Powerpoint-präsentation



Pain before, during and after
endodontic emergency treatment
• Pain control before emergency treatment
• Pain control during emergency treatment
• Pain control after emergency treatment
• Rules of thumb:
• There is ample evidence that:
Pretreatment with antibiotics is not beneficial and seems
antibiotics are not efficacious in preventing post-
to have no therapeutic benefit
treatment symptoms of pain or swelling (flare-ups)
(Longman et al., J Dent 2000)
Antibiotics are not an alternative to dental
intervention, they are an adjunct to it (Abbott et al., Aust
antibiotics are ineffective for pain relief in the case of
Dent J 1990; Martin et al., Br Dent J 1997)
irreversible pulpitis (Nagle et al., Oral Surg 2000)
Antibiotics are indicated if there is a diffuse spreading
antibiotics are ineffective for pain relief in the case of
infection or evidence of systemic
symptomatic apical periodontitis (Fouad et al., Oral Surg
involvement (feeling of malaise;
1996; Henry et al., J Endod 2001; Torabinejad et al., J Endod
elevated body temperature)
(Longman et al., J Dent 2000)
• Corticoids are effective for the prevention of post-
• Corticoids are effective for the prevention of post-
treatment pain :
treatment pain :
Double-blind parallel-randomized clinical study: 30 mg
Numerous clinical trials have shown that pre-treatment with
prednisolone 30 min before root canal treatment (oral) >
oral corticoids is effective in reducing post-endodontic pain
significantly less post-operative pain (Jalalzadeh et al., J
for at least 12 hours (Marschall et al., J Endod 1993; Glassman
Endod 2010)
et al., Oral Surg 1989; Mehrvarzfar et al., Aust Endod J 2008;
Placebo-controlled study > pretreatment with 4 mg
Liesinger et al., J Endod 1993)
dexamethasone > significantly less post-endodontic pain
Oral administration of 30 mg prednisolone or 0.75-4 mg
after 4-12 hours after treatment (Pochapski et al., Oral Surg
dexamethasone 30-60 min before treatment




• Effective for the prevention of post-treatment pain are:
• Pain control before emergency treatment
ibuprofen 800 mg (Jackson et al., J Am Dent Assoc 189;
• Pain control during emergency treatment
Doroschak et al., J Endod 1999)
if patients may not be able to tolerate non-steroidal anti-
inflammatory drugs (NSAIDs) (gastro-intestinal disorders,
• Anodyne medicaments
active asthmatics, hypertension) > acetaminophen
• Pain control after emergency treatment
1000 mg (Moore et al., J Am Dent Assoc 1986)
In general, ibuprofen is more effective than
acetaminophen (Dionne et al., J Clin Pharmakol 1983)
• Irreversible pulpitis of mandibular molars:
• Anaesthesia in the maxilla:
Single inferior alveolar nerve block injection is ineffective
Infiltration injection
in 30-80% of patients with diagnosis of irreversible
Palatal injection > 0.3 ml, premolars and molars
pulpitis (Nusstein et al., J Endod 1998; Reisman et al., Oral
Periodontal ligament injection > 0.2 ml per injection; two
Surg 1997; Claffey et al., J Endod 2004)
injections per root > sufficient for endodontic procedures
Premedication with ibuprofen > significantly deeper
in 60-70% of cases (Meechan, Int Endod J 2002)
anaesthesia during root canal treatment (Modaresi et al.,
Oral Surg 2006; Parirokh et al., J Endod 2010)
1 hour before local anaesthesia 200 mg ibuprofen
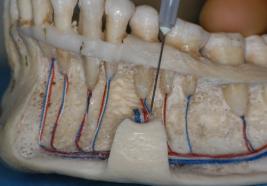
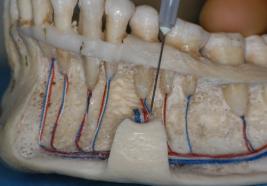
• Supplemental injections: intrapulpal injection
• Anaesthesia in the mandible:
Effective intrapulpal injection depends on back-pressure
Inferior alveolar block injection
Effect of intrapulpal injection is independent of the
buccal infiltration
solution used (VanGheluwe & Walton, Oral Surg 1997)
Mylohyoid infiltration > branches of the mylohyoid nerve >
second and third molars
Mental foramen injection >
premolars and first molar
Periodontal ligament injection
> 0.2 ml per injection;
two injections per root
Supplemental injections: intraosseous injection
Supplemental injections: intraosseous injection
Direct access to the cancellous bone
Onset of anaesthesia is immediately (Gallatin et al., J Am
Perforate the cortical plate with rotating drill > unattached
Deent Assoc 2003)
gingiva, distal to the tooth to be anaesthetised
Up to 91% successful in gaining total pulp anaesthesia
in molars with irreversible pulpitis (Nusstein et al., J Endod 1998)
Pain of perforation
Perforator breakage > about 1% (Reader & Nusstein,
Endodonticc Topics 2002)
Systemic effects > in about 50-96% of cases increase in
X-tip (Dentsply Tulsa)
heart rate > 23-28 beats per minute (Reader & Nusstein,
drill = hollow needle
Endodonticc Topics 2002)
• The "hot" tooth
• Pain control before emergency treatment
If non of the afore mentioned measures blocks the pain in
• Pain control during emergency treatment
a patient with painful pulpitis, last resort >
Application of Ledermix or eugenol to the exposed pulp
• Pain control after emergency treatment
Anodyne medicaments suppress the inflammation >
better effect anaesthetic in the
next appointment
(2-3 weeks later)
• Pain is not an indication for antibiotic treatment (Henry
et al., J Endod 2001)
• Again, antibiotics are only indicated when the patient is
febril and for patients who present with cellulitis
Pain Research Unit, Department of Anesthesia, Oxford;
• Analgesics are mere an adjunct to causal treatment
• Causal endodontic treatment > more than 50% pain
reduction by one day, about 90% by 2 days (Doroschak
et al., J Endod 1999)
• Post-operative prescription of analgesics only for 2
• Meta-analysis of the effectiveness of non-steroidal anti-
• First analgesic should be taken directly after the
inflammatory analgesics > NSAIDs were either as
endodontic treatment
effective or more effective than codeine-based
• Analgesic should be taken „by the clock" > for the first
analgesics (NSAIDs were also associated with fewer
2 days every 6 hours (Keiser & Hargreaves, Endodontic
complications (Biddle, AANA J 2002)
Topics 2002)
• Analgesics of first choice for post-operative pain:
ibuprofen 800 mg (Holstein et al., Endodontic Topics
• Patients who cannot tolerate NSAIDs > acetaminophen
Source: https://nvve.com/assets/files/Congressen_2/2011maart11/Hand-out_prof.dr.Schafer.02.pdf
Prevention of Type 2 DiabetesInsulin Resistance and -Cell FunctionJ.-L. Chiasson and Re ´ mi Rabasa-Lhoret Type 2 diabetes is increasing worldwide in epidemic pro- (2– 4). Type 2 diabetes will certainly be one of the major portions. Its associated morbidity and mortality is impos- diseases of the 21st century and should be recognized as a
Viterol.A (viatrozene gel) 16% and patients with sunburn should beadvised not to use the product until ful y recovered. • Weather extremes, such as wind or cold, also may be irritating to patients under treatment with Viterol.A. Drug Interactions: Concomitant use of potential y irritating topical products (medicated or abrasive soaps and cleansers, soaps and cosmetics that have a strong drying ef ect, and products with high concentrations of alcohol, astringents, spices, or lime) should be approached with caution. Particular caution should be exercised in using preparations containing sulfur, resorcinol, or salicylic acid in combination with Viterol.A.