measurements
porcine plasma solution for in vitro validations previously
were obtained at baseline (time 0) and 30, 60, 90, and 120 min
described. At baselines and at 30-min intervals throughout the
after either vehicle (saline) or TXA (30 mg/kg) infusion. The
protocol, coinciding with the microdialysis samples, arterial
differences in fluorescence emission values between the ve-
blood samples (10 mL) were collected. All blood samples
hicle and TXA groups at each of the respective time intervals
were collected in EDTA tubes, centrifuged, and the plasma
are reflective of changes in PLact induced by the administra-
was decanted and frozen for subsequent measurement of
tion of TXA. Therefore, to directly examine the effects of TXA
PLact using the previously described fluorescence measure-
on PLact, the absolute fluorescence emission values were
ment system.
transformed to yield a net change in mean fluorescenceemission with respect to mean vehicle values for each of the
TXA Plasma Concentration Measurements
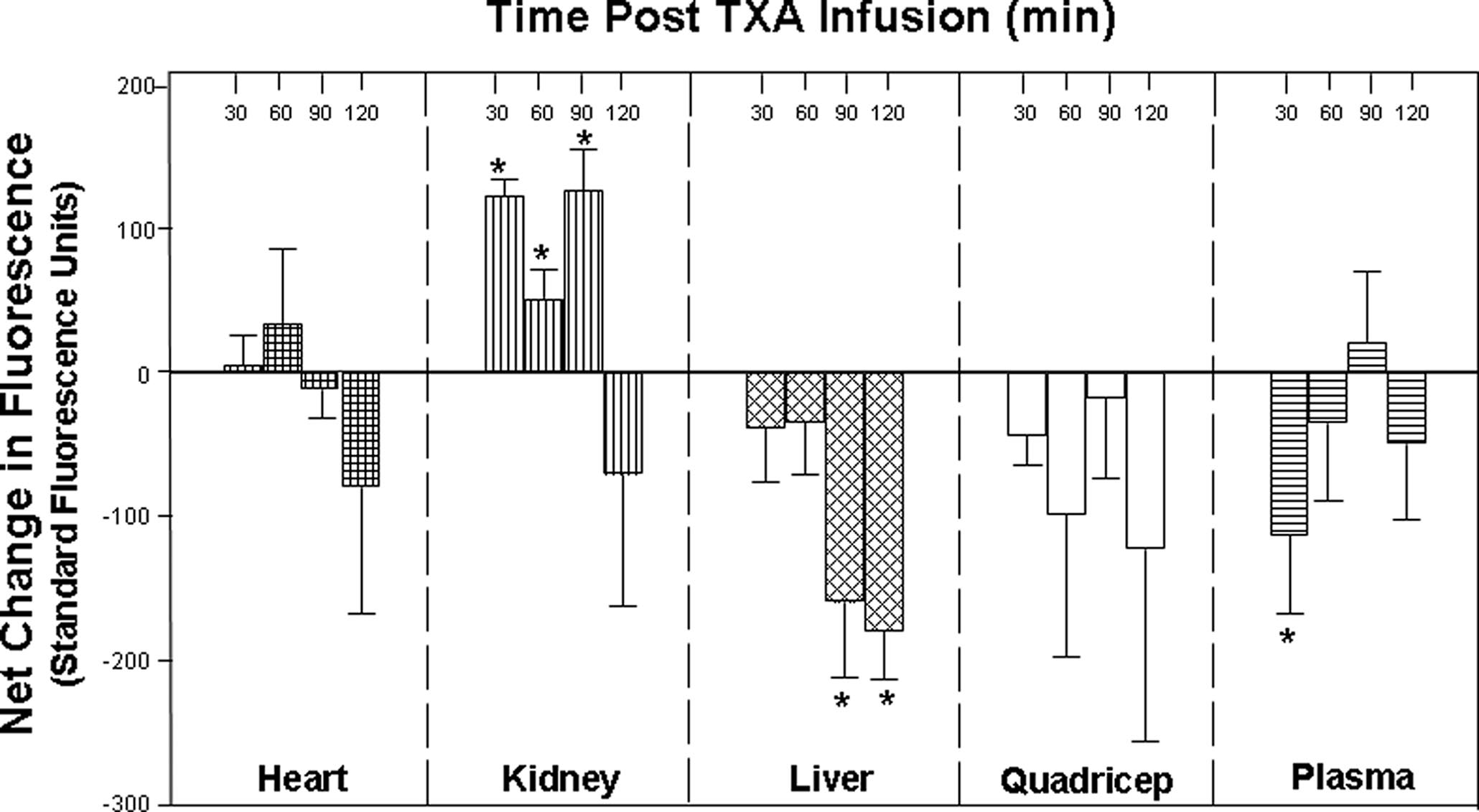
selected compartments at the specified time intervals (Fig. 3).
An Acquity UPLC coupled to a Quattro Premier XE mass
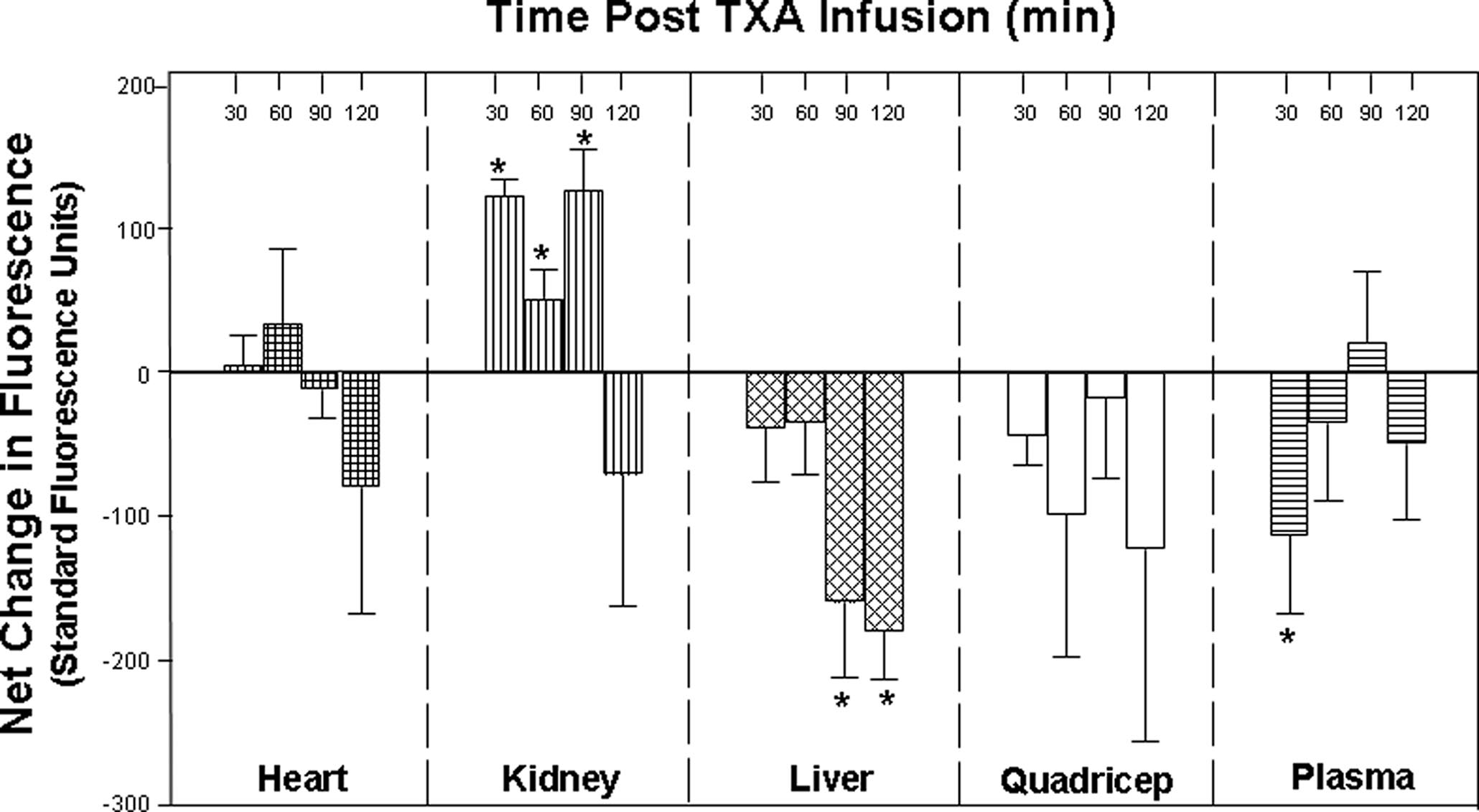
Compared with vehicle values, TXA significantly reduced
spectrometer (Waters, Milford, MA) was used to measure
plasma PLact at 30 min after infusion. However, in the
TXA plasma concentrations. Chromatographic separation
interstitial compartments, temporal and regional differences
was performed on an Acquity UPLC HSS C18 2.1 ⫻ 100
in PLact were observed after TXA administration. Specifically,
mm (1.8 m) column preceded by an Acquity UPLC HSS
there was a significant decrease in liver PLact at 90 and 120
C18 (1.8 m) precolumn. Samples were eluted isocratically
min, which occurred 60 min after the maximal decrease in
ANESTHESIA & ANALGESIA

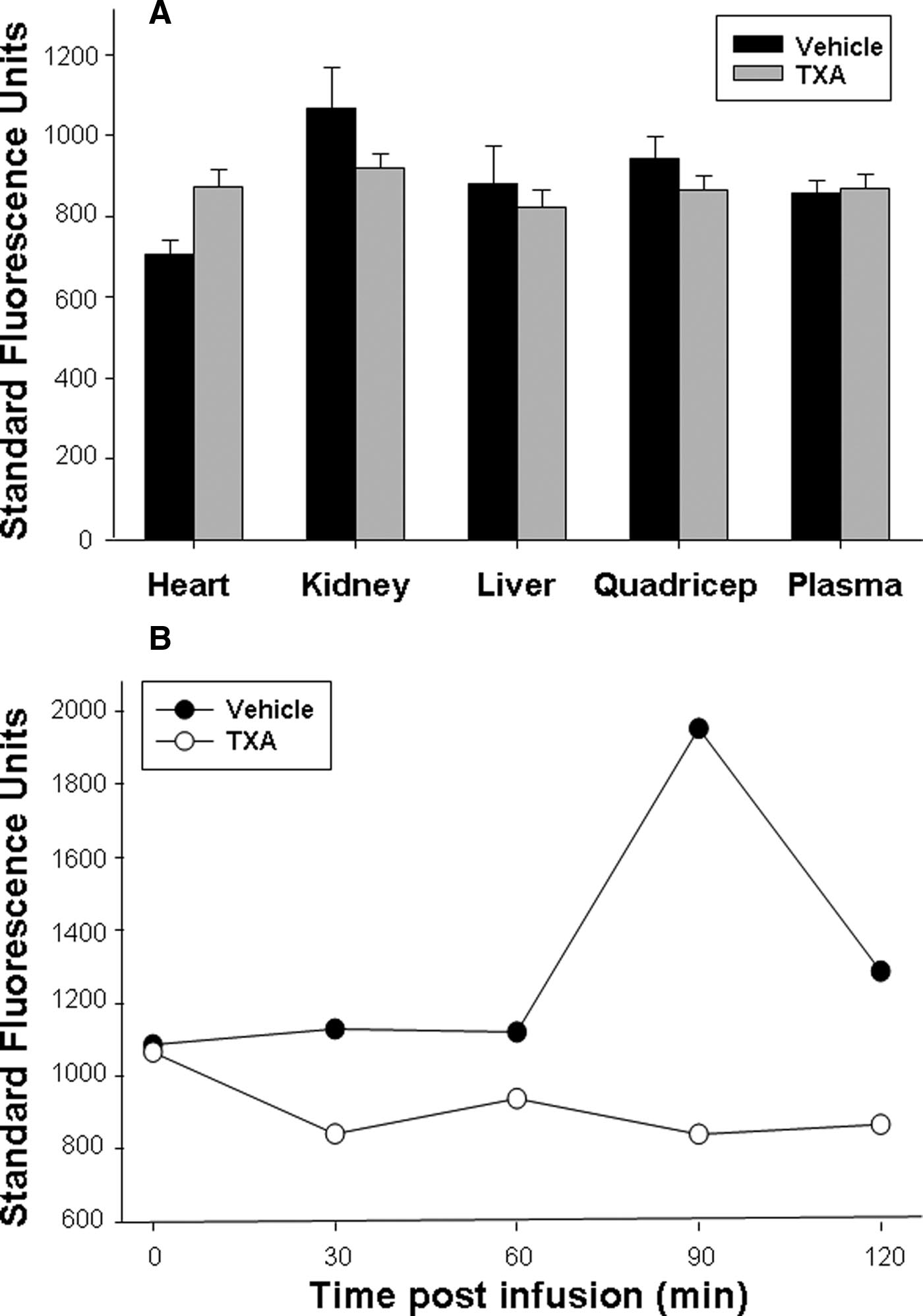
Figure 2. A, Steady-state baseline fluo-rescence emission, reflective of plasminactivity (PLact), within each of the targettissue compartments was equivalent inpigs randomized to either vehicle (saline)or tranexamic acid (TXA) (30 mg/kg).
Thus, the baseline fluorescence emis-sions between the 2 groups was compa-rable before initiation of treatment (plot-ted values are mean ⫾ SEM, *P ⬍ 0.05).
B, Representative fluorescence emissionmeasurements within the liver tissuecompartment were obtained at baseline(time 0) and 30, 60, 90, and 120 minafter either vehicle (saline) or TXA (30mg/kg) infusion. There was a notableincrease in absolute fluorescence emis-sion over time after vehicle (saline) infu-sion. In contrast, there was an overalldecrease in fluorescence emission overtime, reflective of reduced PLact withinthe liver after TXA administration. Thesummary data reflective of PLact acrosseach target compartment and all timeintervals are shown in Figure 3.
plasma PLact. In contrast, kidney PLact was significantly
at randomization (P ⫽ 0.67). The plasma d-dimer concentra-
increased at 30, 60, and 90 min. Within the myocardium, PLact
tion at 120 min after infusion decreased slightly, but not
remained virtually unchanged. In the quadriceps muscle,
significantly, from baseline (13 ⫾ 3 g/mL, P ⫽ 0.49) with no
PLact decreased after TXA infusion but did not reach statis-
difference between vehicle or TXA (P ⫽ 0.77).
tical significance at any time point (P ⬎ 0.5).
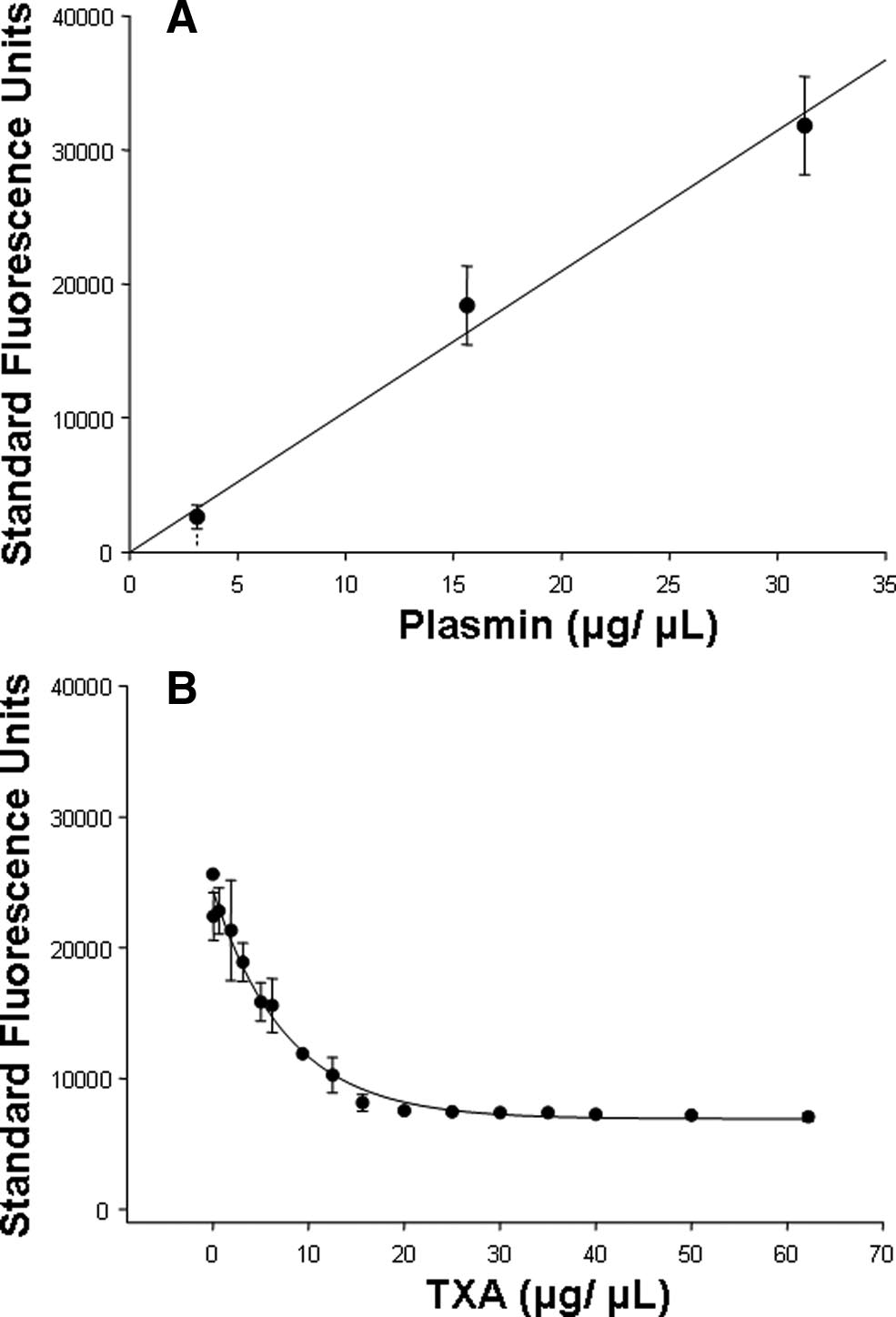
The TXA plasma concentrations for time intervals 30, 60,
90, and 120 min after TXA infusion are shown in Figure 4.
Perioperative hemorrhage is an important risk factor for
The peak TXA plasma concentration occurred at 30 min after
morbidity and mortality in most major surgical procedures,
TXA infusion and subsequently decreased in a negative
notably cardiovascular surgery.14–17 Accordingly, blood
logarithmic time-dependent manner consistent with first-
transfusions, blood product and coagulation factor deliv-
order elimination pharmacokinetics.13 Plasma from baseline
ery, as well as pharmacological modalities targeted at the
(time 0) and 120-min time intervals for vehicle and TXA
coagulation/fibrinolytic mechanisms are important clinical
treatment groups was subjected to d-dimer analysis. The
maneuvers in the perioperative setting.3,14 However, these
baseline, steady-state plasma d-dimer concentration was 20 ⫾
interventional strategies, such as pharmacological ap-
8 g/mL with no difference between vehicle and TXA groups
proaches, can be associated with adverse outcomes, which
March 2010 • Volume 110 • Number 3

Plasmin Activity and Tranexamic Acid
Figure 3. The computed net change in mean fluorescence emission, reflective of changes in plasmin activity (PLact), with respect totime-matched vehicle values after tranexamic acid (TXA) (30 mg/kg) infusion for selected compartments demonstrates the unique temporaland regional differences in the effects of TXA on PLact. Specifically, TXA significantly reduced plasma PLact at 30 min. In addition, there wasa significant decrease in liver PLact at 90 and 120 min. In contrast, kidney PLact was significantly increased at 30, 60, and 90 min. There wasno significant change in heart PLact for all time points. The PLact within the quadriceps muscle decreased after TXA infusion but did not reachstatistical significance at any time point (plotted values are mean ⫾ SEM, *P ⬍ 0.05 versus baseline).
Figure 4. Tranexamic acid (TXA) plasmaconcentrations
performance liquid chromatography/ massspectrometry
time intervals 30, 60, 90, and 120 minafter TXA infusion decreased in a negativelogarithmic time-dependent manner consis-tent with first-order elimination pharmacoki-netics13 (plotted values are mean ⫾ SEM,regression, y(x) ⫽ 219.37 ⫻ e⫺0.019 ⫻ x,r2 ⫽ 0.994, P ⫽ 0.003).
may be attributable to differences in dosing regimens as
fluorogenic-microdialysis approach in a large animal model,
well as off-target effects.14–18 One frequently used antifibrino-
to provide serial assessment of PLact on a regional basis, after
lytic is TXA, which can modulate the fibrinolytic pathway by
a standardized dose of TXA.9 The unique finding from this
inhibiting local PLact.19 However, current TXA dosing sched-
study is that interstitial PLact is differentially affected after
ules are largely empirical, and the regional and temporal
TXA infusion in both a region- and time-dependent manner.
effects with respect to changes in PLact remain unknown.8
For example, TXA induced temporally distinct PLact profiles
This study addressed this issue through the use of a validated
within the plasma and selected interstitial compartments such
ANESTHESIA & ANALGESIA
as the kidney and the liver. These temporal and regional
respect to PLact profiles was 2-fold. First, the objective of this
differences in the effects of TXA on PLact may have important
study was to demonstrate the proof of concept that there is
therapeutic considerations when managing fibrinolysis in the
regional and temporal heterogeneity regarding 1 computed
perioperative period. The prophylactic use of lysine analogue
dose of an antifibrinolytic, and TXA was chosen as a proto-
antifibrinolytics during cardiac surgery has the potential to
typical example. Second, the serine protease inhibitor, aproti-
induce a hypercoagulable prethrombotic state.20 As such,
nin, although historically considered the first-line drug for
thrombosis (deep vein, pulmonary artery, renal pelvic and
modulating PLact, has been withdrawn from clinical use, thus
artery, bladder, and cerebral vascular) with respective con-
leaving lysine analogues such as TXA as the pharmacological
comitant organ injury and dysfunction have been associated
mainstay for antifibrinolytic therapy. Lysine analogues such
with the use of antifibrinolytics such as TXA.17,21–26 The
as TXA affect PLact primarily by inhibiting the enzymatic
primary mechanism of elimination of TXA is via renal excre-
interaction of plasminogen and plasmin with fibrinogen and
tion. As such, acute temporal alterations in renal function
fibrin, which is key to the enzymatic induction of fibrinoly-
associated with cardiac surgery further compound the com-
sis.19 Thus, TXA served as a reasonable first step, with
plexity of maintaining a safe hemostatic state in such clinical
respect to clinical relevance, in determining the fundamen-
scenarios in which TXA is indicated.27 Thus, there are several
tal mechanistic underpinnings of the regional and temporal
temporal and regional variables that must be considered
effects of lysine analogues on PLact profiles. Comparative
when attempting to balance the extensively dynamic and
studies of specific antifibrinolytic drugs hold significant
sensitive coagulation/fibrinolytic state(s) of cardiac surgical
clinical relevance and warrant future investigation. Never-
patients in the perioperative period.
theless, it is likely that the results from this study can be
Although the pharmacology of TXA has been rigorously
extrapolated to some degree to other lysine analogues (i.e.,
described regarding mechanisms of action,19 there have
⑀-aminocaproic acid) as well as aprotinin, with respect to
been no studies that have precisely quantified the effects of
the regional and temporal heterogeneity observed. For
TXA on interstitial PLact in vivo, the primary target for TXA
example, after a single bolus dose of TXA, transient effects
with respect to modulating fibrinolysis. Tissue plasminogen
on PLact were observed in the heart and kidney, whereas
activator is synthesized and secreted by endothelial cells
there were persistent effects in the liver. Although this
intraluminally and abluminally into the vascular and intersti-
acute study could not address this issue directly, the
tial spaces, respectively, where it catalyzes the conversion of
disparate effects on PLact may in turn affect hepatic and
plasminogen to plasmin and thus facilitates fibrinolysis.28
renal function, the latter of which has been identified as
This microdialysis approach provides for interstitial
a potential risk factor for the adverse effects of antifi-
interrogation of PLact and thus a means to directly measure
brinolytics such as aprotinin.17,18,29
a key determinant of fibrinolysis and avoids the interfer-
The peak TXA plasma concentrations obtained in this
ence of intraluminal dynamics. Furthermore, although past
study are consistent with those typically reported in prior
basic and clinical studies have described the utility of TXA
clinical investigations.8,31,32 As such, the TXA dosing regimen
in the context of cardiovascular surgery, such as that
used in this study is a clinically relevant dosing approach. The
associated with cardiopulmonary bypass, optimal dosing
TXA plasma elimination profile obtained is congruent with
strategies remain a subject of debate.8 This is the first study
classic first-order pharmacokinetics,13 indicating that the large
in which an approach was developed to continuously
animal model used in this study holds pharmacological
measure the major biological response variable relevant to
relevance. The time of the peak TXA plasma at 30 min
TXA administration, PLact, within the plasma as well as
coincides with the occurrence of peak plasma PLact inhibi-
interstitial space of critical target tissues. In this study, a
tion, demonstrating the pharmacological efficacy of the TXA
microdialysis approach was used to interrogate the interstitial
within the vascular compartment. Thus, the large animal
compartment, an approach that has been well described
preparation and TXA dosing paradigm used in this study are
previously in both animal and clinical studies.10,11 This mi-
likely to be a clinically relevant simulation.
crodialysis method was coupled with a fluorogenic substratespecific for plasmin and therefore provided a means to
Study Limitations and Conclusions
quantify PLact within the interstitial space. This methodology
One potential limitation of this study was that the TXA
may provide a useful analytical approach to assess PLact with
regimen implemented involved an initial loading dose only
varying TXA dosing regimens and thereby provide a basis for
without a subsequent continuous infusion of TXA. In
optimal TXA administration. This study provided the funda-
addition, the in vivo investigations did not include the
mental temporal and regional information necessary to move
context of cardiopulmonary bypass, which is a typical
forward with studies aimed at TXA dosing optimization.
clinical scenario in which TXA is frequently used. Our
Moreover, this study identified differences in PLact after TXA
primary objective was to quantify the regional and tempo-
administration in critical target organs such as the liver and
ral effects of TXA on relevant compartment PLact profiles.
kidney, which may hold relevance in the clinical context of
Accordingly, the TXA regimen involved an initial dose only
hepatic or renal dysfunction.17,18,29 The continuous PLact
to examine the compartment-specific temporal dynamics of
profiling, which is described in the current study, may pro-
TXA on PLact profiles, which would have been potentially
vide a means by which to address these issues and further
obscured by the subsequent administration of a continuous
optimize current and future antifibrinolytic therapies.30
infusion of TXA. Furthermore, the context of cardiopulmo-
In this study, TXA was used to investigate the effects of a
nary bypass would have included requisite systemic hepa-
frequently used antifibrinolytic drug on plasma and intersti-
rinization, which could have added coagulation interactions
tial PLact profiles. The rationale for focusing on TXA with
that potentially affected de novo fibrinolytic processes. Indeed,
March 2010 • Volume 110 • Number 3
Plasmin Activity and Tranexamic Acid
this study demonstrated that static measurements to quan-
7. Stensrud PE, Nuttal GA. Pharmacology of antifibrinolytic
tify fibrinolysis (i.e., d-dimers) were stable and not different
agents (chap 8). In: Housman PR, Nuttall GA, eds. Advances in
between vehicle and TXA groups. This suggests that the
Cardiovascular Pharmacology. Philadelphia, PA: LipincottWilliams & Wilkins, 2008:183–204
experimental design did not evoke a substantial fibrinolytic
8. Dowd NP, Karski JM, Cheng DC, Carroll JA, Lin Y, James RL,
response. Nevertheless, using a continuous interstitial
Butterworth J. Pharmacokinetics of tranexamic acid during
monitoring approach, this study demonstrated that there
cardiopulmonary bypass. Anesthesiology 2002;97:390 –9
was heterogeneity in steady-state PLact in specific tissue
9. Chauhan S, Bisoi A, Kumar N, Mittal D, Kale S, Kiran U,
compartments, which were differentially affected by TXA.
Venugopal P. Dose comparison of tranexamic acid in pediatriccardiac surgery. Asian Cardiovasc Thorac Ann 2004;12:121– 4
These observations suggest that continuous PLact monitor-
10. Spinale FG, Koval CN, Deschamps AM, Stroud RE, Ikonomidis
ing would be of much greater importance in the context of
JS. Dynamic changes in matrix metalloprotienase activity
a heightened fibrinolytic state such as cardiopulmonary
within the human myocardial interstitium during myocardial
bypass. The primary focus of this preliminary study was to
arrest and reperfusion. Circulation 2008;118:S16 –23
determine the fundamental mechanistic underpinnings of
11. Deschamps AM, Zavadzkas J, Murphy RL, Koval CN, McLean
the regional and temporal effects of TXA on PLact profiles
JE, Jeffords L, Saunders SM, Sheats NJ, Stroud RE, Spinale FG.
Interruption of endothelin signaling modifies membrane type
in a de novo, nonpathological, fibrinolytic state. Logically,
1 matrix metalloproteinase activity during ischemia and reper-
one may anticipate an even greater magnitude of effect by
fusion. Am J Physiol Heart Circ Physiol 2008;294:H875– 83
TXA in a pathological fibrinolytic state such as that induced
12. Smith RE, Bissell ER, Mitchell AR, Pearson KW. Direct photo-
by cardiopulmonary bypass. The extension of the current
metric or fluorometric assay of proteinases using substrates
findings will provide a basis for the pursuit of similar PLact
containing 7-amino-4-trifluoromethylcoumarin. Thromb Res
investigations involving a clinically relevant cardiopulmo-
1980;17:393– 402
13. Buxton ILO. Pharmacokinetics and pharmacodynamics: the dy-
nary bypass model. Nevertheless, this study demonstrated
namics of drug absorption, distribution, action, and elimination
in a clinically relevant large animal model that there is
(chap 1). In: Brunton LL, Lazo JS, Parker KL, eds. Goodman &
regional and temporal heterogeneity in PLact after a single
Gilman's The Pharmacological Basis of Therapeutics. 11th ed.
computed dose of TXA, a prototypical antifibrinolytic.
New York, NY: McGraw Hill. Available at: http://www.
Although TXA and similar antifibrinolytics are frequently
used, they are not approved by the Food and Drug Admin-
14. Nuttall GA, Brost BC, Connis RT, Gessner JS, Harrison CR,
istration for prophylactic use to reduce blood loss and
Miller RD, Nickinovich DG, Nussmeier NA, Rosenberg AD,
blood component transfusions in patients undergoing cor-
Spence R. Practice guidelines for perioperative blood transfu-
onary bypass surgery. Coupled with recent concerns for the
sion and adjuvant therapies. An updated report by the Ameri-
adverse effects of aprotinin, the findings of this study
can Society of Anesthesiologists Task Force on Perioperative
underscore the need for more rigorous monitoring and
Blood Transfusion and Adjuvant Therapies. Anesthesiology2006;105:198 –208
dosing of antifibrinolytics.
15. Marietta M, Facchini L, Pedrazzi P, Busani S, Torelli G. Patho-
physiology of bleeding in surgery. Transplant Proc 2006;38:812–4
16. Goodnough LT. Risks of blood transfusion. Anesthesiol Clin
The authors acknowledge the assistance of Danyelle M.
North America 2005;23:241–52
Townsend, PhD, and Joachim de Klerk Uys, PhD, of the Medical
17. Fraser IS, Porte RJ, Kouides PA, Lukes AS. A benefit-risk
University of South Carolina Hollings Cancer Center Drug Me-
review of systemic haemostatic agents: part 1: in major sur-
tabolism and Clinical Pharmacology Core Facility in the measure-
gery. Drug Saf 2008;31:217–30
ment of plasma tranexamic acid concentrations.
18. Fergusson DA, He´bert PC, Mazer CD, Fremes S, MacAdams C,
Murkin JM, Teoh K, Duke PC, Arellano R, Blajchman MA,Bussie res JS, Coˆte´ D, Karski J, Martineau R, Robblee JA, Rodger
M, Wells G, Clinch J, Pretorius R; BART Investigators. A
1. Laupacis A, Fergusson D. Drugs to minimize perioperative blood
comparison of aprotinin and lysine analogues in high-risk
loss in cardiac surgery: meta-analyses using perioperative blood
cardiac surgery. N Engl J Med 2008;358:2319 –31
transfusion as the outcome. Anesth Analg 1997;85:1258–67
19. Verstraete M. Clinical application of inhibitors of fibrinolysis.
2. Hardy JF, Be´lisle S. Natural and synthetic antifibrinolytics in
Drugs 1985;29:236 – 61
adult cardiac surgery: efficacy, effectiveness and efficiency.
20. Slaughter TF, Faghih F, Greenberg CS, Leslie JB, Sladen RN. The
Can J Anaesth 1994;41:1104 –12
effects of epsilon-aminocaproic acid on fibrinolysis and thrombin
3. Society of Thoracic Surgeons Blood Conservation Guideline
generation during cardiac surgery. Anesth Analg 1997;85:1221–6
Task Force, Ferraris VA, Ferraris SP, Saha SP, Hessel EA II,
21. Mutter WP, Stillman IE, Dahl NK. Thrombotic microangiopa-
Haan CK, Royston BD, Bridges CR, Higgins RS, Despotis G,
thy and renal failure exacerbated by epsilon-aminocaproic
Brown JR; Society of Cardiovascular Anesthesiologists Special
acid. Am J Kidney Dis 2009;53:346 –50
Task Force on Blood Transfusion, Spiess BD, Shore-Lesserson
22. Wymenga LF, van der Boon WJ. Obstruction of the renal pelvis
L, Stafford-Smith M, Mazer CD, Bennett-Guerrero E, Hill SE,Body S. Perioperative blood transfusion and blood conserva-
due to aninsoluble blood clot after epsilon-aminocaproic acid
tion in cardiac surgery: the Society of Thoracic Surgeons and
therapy: resolution with intraureteral streptokinase instilla-
The Society of Cardiovascular Anesthesiologists clinical prac-
tions. J Urol 1998;159:490 –2
tice guideline. Ann Thorac Surg 2007;83:S27– 86
23. Hocker JR, Saving KL. Fatal aortic thrombosis in a neonate
4. Molenaar IQ, Warnaar N, Groen H, Tenvergert EM, Slooff MJ,
during infusion of epsilon-aminocaproic acid. J Pediatr Surg
Porte RJ. Efficacy and safety of antifibrinolytic drugs in liver
1995;30:1490 –2
transplantation: a systematic review and meta-analysis. Am J
24. Dentz ME, Slaughter TF, Mark JB. Early thrombus formation on
heparin-bonded pulmonary artery catheters in patients receiving
5. Gill JB, Chin Y, Levin A, Feng D. The use of antifibrinolytic
epsilon aminocaproic acid. Anesthesiology 1995;82:583–6
agents in spine surgery. A meta-analysis. J Bone Joint Surg Am
25. Hoffman EP, Koo AH. Cerebral thrombosis associated with
2008;90:2399 – 407
Amicar therapy. Radiology 1979;131:687–9
6. Coats T, Roberts I, Shakur H. Antifibrinolytic drugs for acute
26. Seymour BD, Rubinger M. Rhabdomyolysis induced by
traumatic injury. Cochrane Database Syst Rev 2004;4:CD004896
epsilon-aminocaproic acid. Ann Pharmacother 1997;31:56 – 8
ANESTHESIA & ANALGESIA
27. Shaw A, Swaminathan M, Stafford-Smith M. Cardiac surgery-
30. Dietrich W, Nicklisch S, Koster A, Spannagl M, Giersiefen H,
associated acute kidney injury: putting together the pieces of
van de Locht A. CU-2010: a novel small molecule protease
the puzzle. Nephron Physiol 2008;109:55– 60
inhibitor with antifibrinolytic and anticoagulant properties.
28. Roelofs JJ, Rouschop KM, Leemans JC, Claessen N, de Boer
AM, Frederiks WM, Lijnen HR, Weening JJ, Florquin S. Tissue-
31. Fiechtner BK, Nuttall GA, Johnson ME, Dong Y, Sujirattanawi-
type plasminogen activator modulates inflammatory re-
mol N, Oliver WC Jr, Sarpal RS, Oyen LJ, Ereth MH. Plasma
sponses and renal function in ischemia reperfusion injury.
tranexamic acid concentrations during cardiopulmonary by-
J Am Soc Nephrol 2006;17:131– 40
pass. Anesth Analg 2001;92:1131– 6
29. Kincaid EH, Ashburn DA, Hoyle JR, Reichert MG, Hammon
32. Nuttall GA, Gutierrez MC, Dewey JD, Johnson ME, Oyen LJ,
JW, Kon ND. Does the combination of aprotinin and
Hanson AC, Oliver WC Jr. A preliminary study of a new
angiotensin-converting enzyme inhibitor cause renal failureafter cardiac surgery? Ann Thorac Surg 2005;80:1388 –93; dis-
tranexamic acid dosing schedule for cardiac surgery. J Cardio-
thorac Vasc Anesth 2008;22:230 –5
March 2010 • Volume 110 • Number 3
Source: http://www.microvide.com/uploads/Reust-TXA.pdf
Inter national Organization for Succulent Plant Study para el Estudio de Plantas Suculentas de Recherche sur les Plantes Succulentes Inter nationale Organisation A short history of Repertorium Plantarum Succulentarum The first issue of Repertorium Plantarum Succulentarum (RPS) was produced in 1951 byMichael Roan (1909−2003), one of the founder members of the International Organizationfor Succulent Plant Study (IOS) in 1950. It listed the ‘majority of the new names [ofsucculent plants] published the previous year'. The first issue, edited by Roan himself withthe help of A.J.A Uitewaal (1899−1963), was published for IOS by the National Cactus &Succulent Society, and the next four (with Gordon Rowley as Associate and later JointEditor) by Roan's newly formed British Section of the IOS. For issues 5−12, GordonRowley became the sole editor. Issue 6 was published by IOS with assistance by theAcclimatisation Garden Pinya de Rosa, Costa Brava, Spain, owned by Fernando Riviere deCaralt, another founder member of IOS.
Bid No: 2013-145-00-00-SMA Buyer: Sandra Montalvo Tel. No: (956) 318-2626 ext 4865 REQUEST FOR BIDS Hidalgo County Sheriff's Office "Legend & Non-Legend Pharmaceuticals BID OPENING DATE: _2013 @ 9:30 a.m. Contact Person: Martha L. Salazar, CPPB, Purchasing Agent Hidalgo County Purchasing Department Physical Address: 2802 S. Business Hwy. 281 -New Administration Building Mailing/Postal Address: 2812 S. Business Hwy. 281 Edinburg, Texas 78539 956 318-2626