Untitled
Blinded, Randomized, Quantitative Grading
Comparison of Minimally Invasive, Fractional
Radiofrequency and Surgical Face-lift
to Treat Skin Laxity
Macrene Alexiades-Armenakas, MD, PhD; David Rosenberg, MD;Bradley Renton, PhD; Jeffrey Dover, MD; Kenneth Arndt, MD
Objectives: To quantify the improvements in laxity from
gical face-lift. Patient satisfaction was high (dissatisfied, 0%;
the surgical face-lift and to perform a randomized, blinded
neutral, 7%; satisfied, 60%; and very satisfied, 33%). All par-
comparison with the clinical effects of a novel, mini-
ticipants in the FRF treatment group experienced transient
mally invasive fractional radiofrequency (FRF) system.
erythema, mild edema, and mild to moderate purpura thatresolved in 5 to 10 days, and they returned to normal activi-
Study Design: Randomized, blinded, comparative trial.
ties within 24 hours. There were no adverse events or com-plications in the FRF group. All patients in the surgical face-
Patients: Fifteen sequential patients with facial skin lax-
ity enrolled in the trial and completed FRF treatment and
edema, and ecchymosis, and they returned to normal activi-
follow-up. Baseline and follow-up digital photographs of
ties on suture removal at 7 to 10 days.
patients undergoing FRF were randomly mixed with 6 setsof baseline and follow-up images of patients undergoing
Conclusions: This randomized, blinded, quantitative as-
surgical face-lift with equivalent baseline facial laxity grades.
sessment using a validated grading scale of skin laxity im-provement from the gold standard treatment, the surgical
Main Outcome Measures: Five independent blinded
face-lift, and comparative analysis to a novel, minimally
evaluators graded randomized baseline and 3- to 6-month
invasive FRF treatment has demonstrated 49% improve-
follow-up photographs using a comprehensive quanti-
ment in skin laxity relative to baseline for the surgical face-
tative 4-point laxity grading scale. Quantitative changes
lift, compared with 16% for FRF. The surgical face-lift re-
in laxity grades were calculated and compared statisti-
sulted in a mean 1.20-grade improvement on the 4-point
cally for FRF treatment vs surgical face-lifts. Patient sat-
laxity grading scale. In comparison, a single, minimally in-
isfaction and adverse events were also evaluated.
vasive FRF treatment demonstrated a 0.44–laxity grade im-
Results: Blinded grading of unmarked, randomized base-
provement, or 37% that of the surgical face-lift, without the
line and follow-up photographs of patients undergoing FRF
adverse effects and complications of surgical procedures.
treatment randomized with baseline and follow-up photo-
This study provides a basis for quantifying cosmetic out-
graphs of patients undergoing surgical face-lift demonstrated
comes from novel treatments with comparative analysis to
statistically significant improvement in facial laxity, with a
the gold standard. It also suggests that minimally invasive
mean grade improvement of 1.20 for patients in the surgi-
FRF treatment may provide an important nonsurgical op-
cal face-lift group and of 0.44 for FRF-treated patients on a
tion for the treatment of facial skin laxity.
4-point laxity grading scale (
P⬍.001). The improvements
Trial Registration: clinicaltrials.gov Identifier:
relative to baseline were 16% for FRF treatment compared
with 49% for the surgical face-lift. The mean laxity improve-ment from a single FRF treatment was 37% that of the sur-
Arch Dermatol. 2010;146(4):396-405
rized as intrinsic aging, ow-
the treatment of laxity associated with in-
ing to genetic factors and
trinsic aging. Nonsurgical devices have
characterized by laxity and
been used to treat rhytids and laxity be-
deep rhytids, and photoag-
cause patients are willing to trade the
ing, owing to ultraviolet damage and char-
greater cosmetic improvement obtained
acterized by dyschromia, elastosis, fine
from surgical treatment for the minimal
rhytids, erythema, telangiectasia, tex-
risk and rapid recovery associated with the
tural changes, and keratoses.1 Laser, light,
former.2 To date, however, the level and
and radiofrequency (RF) energy sources
consistency of outcomes from laser and en-
Author Affiliations are listed at
have succeeded in treating the second cat-
ergy-based technologies have not been
the end of this article.
egory of skin aging; however, the surgi-
comparable to surgical face-lift results, nor,
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
to our knowledge, has a valid comparative study to the
gold standard of surgical face-lifts ever been conducted.
The Miratone minimally invasive bipolar fractional RF
(FRF) system (Primaeva Medical, Inc, Pleasanton, Cali-fornia) heats the dermis from within using a mi-
The FRF treatments were performed by the lead author (M.A.-A.)
croneedle electrode array.3 The microneedle electrodes
using a study protocol approved by an institutional review board.
are arranged in pairs between which bipolar RF energy
Inclusion criteria were being older than 18 years, in good health,
is delivered. Thermal lesions are fractionally generated
and with mild to severe facial rhytids or laxity (minimum baseline
directly within the reticular dermis. The volume of each
laxity, grade 2). Exclusion criteria consisted of history of injection
lesion is defined by the geometry of the microneedle elec-
with silicone, fat, collagen, or a synthetic material in the intendedtreatment area, bleeding disorder, hypertrophic scar or keloid for-
trode pairs. Real-time feedback of lesion temperature from
mation, isotretinoin treatment in the past 12 months, anaphylaxis,
sensors in the tips of the microneedle electrodes allows
energy delivery to be precisely modulated so that le-
current, or anticipated treatment with anticoagulants; thrombo-
sions are created at a specific preselected temperature and
lytics; chemotherapeutics; systemic corticosteroids; or anabolic ste-
for defined time periods. The fractional pattern of in-
jury, wound healing, and dermal remodeling processes
healing (eg, patients with diabetes mellitus), collagen vascular dis-
induced following treatment were recently described his-
ease, an implantable electronic device (eg, pacemaker), or active
tologically in skin to be excised in subsequent abdomi-
infection were also excluded. Participants were required to be avail-
noplasty or face-lift procedures.3,4 Fractional thermal in-
able for posttreatment follow-up evaluation.
jury of deep dermal collagen induced a vigorous woundhealing process leading to dermal remodeling and the gen-
FRF Treatment Protocol
eration of new collagen, elastin, and hyaluronic acid, sug-gesting the device could become an effective treatment
Patients undergoing FRF received fixed-temperature symmetri-
option with predictable outcomes for the treatment of lax-
cal treatment of the lateral mid and lower face with the Mira-
ity and rhytids associated with intrinsic aging. To date,
tone system. The FRF energy was delivered through 5 mi-
there remain no published reports quantifying the lax-
croneedle electrode pairs deployed in the reticular dermis atan angle of 20° to the skin surface, with the exposed electrode
ity improvements from the gold standard treatment, the
length extending from 0.75 to 2 mm below the skin surface
surgical face-lift, or comparatively analyzing the clini-
(
Figure 1). The precise intradermal location of the electrode
cal outcome of noninvasive or minimally invasive non-
tips was determined by real-time impedance measurements, such
surgical treatment of skin laxity with surgical face-lift out-
that impedance measurements between 300 and 2000 ⍀ were
comes. In prior studies evaluating outcomes from surgical
used to define ideal intradermal placement.3 Typical dermal im-
face-lifts, descriptive impressions were used, including
pedance measurements were between 500 and 1500 ⍀. Soft-
"poor, good, or excellent."5-7 In contrast, the present study
ware built into the device precluded energy delivery if imped-
is the first to use quantitative, blinded evaluations with a
ance between an electrode pair measured less than 300 or more
tested laxity grading scale. In this investigational study, we
than 3000 ⍀, thereby restricting energy delivery to proper in-
evaluate the clinical effects of FRF for the treatment of fa-
tradermally placed electrodes.3 Software was also pro-grammed to deliver energy until a preselected intradermal tar-
cial laxity and compare the outcomes with surgical face-
get temperature was attained and for a specified duration in
lift results through randomized, blinded assessment of digi-
seconds (
Figure 2). Epidermal cooling was achieved by po-
tal baseline and follow-up clinical photography.
sitioning a cooling device maintained at a temperature of 15°Cdirectly on the skin above the exposed electrode length. Thespacing of the bipolar needle pairs and the spacing during suc-
cessive applications of the device were selected to give 15% to35% fractional skin coverage by surface projection. Patients 1
The study protocol was approved by the Western Institutional
through 5 received topical anesthesia (EMLA cream; APP Phar-
Review Board. All participants provided verbal and written con-
maceuticals, LLC, Schaumburg, Illinois) only, applied for 45
sent before enrollment. Patient consent for digital photography
to 60 minutes before treatment. Conservative treatment para-
was also obtained before treatment. Randomized (not paired in
meters of 62°C and 3 seconds were selected for these patients.
sequence) digital baseline and 3- to 6-month follow-up images
Patients 6 through 15 received additional local infiltration with
of 15 sequential patients completing FRF treatment and fol-
diluted lidocaine (0.25% with 1:400 000 epinephrine). A local
low-up were intermixed with 6 sets of randomized baseline and
anesthetic (mean quantity, 18 mL of 0.25% lidocaine) was used
3- to 6-month follow-up images of surgical face-lift patients with
in both cheeks and in the submental and lateral neck regions.
equivalent baseline facial laxity, selected from a surgical face-lift
For these patients, more aggressive treatment parameters of 68°C
pool by one of us, a plastic surgeon (D.R.). The FRF treatment
to 78°C and 5 seconds were selected. A representative real-
and surgical face-lift photographs were equivalently cropped and
time temperature curve for a preselected target temperature of
randomly intermixed. Pretreatment and posttreatment photo-
70°C for 5 seconds is shown in Figure 2. Before treatment, the
graphs were not in sequence, but randomly assorted throughout
patient's skin was cleansed with Betadine (Purdue Pharma, Stam-
the intermixed FRF and surgical photographs. Blinded grading
ford, Connecticut), and treatments were delivered medial to
was performed by 5 independent evaluators (J.D., K.A., and 3 oth-
lateral in rows following anatomical margins. Postoperatively,
ers), including dermatologists and plastic surgeons, who were un-
the patient's skin was cleansed with isotonic sodium chloride
aware of the nature or types of treatments being tested, using a
solution, and a thin coat of white petrolatum was applied. Pa-
quantitative 4-point grading scale assessing changes in skin lax-
tients were allowed to resume normal activities immediately
ity.8-10 The blinded evaluators were unaware that surgical face-
and were instructed to wash the skin with mild cleansers, to
lift photographs were included in this study, nor were they privy
avoid makeup for 24 hours, and to minimize sun exposure for
to the type of nonsurgical treatment being tested.
14 days. Patients were required to report any discomfort, ad-
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.


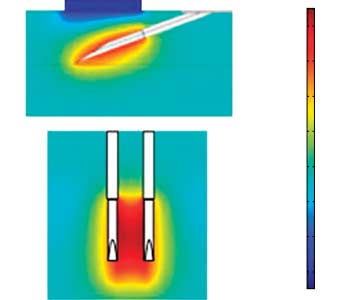
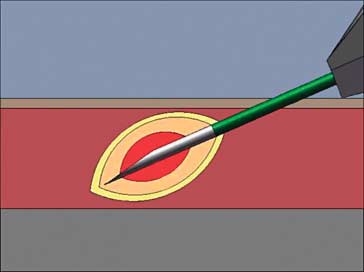
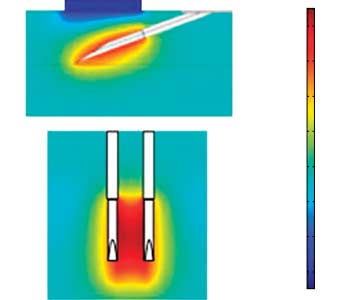
Figure 1. Schematic of the fractional radiofrequency (FRF) handpiece, energy delivery, real-time temperature feedback, and time-at-temperature control. The FRF
handpiece consists of 5 paired electrodes that are insulated, except for the distal tips extending from 0.75 to 2 mm beneath the skin surface, thereby assuring dermal
energy delivery and protection of the superficial dermis and epidermis (A). The 32-gauge electrode tips are inserted into the dermis at a 20º angle (B). Temperature
sensors are built into each electrode pair (C), thereby providing accurate real-time temperature readings, as opposed to mathematical modeling, as in prior modalities.
Software is programmed to emit energy until preselected target temperatures (eg, 70ºC) are attained and to maintain temperature for a desired duration (eg, 5 seconds);
parameters are selected for optimal collagen denaturation (D).
verse effects, and complications during or following treatment
crosses. The cheek flap was closed by suturing the superficial
and completed questionnaires at each follow-up visit. Patients
muscular aponeurotic system flap to the preauricular tissue
were followed up at 1, 3, and 6 months following treatment.
and anchoring the flap posteriorly, just anterior to the tragus.
During 3- and 6-month follow-up visits, patients were asked
The platysmal flap, beginning at the mandibular angle, was
to rate their overall satisfaction and their impression of wrinkles
sutured to the mastoid periosteum. Redundant preauricular
and laxity improvement using a 5-point scale.
tissue was excised. Excision and closure of the skin flap com-menced at the apex of the postauricular incision, followed by
SURGICAL FACE-LIFT PROCEDURE
skin excision and closure anteriorly and posteriorly. The post-auricular, hair-bearing region and temporal incision were
Surgical face-lifts were performed by one of us (D.R.). Each
closed superficially with staples and sutures. A compression
patient received general endotracheal and local anesthesia.
head dressing was placed and secured with burn netting.
The procedure consisted of submentoplasty, suction and exci-
Patients received treatment overnight by a registered nurse,
sional lipectomy, and deep-plane plication. The incision and
were instructed about wound care, and had sutures removed
dissection extended from the malar eminence and mandibular
7 to 10 days posttreatment.
angle into the neck in the preplatysmal plane to the midlineand submental incision. The deep-plane dissection extended
QUANTITATIVE LAXITY GRADING,
deep to the jowl fat and inferiorly to 2 cm below the mandibu-
ASSESSMENTS, AND STATISTICAL ANALYSIS
lar angle and continued anteriorly within the fibroadipose tis-sues of the melolabial fold and deep to the superficial muscu-
Standardized photographs were taken for the FRF patient
lar aponeurotic system of the jowl. The melolabial fold was
group at baseline on the day of treatment and during each
approached by undermining the fibroadipose layer of the
follow-up visit. Standardized photographs were taken for the
cheek overlying the zygomatic muscles and anteroinferiorly to
surgical face-lift pool during their preoperative office visit and
the nose and lip. The superficial muscular aponeurotic system
during routine 3- to 6-month follow-up visits. Six sets of base-
of the jowl was undermined from the parotid gland to the
line and follow-up surgical face-lift images with baseline facial
masseter. The dissection continued anteriorly over the masse-
laxity spanning mild (n = 1), moderate (n = 3), and advanced
ter muscle border and inferiorly over the lower border of the
(n = 2) categories were selected by one of us (D.R.) as repre-
mandible, extending anteriorly to where the facial artery
sentative surgical face-lift patients. Photographs were taken
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
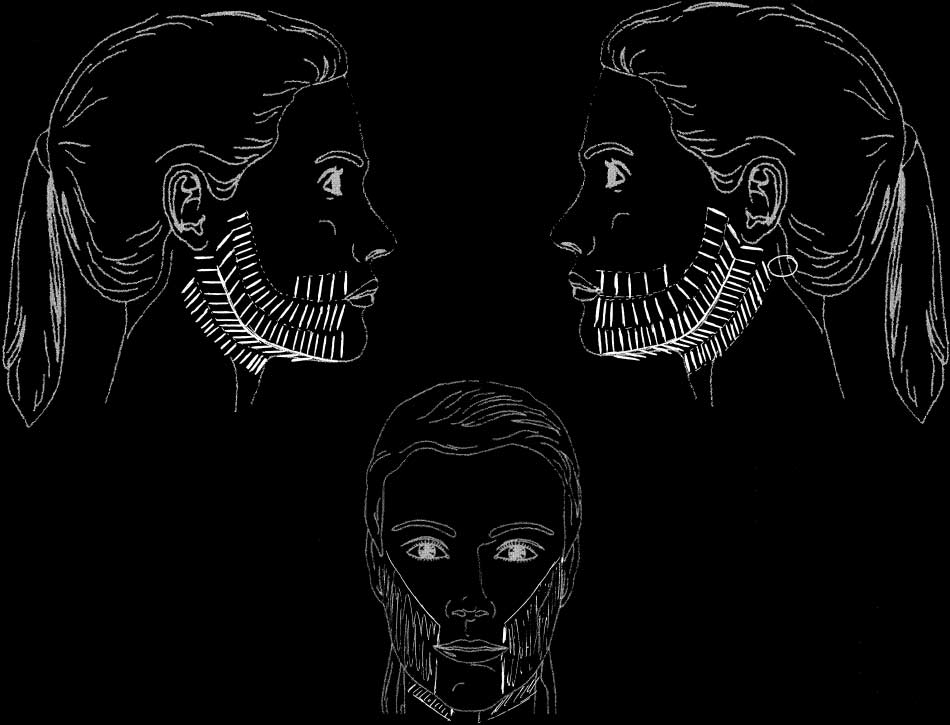
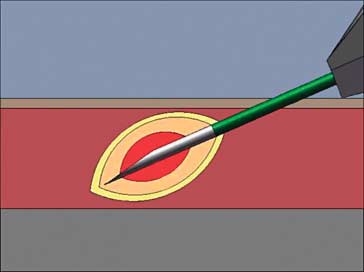
Figure 2. Schematic representation of the insertion sites and distribution of the electrode tips of the handpiece. The paired electrode tips were inserted at an interval of
3 to 5 mm apart in the distribution shown. A total of 155 insertions were administered to this patient. The insertion sites typically involved the melolabial folds medially
on the lower part of the face extending to the preauricular regions, as shown. In the submental and submandibular regions, insertions were typically delivered from the
midline submental region medially extending to the infra-auricular regions laterally and the lateral aspects of the upper part of the neck inferiorly.
using a digital single-lens reflex camera (model E-500; Olym-
and mean follow-up grades, and a paired t test was used to
pus America, Central Valley, Pennsylvania) fitted with an
assess statistical significance. The mean baseline and
external shoe-mounted electronic flash (model FL-50, Olym-
follow-up grades for each treatment modality group were then
pus America) and a fixed focal length 50-mm 1:2 macro lens
averaged and compared using a paired t test. The percentage
(Olympus ED), using standardized settings (F9.0, 1/125,
FRF to surgical face-lift result and the percentage improve-
ISO400) from a 1-m distance and in a photography room with
ment over baseline for each patient pool were calculated.
set lighting for every patient. The FRF treatment and surgicalface-lift photographs were equivalently cropped and random-ized. Five independent blinded evaluators graded the uniden-
tified images using a Quantitative Comprehensive Grading
Scale for facial and neck laxity8-10 (Table 1). The grading sys-
tem is binary, and blinded evaluators determine the patient'slaxity grade category based on the presence or absence of a
given finding (eg, melolabial folds). Two of the blinded evalu-ators ( J.D. and K.A.) have used this grading scale in a prior
Fifteen sequential patients completing treatment and
study.12 The evaluators were not informed of the randomized
follow-up were included in the FRF group. All
comparison to the surgical face-lift or of the nature of the
patients were women, and the mean (SD) age was 59.7
intervention. Upon unblinding, the results were tabulated,
(8.9) years. Two patients (13%) were Fitzpatrick skin
grouped, and analyzed. Mean baseline and follow-up grades
type I, 8 (53%) were type II, 4 (27%) were type III,
with standard deviations were calculated for each patient. Thereliability of the grade assignment agreement of independent
and 1 (7%) was type IV. In the surgical face-lift group
evaluators was assessed by calculating a Fleiss statistic using
(6 patients), all patients were women, and the mean
each one-half point grade assignment from 0 to 4 of the laxity
(SD) age was 54.0 (9.2) years. Three patients (50%)
scale as categorical ratings. The improvement for each patient
were Fitzpatrick skin type I and 3 (50%) were type II.
was calculated as the difference between the mean baseline
The baseline mean laxity grades were similar: 2.76 for
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
Table 1. Quantitative Comprehensive Grading Scalea of Rhytids, Laxity, and Photoaging 8-10
Skin Aging and Photodamage
Wrinkles in motion: Localized, NL folds
Few (1-3) discrete,
Wrinkles in motion: Localized, NL and
Yellow hue or early,
Pink E or several T,
localized 2 sites
Wrinkles at rest:
Red E or multiple T, Multiple, small
Wrinkles at rest:
Yellow hue, PO and
Multiple small and
Red E or multiple T, Multiple, large
Wrinkles at rest:
Wrinkles at rest:
Deep NL/ML folds,
or multiple large
little uninvolved
little uninvolved
Deep, violaceous E
distributed, deep
Abbreviations: EB, elastotic beads; E-T, erythema-telangiectasia; FRF, fractional radiofrequency; ML, melolabial; NL, nasolabial; PO, perio-orbital;
a This 4-point grading scale has been extensively tested and used for evaluating laser and energy-based cosmetic treatments.9,11-13 The laxity category was used
by blinded evaluators to assess the baseline and follow-up laxity grades following surgical face-lift and FRF treatment in the present study.
the FRF group and 2.47 for the surgical face-lift group
(Table 2).
There were no adverse events or complications in the FRF
treatment group. All participants experienced transienterythema, swelling, and ecchymoses, which resolved in
Photographic examples of typical patient outcomes from
5 to 10 days. On a scale of minimal, mild, moderate, ad-
surgical face-lift and FRF treatment are shown in
vanced, and severe, the erythema was mild to moderate
Figures 3, 4, 5, 6, and 7. The results of the blinded
and resolved within 24 hours in the vast majority of pa-
grading evaluation and statistical analysis for the FRF
tients. The edema varied from minimal to moderate among
treatment and surgical face-lift patient groups are shown
the patients and resolved gradually in 5 to 10 days. Ec-
in Table 2. These results are summarized and compared
chymoses varied from minimal to advanced and re-
in Table 3. There was good agreement between the lax-
solved in the vast majority of patients within 5 to 10 days,
ity grades assigned by all independent evaluators (Fleiss
with the exception of 1 patient who had residual yellow-
=0.45), with standard errors less than or equal to the
brown discoloration that resolved 2 to 3 weeks postop-
laxity scale resolution. The mean (SD) laxity grade im-
eratively. Topical anesthesia minimized discomfort as-
provement for the FRF treatment and surgical face-lift
sociated with microneedle deployment. However, topical
patient pools were 0.44 (0.20) (P ⬍ .001) and 1.20
anesthesia alone proved marginal to inadequate for man-
(0.44) (P⬍.001), respectively. The percentage improve-
aging discomfort associated with dermal heating during
ments relative to mean baseline for the FRF treatment
FRF energy delivery. In contrast, patients receiving di-
and surgical face-lift patient pools were 16% and 49%,
luted local anesthesia with or without prior topical an-
respectively. The mean percentage improvement for FRF
esthesia tolerated all aspects of treatment with minimal
treatment was 37% that of the surgical face-lift.
discomfort. All patients returned to normal activities
Patient self-assessments of clinical improvements from
within 24 hours.
FRF yielded a mean rating of moderate for rhytids and
All surgical face-lift patients had sutures in place for
moderate to significant for laxity. Patient satisfaction with
7 days and experienced scarring, which varied from mild
FRF treatment was high: 0% were dissatisfied; 7%, neu-
to hypertrophic, at surgical margins. In 4 of the 6 surgi-
tral; 60%, satisfied; and 33%, very satisfied.
cal patients, hypertrophic scars developed in the pre- and
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.

Table 2. Blinded Grading Data of 15 FRF and 6 Surgical
Grade (SD)
FRF Treatment Group
Surgical Face-lift Group
Figure 3. Surgical face-lift patient (P2) at baseline (A) and at the 6-month
follow-up visit (B). Blinded grading by 5 independent physicians resulted in amean improvement in skin laxity of 1.60 grades on the 4-point grading scale.
Abbreviations: FRF, fractional radiofrequency; NA, not applicable.
Blinded evaluators were unaware of the types of treatments being evaluated
a Each randomized digital baseline and follow-up image was evaluated by
(fractional radiofrequency or surgical face-lift) and were also blinded to
5 blinded evaluators using the quantitative 4-point laxity grading scale. Upon
pretreatment and posttreatment photographs.
unblinding, the mean baseline and follow-up laxity grades were calculated foreach FRF and surgical face-lift patient, and the mean change in laxity gradewas calculated. In both groups, the mean laxity grade change was
When assessed by 5 blinded evaluators of randomized
statistically significant (P ⬍.001).
photographs, the mean laxity grade improvement fromthe surgical face-lift in this cohort of patients was 1.20on a 4-point laxity grading scale, with FRF treatment
posterior-auricular regions. These were treated postop-
achieving a 0.44-grade improvement (Table 3). The
eratively with intralesional triamcinolone acetonide and
improvement in skin laxity relative to baseline from a
pulsed dye laser localized to the scar margins. Ecchymo-
surgical face-lift was calculated as 49%, and FRF treat-
ses and edema were present in all patients postopera-
ment resulted in a 16% improvement over baseline, or
tively for 2 to 4 weeks. The ecchymoses were mild to ad-
37% of a surgical face-lift result from a single minimally
vanced and resolved by the 4-week follow-up visit. The
invasive treatment. A 16% laxity improvement above
edema varied from mild to advanced and resolved within
the baseline from a single nonsurgical intervention is a
2 to 4 weeks. Among the 6 patients selected, no patients
significant improvement, considering that the gold
experienced hematoma formation, flap necrosis, or in-
standard treatment with its associated risks and compli-
fection. Patients returned to normal activities within 7
cations yielded a 49% improvement.
The laxity improvements quantified here for the
surgical face-lift and this novel RF device provide
needed evidence-based outcome measurements forwhat has been a largely descriptive field and will assist
In evidence-based medicine, it is generally agreed that
in managing patient expectations. The mean improve-
the validity of a novel treatment is best tested by com-
ment in laxity grade of 1.20 for the surgical face-lift
parative trial to the gold standard. Until now, such a
indicates that this gold standard procedure can pro-
comparative trial had not been performed for nonsurgi-
vide a reduction in a patient's laxity grade from severe
cal treatments of skin laxity, owing to the absence of a
to advanced, advanced to moderate, or moderate to
quantitative measure for the outcome of the surgical
mild, but will not, on average, improve laxity from
face-lift. In this study, a quantitative blinded graded
severe to moderate, advanced to mild, or moderate to
value in laxity improvement has been assigned to the
none. By placing patients in a specific laxity grade cat-
gold standard surgical face-lift, allowing for comparison
egory, it is now possible to show them on the grading
with a minimally invasive nonsurgical FRF treatment.
table what outcome to expect from a single grade
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
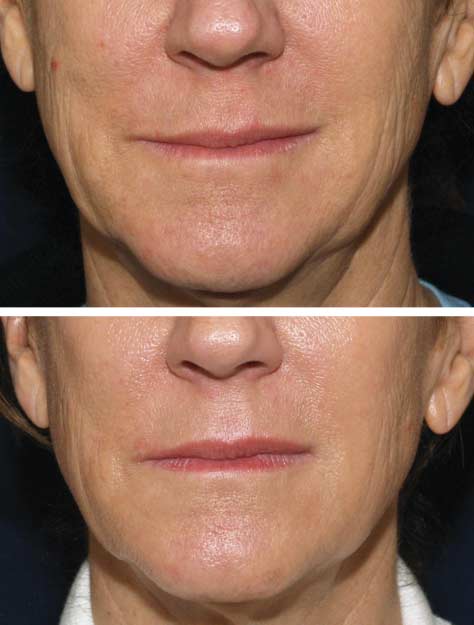

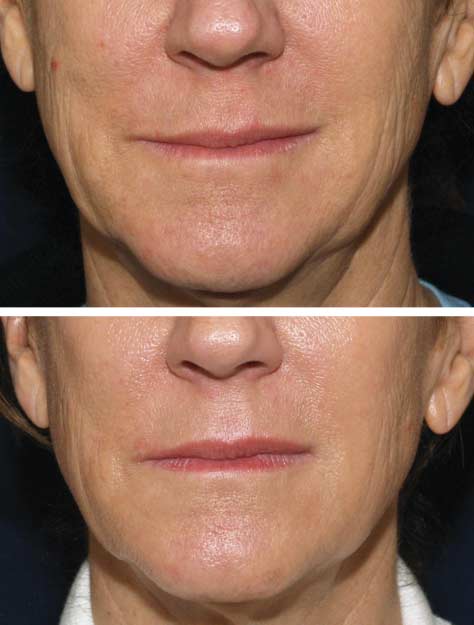
Figure 4. Fractional radiofrequency (FRF) treatment patient (M09) at
baseline (A) and at the 6-month follow-up visit (B). Blinded grading by
5 independent physicians of randomized baseline and 6-month follow-up
photographs, which had been randomized with surgical face-lift
photographs, demonstrated a mean improvement in skin laxity of 0.40 grade
on the 4-point grading scale after a single FRF treatment. The 2
erythematous papules on the right cheek in the pretreatment photograph are
Figure 5. Surgical face-lift patient (P3) at baseline (A) and at the 6-month
acne lesions, which are no longer present in the posttreatment photograph.
follow-up visit (B). Blinded grading by 5 independent physicians resulted in amean improvement in skin laxity of 0.60 grade on the 4-point grading scale.
Blinded evaluators were unaware of the types of treatments being evaluatedand were also blinded to pretreatment and posttreatment photographs,
reduction following a surgical face-lift, thereby tem-
which were randomized with fractional radiofrequency (FRF) images.
pering expectations in specific terms. Of equal impor-tance, the quantitative measure of relative outcome of
Given the rigor of blinding and the inclusion of der-
nonsurgical alternatives enables patients to make more
matologist and plastic surgeon graders, the benefits of
informed choices from among different treatment
grading to a quantitative scale was demonstrated by the
modalities based on their baseline condition and treat-
strong agreement between laxity grades assigned by all
ment expectations. The findings and methods pre-
independent evaluators. The grading system resulted in
sented herein provide a basis for future studies to test
narrow standards of error and a Fleiss statistic of 0.45,
the validity of novel therapies and to quantitatively
consistent with strong agreement given the nine 1⁄2-
assess and compare changes in skin laxity from surgi-
grade categories and 5 graders. The baseline mean lax-
cal and nonsurgical treatments alike to the gold stan-
ity grades in the 2 groups were similar, with a slightly
dard treatment.
higher baseline grade for the FRF group (2.76 vs 2.47
Two important aspects of the methods used in the
for surgical face-lift), therefore eliminating bias toward
present study were the rigor of randomization and blinded
more advanced cases in the surgical face-lift group. The
evaluation and the use of a quantitative grading scale. Base-
extent of change in laxity from surgical treatment is greater
line and follow-up photographs from patients undergo-
than that from FRF; therefore, fewer surgical than FRF
ing both surgical face-lift and FRF were randomly as-
participants were required to achieve statistical signifi-
sorted, then sent to 5 independent evaluators who were
cance. Statistical significance was achieved in both pa-
blinded to which image was baseline or follow-up and
tient pools, suggesting that the number of patients in each
to the types of treatments being compared. The evalua-
pool was appropriate for the degree of improvement
tors were unaware that photographs of 2 different treat-
ment modalities were randomly intermixed or that sur-
This study is the first to use a reproducible, quanti-
gical face-lift photographs were included in the study.
tative grading scale for the evaluation of skin laxity by
The use of 5 evaluators, including dermatologists and plas-
blinded evaluators to assess the clinical outcome from
tic surgeons, allowed for greater statistical accuracy of
the surgical face-lift and to compare it with an alterna-
laxity grades.
tive, nonsurgical therapy. Nonsurgical skin tightening
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
Figure 6. Fractional radiofrequency (FRF) treatment patient (M10) at
Figure 7. Three-quarter–angle view of fractional radiofrequency (FRF) treatment
baseline (A) and at the 6-month follow-up visit (B). Blinded grading by
patient (M02) at baseline (A) and at the 6-month follow-up visit (B). Blinded
5 independent physicians of randomized baseline and 6-month follow-up
grading by 5 independent physicians of randomized baseline and 6-month
photographs, which had been randomized with surgical face-lift
follow-up photographs, which had been randomly intermixed with surgical
photographs, demonstrated a mean improvement in skin laxity of 0.50 grade
face-lift photographs, demonstrated a mean skin laxity improvement of 0.60
on the 4-point grading scale following a single FRF treatment.
grade on the 4-point grading scale from a single FRF treatment.
techniques have previously been quantitatively as-sessed using this grading scale; however, the current de-
Table 3. Comparison of FRF Treatment and Surgical
vice demonstrated much higher efficacy in treating skin
Face-lift Blinded Grading Resultsa
laxity. These prior device studies reported 0.075 to 0.236
mean laxity grade improvement per treatment.9,11-13 All
of these previously tested techniques were skin-surface
applied RF or infrared laser or light devices. The cur-
rent device demonstrated a mean grade improvement of
0.44, significantly higher than all prior studies follow-
ing a single treatment. Prior skin-surface RF devices have
been observed to yield lower efficacy in reducing laxityin fat faces; in contrast, the FRF treatment demon-
Abbreviations: FRF, fractional radiofrequency; NA, not applicable.
a The mean baseline, follow-up, and improvements in laxity grades as
strated similar laxity grade reductions among the thin vs
assessed by 5 independent blinded evaluators of randomized digital images
fat faces in the present study, although the numbers were
are shown. The percentage improvement was then calculated for FRF relative
too small for statistical comparison.
to the surgical face-lift group and for each treatment relative to baseline.
To date, there has been no prior report of surgical face-
P ⬍.001 for all comparisons.
c FRF treatment resulted in 37% of the level of improvement of the surgical
lifting evaluated with quantitative grading scales by
face-lift result, ie, (0.44/1.20)⫻100.
blinded evaluators. Prior studies evaluating the improve-
d Comparison of each percentage improvement in laxity compared with
ments from surgical face-lifts have used subjective, de-
baseline for each treatment group.
scriptive grades of "poor," "good," or "excellent" in anunblended manner.5-7 In addition, it is important to note
ity improvements from the surgical face-lift and a basis
that the surgical face-lift entails treating the subcutane-
for comparison of this novel FRF technology with prior
ous and deeper tissues, including lipectomy and platys-
skin-tightening technologies. The findings presented here
mal flaps, in contrast to FRF, which only targets the der-
also now make possible further research into transla-
mis (see the "FRF Treatment Protocol" sub-subsection
tion of clinical laxity grade reductions from these "turn-
of the "Methods" section). Thus, the results of the quan-
back-the clock" treatments into age-specific reductions.
titative, blinded, and randomized study design pre-
The rationale for such an analysis is that the current lax-
sented here provide the first quantitative measure of lax-
ity grading scale with its small margins of error among 5
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
independent blinded evaluators, both dermatologists and
the surgical face-lift, using most rigorous standards. The
plastic surgeons, provides a basis for analyzing the av-
direct insertion of paired electrodes into the dermis, pre-
erage laxity grade for each age. As stated in the intro-
cise delivery of the energy into the target dermis, real-
duction, skin aging may be categorized as intrinsic and
time attainment of target tissue temperature, and speci-
extrinsic; laxity is a feature primarily of the former and
fied time-at-temperature appear to correlate with more
is the result of many factors. In spite of the multifacto-
efficient skin tightening and laxity reductions following
rial nature of progressive skin laxity with age, it is pos-
a single treatment as compared with prior skin-surface
sible to calculate the mean laxity grade per age group if
technologies. The goal in the nonsurgical field has been
one includes large numbers of patients of different skin
to reach this point, wherein a single treatment, as op-
types in the general population. These large numbers
posed to a series of treatments, can attain significant clini-
should control for additional variables such as body mass,
cal results that can be compared with the gold standard
sun exposure, or genetic variability. By calculating the
and that can be designed rationally to target specific bio-
mean laxity grades for age groups across the general popu-
logical end points.
lation, it will now be possible to translate a laxity grade
In conclusion, the gold standard treatment, the sur-
reduction into a correlate mean laxity age reduction in
gical face-lift, has been quantified in its degree of im-
years. For example, a 1.20–laxity grade reduction from
provement in skin laxity and compared with a novel, mini-
a surgical face-lift may translate into making a 55-year-
mally invasive FRF treatment using randomized, blinded
old look 45, but not 35 if one examines the average lax-
grading with a previously tested laxity grading scale. This
ity grade per age group and calculates a 1.20-grade re-
randomized, blinded, quantitative comparative study pro-
duction. The same type of calculation will now also be
vides a basis for quantifying cosmetic outcomes from novel
possible for nonsurgical alternatives; for example, a 0.44–
treatments with valid comparative analysis to the gold
laxity grade reduction from FRF may be translated in a
standard. It also suggests that minimally invasive FRF
several year reduction in laxity age, on average. The as-
treatment may provide an important nonsurgical op-
signment of laxity age reductions to laxity grade reduc-
tion for the treatment of facial skin laxity.
tions is another important application of the findings pre-sented here that will further the ability to accurately inform
Accepted for Publication: November 4, 2009.
patients of predicted outcomes of surgical and nonsur-
Author Affiliations: Department of Dermatology, Yale
gical alternatives so that they may make better informed
University School of Medicine, New Haven, Connecti-
decisions. The underlying mechanism for improvement
cut (Drs Alexiades-Armenakas, Dover, and Arndt); Der-
in laxity following thermal injury to the dermis is be-
matology and Laser Surgery Center (Dr Alexiades-
lieved to derive from dermal remodeling and neocolla-
Armenakas) and Manhattan Eye and Ear Infirmary
genesis following treatment.
(Dr Rosenberg), New York, New York; Iridex Corp,
Prior studies using various laser- and light-based de-
Mountain View, California (Dr Renton); SkinCare Phy-
vices have repeatedly demonstrated that dermal tem-
sicians, Chestnut Hill, Massachusetts (Drs Dover and
peratures in excess of 55°C are required to induce col-
Arndt); and Departments of Dermatology, Dartmouth
lagen denaturation, and that this denaturation is followed
Medical School, Hanover, New Hampshire, and Har-
by neocollagenesis during a 6- to-12-month period.8 The
vard Medical School, Boston, Massachusetts (Dr Arndt).
disadvantage of prior modalities is that temperature at-
Correspondence: Macrene Alexiades-Armenakas, MD,
tainment in the dermis is theoretical based on Monte-
PhD, Department of Dermatology, Yale University School
Carlo simulations and relies on skin surface infrared tem-
of Medicine, 955 Park Ave, New York, NY 10028
perature measurements. The current FRF device has the
technological advantage of real-time temperature feed-
Author Contributions: Drs Alexiades-Armenakas, Renton,
back, allowing a specific target temperature of 62°C to
and Arndt had full access to all the data in the study and
78°C to be preselected and attained in the dermis.3,4 In
take responsibility for the integrity of the data and the
addition, precise times-at-temperature have been imple-
accuracy of the data analysis. Study concept and design:
mented for the first time using this real-time feedback
Alexiades-Armenakas, Rosenberg, and Renton. Acquisi-
system, unique to the current device. The time-at-
tion of data: Alexiades-Armenakas, Rosenberg, Renton,
temperature is a second critical element to inducing ad-
Dover, and Arndt. Analysis and interpretation of data: Alex-
equate thermal denaturation. Once dermal thermal in-
iades-Armenakas, Rosenberg, Renton, Dover, and Arndt.
jury has been caused, this is followed by progressive
Drafting of the manuscript: Alexiades-Armenakas, Rosen-
neocollagenesis, which has been shown to correlate with
berg, and Renton. Critical revision of the manuscript for
progressive clinical tissue tightening.8
important intellectual content: Alexiades-Armenakas,
This FRF is the first light- or energy-based modality
Rosenberg, Renton, Dover, and Arndt. Statistical analy-
to be shown to induce elastogenesis.4 This finding has
sis: Alexiades-Armenakas and Renton. Obtained fund-
been clinically correlated with increased skin elasticity
ing: Alexiades-Armenakas. Administrative, technical, and
as measured by elastometry.14 It is possible that the in-
material support: Alexiades-Armenakas, Rosenberg,
duction of collagen and elastin in part contributes to the
Renton, Dover, and Arndt.
superior laxity reductions quantified here. Thus, the ra-
Financial Disclosure: Dr Alexiades-Armenakas re-
tional device-design approach put forth here resulted in
ceived a research grant from Primaeva Medical, Inc, and
significant clinical findings from a single treatment, which
served on the company's medical advisory board for 5
correlate with histological changes, and are supported by
months during the study. She no longer serves on the ad-
a legitimate comparison to the gold standard treatment,
visory board and is neither a consultant nor a share-
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
holder. At the time of the study, Dr Renton was em-
5. Berry MG, Davies D. Platysma-SMAS plication face-lift [published online ahead
ployed by Primaeva Medical, Inc, but is no longer an
of print March 26, 2009]. J Plast Reconstr Aesthet Surg. 2009. doi:10.1016/j.bjps.2009.02.067.
employee of the company.
6. Becker FF, Bassichis BA. Deep-plane face-lift vs superficial musculoaponeurotic
Funding/Support: This study was supported in part by
system plication face-lift: a comparative study. Arch Facial Plast Surg. 2004;
a research grant from Primaeva Medical, Inc.
Role of the Sponsors: The sponsors had no role in the
7. Ivy EJ, Lorenc ZP, Aston SJ. Is there a difference? a prospective study compar-
design and conduct of the study; in the collection, analy-
ing lateral and standard SMAS face-lifts with extended SMAS and compositerhytidectomies. Plast Reconstr Surg. 1996;98(7):1135-1147.
sis and interpretation of the data; or in the preparation,
8. Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin re-
review, or approval of the manuscript.
surfacing: non-ablative, fractional and ablative laser resurfacing. J Am Acad
Additional Contributions: Suzanne Kilmer, MD, An-
drea Willey, MD, and James Newman, MD, provided in-
9. Alexiades-Armenakas MR. Rhytides, laxity and photoaging treated with a com-
bination of radiofrequency, diode laser, and pulsed light and assessed with a com-
valuable assistance as blinded evaluators of the random-
prehensive grading scale. J Drugs Dermatol. 2006;5(8):609-616.
ized pretreatment and posttreatment images.
10. Alexiades-Armenakas M. A quantitative and comprehensive grading scale for rhyti-
des, laxity and photoaging. J Drugs Dermatol. 2006;5(8):808-809.
11. Alexiades-Armenakas M. Non-ablative skin tightening with a variable depth heat-
ing 1310 nm–wavelength laser in combination with surface cooling. J DrugsDermatol. 2007;6(11):1096-1103.
1. Rabe JH, Mamelak AJ, McElgunn PJS, Morison WL, Sauder DN. Photoaging:
12. Alexiades-Armenakas M, Dover JS, Arndt KA. Unipolar versus bipolar radiofre-
mechanisms and repair. J Am Acad Dermatol. 2006;55(1):1-19.
quency treatment of rhytides and laxity using a mobile painless delivery method.
2. Alexiades-Armenakas M. Laser skin tightening: non-surgical alternative to the
Lasers Surg Med. 2008;40(7):446-453.
face-lift. J Drugs Dermatol. 2006;5(3):295-296.
13. Alexiades-Armenakas M. Assessment of the mobile delivery of infrared light (1100-
3. Hantash BM, Renton B, Berkowitz RL, Stridde BC, Newman J. Pilot clinical study
1800 nm) for the treatment of facial and neck skin laxity. J Drugs Dermatol. 2009;
of a novel minimally invasive bipolar micro-needle radiofrequency device. La-
sers Surg Med. 2009;41(2):87-95.
14. Willey A, Newman J, Renton B, Berube D, Krishna S, Kilmer S. Minimally-
4. Hantash BM, Ubeid AA, Chang H, Kafi R, Renton B. Bipolar fractional radiofre-
invasive fractional bipolar radiofrequency for the treatment of facial laxity and
quency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg
rhytides. Poster presented at: 29th Annual Conference of the American Society
for Laser Medicine and Surgery; April 1-5, 2009; National Harbor, MD.
(REPRINTED) ARCH DERMATOL/ VOL 146 (NO. 4), APR 2010
2010 American Medical Association. All rights reserved.
Source: http://www.syneron-candela.cn/sites/default/files/ePrime%20Alexiades_et_al_-_published_version_0.pdf
Detail-Document #241001 −This Detail-Document accompanies the related article published in− PHARMACIST'S LETTER / PRESCRIBER'S LETTER October 2008 Volume 24 Number 241001 Stability of Refrigerated and Frozen Drugs —Chart modified November 2008— (Based on U.S. product labeling and relevant studies)
Rivastigmine for the treatment of dementia associated with Parkinson's disease Jennifer L Reingold Abstract: Parkinson's disease (PD) affl icts millions of people worldwide and leads to cognitive impairment or dementia in the majority of patients over time. Parkinson's disease dementia (PDD) is characterized by defi cits in attention, executive and visuospatial function, and memory.