E-asta.cn
Prevention of Type 2 Diabetes
Insulin Resistance and -Cell Function
J.-L. Chiasson and Re
´ mi Rabasa-Lhoret
Type 2 diabetes is increasing worldwide in epidemic pro-
(2– 4). Type 2 diabetes will certainly be one of the major
portions. Its associated morbidity and mortality is impos-
diseases of the 21st century and should be recognized as a
ing a major burden on the health care system. Based on a
better understanding of the pathophysiology of glucose
It is now well established that the development of type
intolerance, clinical trials on the prevention of diabetes
2 diabetes results from the interaction between the genetic
have been performed. It has now been demonstrated that
makeup of the individuals and their environment (5). The
diet and exercise, metformin, acarbose, and troglitazone
development of obesity seems to be an important factor in
can prevent or at least delay the development of diabetes
the development of insulin resistance (6,7). If this insulin
in subjects with impaired glucose tolerance (IGT). It is
resistance occurs in the presence of a genetically deter-
now generally accepted that insulin resistance and 
-cell
mined propensity to -cell dysfunction, glucose intoler-
dysfunction are major factors involved in the development
of diabetes. The relative contribution of insulin resistance
ance can occur (5). Although there is still disagreement
versus 
-cell dysfunction on the pathogenesis of diabetes
over the relative contribution in the alterations in insulin
has aroused much debate. These two processes should be
sensitivity versus -cell function in the development of
studied in relation to one another: their relationship is
diabetes, it is becoming clear that reductions in both
best described as hyperbolic in nature. When this relation-
processes have already occurred by the time hyperglyce-
ship is taken into consideration, it becomes evident that
mia develops (8).
subjects at risk of developing type 2 diabetes have 
-cell
The concept for the prevention of diabetes developed on
dysfunction before they develop glucose intolerance. In-
the basis of a better understanding of the pathophysiology
sulin resistance may be mostly explained by the presence
of glucose intolerance and stimulated by the ever-increas-
of obesity and accelerate the progression to diabetes in
ing burden of the disease. It has now been demonstrated
subjects with the propensity to 
-cell failure. By the time
hyperglycemia occurs, impairment in both insulin sensitiv-
that diabetes can be prevented, or at least delayed, by
ity and insulin secretion are present. There are still few
nonpharmacological interventions, such as lifestyle modi-
data on insulin sensitivity and insulin secretion from the
fication including diet and exercise (9 –11), and by phar-
trials on the prevention of diabetes. The few data that we
do have suggest that most interventions mostly have an
acarbose (12), and troglitazone (13) (Table 1).
effect on insulin resistance. By reducing insulin resis-
The purpose of this article is to discuss the mecha-
tance, they protect and preserve the 
-cell function. No
nism(s) involved in the prevention of type 2 diabetes by
intervention has yet shown any direct effect on 
-cell
those different interventions. Is it through an effect on
function. Diabetes 53 (Suppl. 3):S34 –S38, 2004
insulin resistance and/or insulin secretion or through someother mechanisms? In the first part, we will briefly reviewthe pathophysiology of type 2 diabetes. In the second part,
we will describe the major intervention trials on the
he prevalence of type 2 diabetes is increasing in
prevention of type 2 diabetes and discuss the probable
epidemic proportions worldwide. It has been
mechanism(s) involved in the prevention of diabetes.
estimated that the diabetic population will dou-ble from 150 to 300 million in the next 25 years
(1). Furthermore, the long-term complications associated
THE PATHOPHYSIOLOGY OF TYPE 2 DIABETES
with diabetes are major causes of morbidity and mortality,
For a more detailed discussion on the pathogenesis of type
imposing a high financial burden on health care costs
2 diabetes, we refer the readers to the recent review articleby Kahn (14). For the purpose of our discussion, we willbriefly discuss insulin resistance, insulin secretion, and
From the Research Centre, Centre Hospitalier de l'Universite´ de Montre´al–
their interactions in the development of type 2 diabetes.
Hoˆtel-Dieu, and the Department of Medicine and Nutrition, University ofMontreal, Montreal, Quebec, Canada.
Several longitudinal studies have clearly shown that
Address correspondence and reprint requests to Dr. Jean-Louis Chiasson,
insulin resistance is a major risk factor for the develop-
Research Centre–CHUM–Hoˆtel-Dieu, 3850 St. Urbain St., Rm. 8-202, Montreal
ment of type 2 diabetes (15,16). In a prospective study of
(Quebec) H2W 1T7, Canada. E-mail:
[email protected].
Received for publication 20 March 2004 and accepted in revised form 3 June
Pima Indians, Lillioja et al. (15) studied the relative roles of
obesity, insulin resistance, and -cell dysfunction in the
This article is based on a presentation at a symposium. The symposium and
the publication of this article were made possible by an unrestricted educa-
development of type 2 diabetes in subjects with normal
tional grant from Servier.
glucose tolerance (
n ⫽ 151) or impaired glucose tolerance
FSIVGTT, frequently sampled intravenous glucose tolerance test; IGT,
impaired glucose tolerance.
⫽ 49). All subjects had body composition assess-
2004 by the American Diabetes Association.
ment, oral and intravenous glucose tolerance tests, and a
DIABETES, VOL. 53, SUPPLEMENT 3, DECEMBER 2004
J.-L. CHIASSON AND R. RABASA-LHORET
TABLE 1Intervention studies on the prevention of type 2 diabetes
Studies (ref. no.)
Lifestyle modifications
Da Qing (1997) (9)
Diet and/or exercise
Diet and exercise
Diet and exercise
Drug interventions
TRIPOD (2002) (13)
STOP-NIDDM (2002) (12)
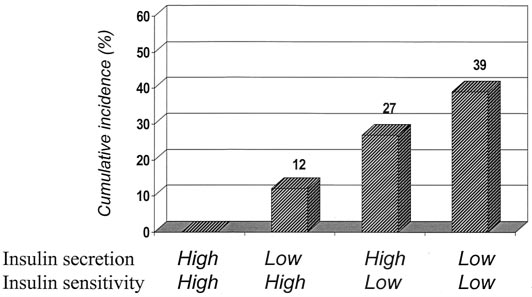
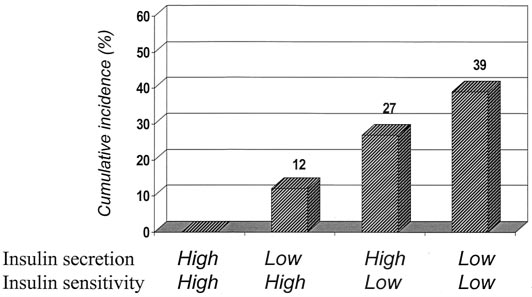
hyperinsulinemic-euglycemic clamp study. The insulin re-
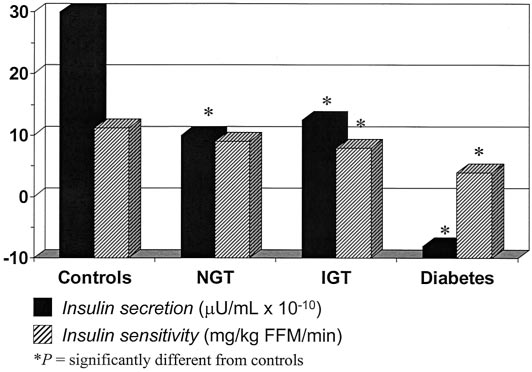
while only those with IGT also had a significant reduction
sistance was the strongest single predictor for diabetes,
in insulin sensitivity compared with appropriate control
with a 27% cumulative incidence of diabetes over 6 years
(Fig. 2). This study provides evidence that impairment of
(Fig. 1). The acute plasma insulin response alone was not
-cells can occur before insulin resistance is detectable.
a significant predictor for diabetes. However, the combi-
However, both seem to be present by the time hypergly-
nation of insulin resistance and insulin response provided
cemia appears. Other reports have confirmed those obser-
the strongest predictor with a 6-year cumulative incidence
vations in offspring of two parents with type 2 diabetes
of diabetes of 39%. They concluded that insulin resistance
(17) or first-degree relatives of someone with type 2
was a major risk factor for the development of diabetes,
diabetes (21,22). Taken together, these observations pro-
with insulin secretion being an additional but weaker risk
vide strong evidence that -cell dysfunction is already
factor (15). Warram et al. (17) followed for 25 years 155
present in normal glucose-tolerant individuals genetically
offspring of couples who both had type 2 diabetes. Sub-
predisposed to develop type 2 diabetes. It also suggests
jects who developed diabetes had insulin resistance ⬎10
that insulin resistance can be attributed mostly to obesity
years before they developed the disease. However, they
and/or reduced physical fitness. This is suggested by a
found no evidence of an insulin secretion defect several
number of studies indicating that weight loss will reverse
years before the development of diabetes. In a few sub-
the insulin resistance (23–25) without normalizing the
jects, they noticed a gradual decline in insulin secretory
insulin secretory defect.
capacity before the onset of diabetes. These observations
In interpretation of these observations, it is most often
argue in favor of insulin resistance as the primary defect in
lost to the observers that insulin sensitivity is itself a
the development of diabetes. The major argument support-
determinant of the magnitude of the insulin response.
ing insulin resistance as a primary genetic factor leading to
Thus, insulin-resistant subjects have a greater insulin
diabetes is the observations that its appearance precedes
response to glucose, whereas insulin-sensitive subjects
detection of impaired -cell function (17,18). However,
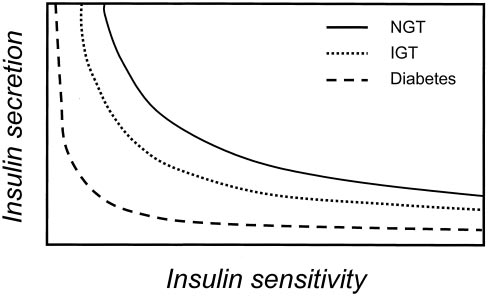
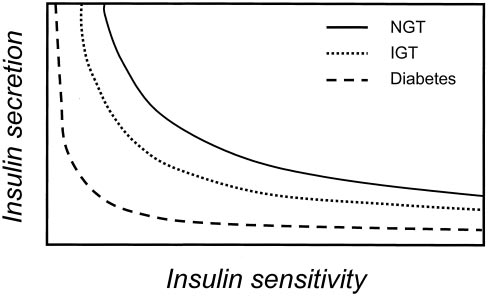
have a smaller insulin response (26). The relationship
Gerich (19) claims that the influence of obesity needs to be
between insulin sensitivity and insulin secretion has been
taken into consideration and that people at risk for diabe-
described as a hyperbolic relationship. The nature of this
tes are not insulin resistant relative to appropriate control,
relationship implies that the product of insulin sensitivity
i.e., obese control! Moreover, although many obese sub-
and insulin response is a constant at a given degree of
jects are insulin resistant, most of them do not progress to
glucose tolerance (26) (Fig. 3). Therefore, when insulin
sensitivity varies, a proportional and reciprocal alteration
Vaag et al. (20) studied monozyzotic twins, one of whom
already had diabetes and one of whom had either normalglucose tolerance or IGT. Those with normal glucosetolerance or IGT had decreased first-phase insulin release,
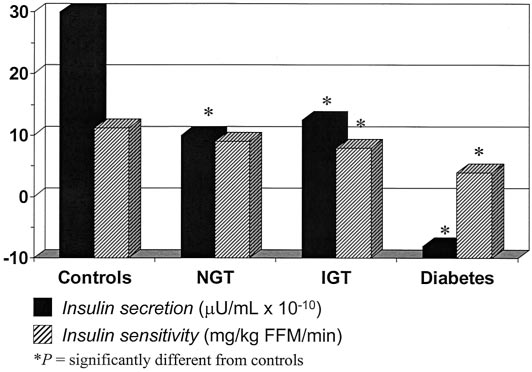
FIG. 2. Insulin secretion and insulin sensitivity in monozygotic twins
FIG. 1. Six-year cumulative incidence of diabetes according to insulin
with normal glucose tolerance, impaired glucose tolerance, or diabetes.
sensitivity and insulin secretion. Adapted from Lillioja et al. (15).
Adapted from Vaag et al. (20).
DIABETES, VOL. 53, SUPPLEMENT 3, DECEMBER 2004
PREVENTION OF TYPE 2 DIABETES
ported by a recent study from Ferrannini et al. (33), whodemonstrated a defect in glucose sensitivity and insulinrelease in IGT subjects that predominated over insulinresistance.
In summary, insulin resistance seems to be explained
mostly by the presence of obesity. In fact, weight reduc-tion is associated with a normalization of insulin sensitiv-ity. On the other hand, -cell dysfunction is present yearsbefore glucose intolerance appears, and no interventionhas yet been able to correct this abnormality. This wouldsupport the concept that -cell failure is the primarydefect leading to the development of diabetes. Insulinresistance, acquired though obesity, and decreased physi-cal activity will further accelerate the progression to
FIG. 3. Schematic representation of hyperbolic relationship between
diabetes. This would explain the epidemic explosion of
insulin sensitivity and insulin secretion in subjects with different
diabetes in a world getting fatter and more sedentary.
glucose tolerance. NGT, normal glucose tolerance. Adapted from Kahn
et al. (26).
THE PREVENTION OF DIABETES: AN EFFECT ON
in insulin output has to occur for glucose tolerance toremain constant. As such, the product of insulin sensitivity
INSULIN SENSITIVITY AND/OR INSULIN SECRETION?
and insulin response provides a better measurement of
The major intervention trials on the prevention of diabetes
-cell function rather than the insulin or C-peptide re- are relatively recent, and analysis of the data is ongoingsponse examined in isolation. When this relationship be-
(Table 1). For that reason, we still do not have published
tween insulin sensitivity and insulin secretion is taken into
data on insulin sensitivity and insulin secretion for those
consideration, it becomes evident that subjects who are at
high risk of developing type 2 diabetes have demonstrated
A number of observational studies suggested that
-cell dysfunction at a time when they still have normal weight loss and physical activity could reduce the risk ofglucose tolerance. The first-degree relatives of patients
developing diabetes (34 –36). Three prospective interven-
with diabetes (27–29) and subjects with IGT (30,31) can all
tion studies have now confirmed the efficacy of lifestyle
be shown to have -cell dysfunction that is reduced
modification, including diet and exercise (9 –11), in reduc-
relative to the degree of insulin sensitivity. These cross-
ing the risk of type 2 diabetes in a high-risk population
sectional data are also supported by a longitudinal study in
with IGT. The Da Qing Study (37) was the first to show in
Pima Indians who had normal glucose tolerance at base-
577 subjects with IGT that diet and/or exercise could
line (32). Those who developed diabetes had a 78% decline
lower the risk of diabetes by 39% over 6 years. Using
in insulin secretion and a 14% decrease in insulin sensitiv-
homeostasis model assessment (HOMA), the authors have
ity (Fig. 4). On the other hand, those who did not develop
looked at the effect of insulin resistance and -cell dys-
diabetes also had an 11% decrease in insulin sensitivity,
function on the incidence of diabetes in a subgroup of
but the change was associated with a 30% increase in
patients (n ⫽ 284) in the four treatment groups (38). Both
insulin secretion. In this latter group, the relationship
insulin resistance and impaired insulin secretion at base-
between insulin sensitivity and insulin release was main-
line were significantly associated with the development of
tained. Close examination of these responses therefore
diabetes at follow up (P ⬍ 0.05, P ⬍ 0.01). When the
show the presence of impaired -cell function in subjects
subgroup was split in two, according to insulin resistance
at risk of developing diabetes, even when these subjects
and insulin secretion, those who were less insulin resistant
still have normal glucose tolerance. This is further sup-
responded better to lifestyle modification. Those who hadgreater insulin secretion, however, did not respond signif-icantly better to the intervention. The missing analysis iswhether intervention per se had any effect on insulinresistance and insulin secretion. Other studies wouldsupport an effect of diet and exercise on insulin resistance(23–25). An effect of lifestyle modification on insulinsecretion, however, is unlikely (24).
In the Finnish Diabetes Prevention Study (DPS) (10),
lifestyle modification in subjects (n ⫽ 522) with IGTresulted in a 58% reduction in the risk of diabetes. Thefrequent sampling intravenous glucose tolerance test(FSIVGTT) was done at baseline and repeated at 4 years.
At 4 years, the insulin sensitivity tended to be higher in theintervention group (P ⫽ 0.067) (39). There was a strongcorrelation between weight change and change in insulinsensitivity. In fact, those who lost weight in the controlgroup were also protected against diabetes. Although no
FIG. 4. Changes in -cell function and in insulin sensitivity at low
improvement was observed in insulin secretion in the
insulin concentration with the development of glucose intolerance.
Adapted from Weyer et al. (32).
intervention group, it declined significantly in the control
DIABETES, VOL. 53, SUPPLEMENT 3, DECEMBER 2004
J.-L. CHIASSON AND R. RABASA-LHORET
TABLE 2Average annual incidence rates of diabetes in tertiles of the troglitazone group defined by changes in insulin sensitivity or by changesin IVGTT insulin between baseline and 3 months on trial
Change in SI
Annual diabetes incidence (%)
Change in IVGTT insulin area
⫺1,238 to ⫺3,053
⫺3,160 to ⫺193,64
Annual diabetes incidence (%)
Data are from 108 women randomized to troglitazone who had IVGTTs at baseline and 3 months on trial. P values among subgroups bylog-rank test. *P ⬍ 0.01, †P ⬍ 0.05, and ‡P ⬍ 0.001 vs. diabetes incidence in placebo group (log-rank test). Adapted from Buchanan et al. (42).
group. They concluded that weight change resulted in a
in insulin resistance offers a protective effect on the -cell
significant improvement in insulin sensitivity, which was
and, therefore, has a preservative effect on the -cell
associated with a reduction in the incidence of diabetes.
function. Furthermore, all interventions on the prevention
Insulin secretion, on the other hand, remained constant in
of diabetes so far could not show any effect on -cell
those who were able to lose weight (39).
function. At best, it can preserve the insulin secretion
At present, no data on insulin sensitivity and insulin
capacity by decreasing the stress on the -cells. This
secretion in relation to lifestyle modification have been
would support the concept that the major genetic defect in
published for the Diabetes Prevention Program (40,41); it
the development of diabetes is related to -cell dysfunction.
is very likely that observations similar to those of the DPSwill be seen. In addition, no data for the metformin treatment
group have yet been published.
1. King H, Aubert RE, Herman WH: Global burden of diabetes, 1995–2025:
The effects of troglitazone on insulin sensitivity and
prevalence, numerical estimates, and projections. Diabetes Care 21:1414 –
insulin secretion were tested at baseline and 12 weeks in
the TRIPOD study using the FSIVGTT (42). In this study,
2. Geiss LS, Herman WH, Smith PJ: Mortality in non-insulin-dependent
266 Hispanic women with a history of gestational diabetes
diabetes. In Diabetes in America. Baltimore, MD, National Institutes of
were randomized to placebo or troglitazone 400 mg o.d.
Health, 1995, p. 233–255
3. Alberti KGMM: The costs of non-insulin-dependent diabetes mellitus.
Treatment with troglitazone reduced the risk of diabetes
Diabet Med 14:7–9, 1997
by 50% over 30 months. Insulin sensitivity improved sig-
4. American Diabetes Association: Economic consequences of diabetes mel-
nificantly at 12 weeks in the troglitazone treatment group
litus in the US in 1997. Diabetes Care 21:296 –309, 1998
(2.60 ⫾ 1.67 to 3.76 ⫾ 2.27; P ⬍ 0.0001). On the other hand,
5. Gerich JE: The genetic basis of type 2 diabetes mellitus: impaired insulin
secretion versus impaired insulin sensitivity.
troglitazone did not have a significant effect on acute
Endocr Rev 19:491–503, 1998
6. Olefsky JM, Farguhar JW, Reaven GM: Relationship between fasting
insulin release (P ⫽ 0.10). To examine the relationship
plasma insulin level and resistance to insulin-mediated glucose uptake in
between early changes in insulin sensitivity and subse-
normal and diabetic subjects. Diabetes 22:507, 1973
quent protection from diabetes, the troglitazone group was
7. Lillioja S, Bogardus C: Obesity and insulin resistance: lessons learned from
divided into tertiles defined by changes in insulin sensitiv-
the Pima Indians. Diabete Metab Rev 4:517–540, 1988
8. Kahn SE, Porte D Jr: Pathophysiology of type II diabetes mellitus. In
ity or by changes in insulin area under the curve in
Diabetes Mellitus. Porte D Jr, Sherwin RS, Eds. Stamford, CT, Appleton &
response to intravenous glucose. Based on insulin sensi-
Lange, 1996, p. 487–512
tivity, the incidence of diabetes was significantly reduced
9. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Lin J, Xiao JZ, Cao HB,
in the second tertile as well as the third tertile (Table 2).
Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH,Howard BV: The Da Qing IGT and Diabetes Study: effects of diet and
Based on insulin secretion, however, the incidence of
exercise in preventing NIDDM in people with impaired glucose tolerance.
diabetes was not reduced in the second tertile, but only in
Diabetes Care 20:537–544, 1997
the third tertile. Furthermore, those who did not have an
10. Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-
improvement in insulin sensitivity were not protected
Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M,
from diabetes. They concluded that the effect of the drug
Salminen V, Uusitupa M: Prevention of type 2 diabetes mellitus by changesin lifestyle among subjects with impaired glucose tolerance. N Engl J Med
on the incidence of diabetes was due primarily to an effect
344:1343–1350, 2001
on insulin sensitivity. This effect resulted in a protective
11. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM,
and preservative effect on the pancreatic -cell function.
Walker EA, Nathan DM: Reduction in the incidence of type 2 diabetes with
We are currently analyzing the effect of acarbose on
lifestyle intervention or metformin. N Engl J Med 346:393– 403, 2002
12. Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M:
insulin sensitivity and -cell function in the STOP- NIDDM
Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM
Trial. These data have not yet been published.
randomised trial. Lancet 359:2072–2077, 2002
13. Buchanan TA, Xiang AH, Peters RK, Kjos SL, Berkowitz K, Marroquin A,
Goico J, Ochoa C, Azen SP: Response of pancreatic beta-cells to improved
insulin sensitivity in women at high risk for type 2 diabetes. Diabetes
Based on observational studies as well as on prospective
49:782–788, 2000
14. Kahn SE: The relative contributions of insulin resistance and beta-cell
intervention trials, it is suggested that the prevention of
dysfunction to the pathophysiology of type 2 diabetes. Diabetologia
diabetes is due to a primary effect on insulin sensitivity
rather than on insulin secretion. However, such a decrease
15. Lillioja S, Mott DM, Spraul M, Ferraro R, Foley JE, Ravussin E, Knowler
DIABETES, VOL. 53, SUPPLEMENT 3, DECEMBER 2004
PREVENTION OF TYPE 2 DIABETES
WC, Bennett PH, Bogardus C: Insulin resistance and insulin secretory
months after pregnancies complicated by gestational diabetes. Diabetes
dysfunction as precursors of non-insulin-dependent diabetes mellitus.
48:2430 –2436, 1999
N Engl J Med 329:1988 –1992, 1993
30. Larsson H, Ahren B: Islet dysfunction in obese women with impaired
16. Chaix C, Durand-Zeleski I: Impact e´conomique des strate´gies de prise en
glucose tolerance. Metabolism 45:502–509, 1996
charge du diabe te gestationnel. Diabete Metab 23 (Suppl. 5):40 – 47, 1997
31. Cavaghan MK, Ehrmann DA, Byrne MM, Polonsky KS: Treatment with the
17. Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR: Slow glucose
oral antidiabetic agent troglitazone improves beta cell responses to
removal rate and hyperinsulinemia precede the development of type II
glucose in subjects with impaired glucose tolerance. J Clin Invest 100:
diabetes in the offspring of diabetic parents. Ann Intern Med 113:909 –915,
32. Weyer C, Bogardus C, Mott DM, Pratley RE: The natural history of insulin
18. Lillioja S, Mott DM, Howard BV, Bennett PH, Yki-Jarvinen H, Freymond D,
secretory dysfunction and insulin resistance in the pathogenesis of type 2
Nyomba BL, Zurlo F, Swinburn B, Bogardus C: Impaired glucose tolerance
diabetes mellitus. J Clin Invest 104:787–794, 1999
as a disorder of insulin action: longitudinal and cross-sectional studies in
33. Ferrannini E, Gastaldelli A, Miyazaki Y, Matsuda M, Pettiti M, Natali A,
Pima Indians. N Engl J Med 318:1217–1225, 1988
Mari A, DeFronzo RA: Predominant role of reduced beta-cell sensitivity to
19. Gerich JE: Is insulin resistance the principal cause of type 2 diabetes?
glucose over insulin resistance in impaired glucose tolerance. Diabetolo-
Diabetes Obes Metab 1:257–263, 1999
gia 46:1211–1219, 2003
20. Vaag A, Henriksen JE, Madsbad S, Holm N, Beck-Nielsen H: Insulin
34. Manson JE, Rimm EB, Stampfer MJ, Colditz GA, Willett WC, Krolewski AS,
secretion, insulin action, and hepatic glucose production in identical twins
Rosner B, Hennekens CH, Speizer FE: Physical activity and incidence of
discordant for non-insulin-dependent diabetes mellitus. J Clin Invest
non-insulin-dependent diabetes mellitus in women. Lancet 338:774 –778,
95:690 – 698, 1995
21. Pimenta W, Korytkowski M, Mitrakou A, Jenssen T, Yki-Jarvinen H, Evron
35. Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennek-
W, Dailey G, Gerich J: Pancreatic beta-cell dysfunction as the primary
ens CH: A prospective study of exercise and incidence of diabetes among
genetic lesion in NIDDM: evidence from studies in normal glucose-tolerant
US male physicians. JAMA 268:63– 67, 1992
individuals with a first-degree NIDDM relative. JAMA 273:1855–1861, 1995
36. Wei M, Gibbons LW, Mitchell TL, Kampert JB, Lee CD, Blair SN: The
22. van Haeften TW, Dubbeldam S, Zonderland ML, Erkelens DW: Insulin
association between cardiorespiratory fitness and impaired fasting glucose
secretion in normal glucose-tolerant relatives of type 2 diabetic subjects:
and type 2 diabetes mellitus in men. Ann Intern Med 130:89 –96, 1999
assessments using hyperglycemic glucose clamps and oral glucose toler-
37. Cominacini L, Garbin U, Pastorino AM, Campagnola M, Fratta Pasini A,
ance tests. Diabetes Care 21:278 –282, 1998
Davoli A, Rigoni A, Lo Cascio V: Effects of troglitazone on in vitro
23. Bak JF, Moller N, Schmitz O, Saaek A, Pedersen O: In vivo insulin action
oxidation of LDL and HDL induced by copper ions and endothelial cells.
and muscle glycogen synthase activity in type 2 (non-insulin-dependent)
Diabetologia 40:165–172, 1997
diabetes mellitus: effects of diet treatment. Diabetologia 35:777–784, 1992
38. Li G, Hu Y, Yang W, Jiang Y, Wang J, Xiao J, Hu Z, Pan X, Howard BV,
24. Beck-Nielsen H, Pedersen O, Lindskov HO: Normalization of the insulin
Bennett PH: Effects of insulin resistance and insulin secretion on the
sensitivity and the cellular insulin binding during treatment of obese
efficacy of interventions to retard development of type 2 diabetes mellitus:
diabetics for 1 year. Acta Endocrinol (Copenh) 90:103–112, 1979
the DA Qing IGT and Diabetes Study. Diabetes Res Clin Pract 58:193–200,
25. Freidenberg GR, Reichart D, Olefsky JM, Henry RR: Reversibility of
defective adipocyte insulin receptor kinase activity in non-insulin-depen-
39. Uusitupa M, Lindi V, Louheranta A, Salopuro T, Lindstrom J, Tuomilehto J:
dent diabetes mellitus: effect of weight loss. J Clin Invest 82:1398 –1406,
Long-term improvement in insulin sensitivity by changing lifestyles of
people with impaired glucose tolerance: 4-year results from the Finnish
26. Kahn SE, Prigeon RL, McCulloch DK, Boyko EJ, Bergman RN, Schwartz
Diabetes Prevention Study. Diabetes 52:2532–2538, 2003
MW, Neifing JL, Ward WK, Beard JC, Palmer JP: Quantification of the
40. The Diabetes Prevention Program Research Group: The Diabetes Preven-
relationship between insulin sensitivity and beta-cell function in human
tion Program: baseline characteristics of the randomized cohort. Diabetes
subjects: evidence for a hyperbolic function. Diabetes 42:1663–1672, 1993
Care 23:1619 –1629, 2000
27. Ward WK, Johnston CL, Beard JC, Benedetti TJ, Halter JB, Porte D, Jr:
41. The Diabetes Prevention Program Research Group: The Diabetes Preven-
Insulin resistance and impaired insulin secretion in subjects with histories
tion Program (DPP): description of lifestyle intervention. Diabetes Care
of gestational diabetes mellitus. Diabetes 34:861– 869, 1985
25:2165–2171, 2002
28. Ryan EA, Imes S, Liu D, McManus R, Finegood DT, Polonsky KS, Sturis J:
42. Buchanan TA, Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, Ochoa
Defects in insulin secretion and action in women with a history of
C, Tan S, Berkowitz K, Hodis HN, Azen SP: Preservation of pancreatic
gestational diabetes. Diabetes 44:506 –512, 1995
beta-cell function and prevention of type 2 diabetes by pharmacological
29. Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK: Antepartum
treatment of insulin resistance in high-risk hispanic women. Diabetes
predictors of the development of type 2 diabetes in Latino women 11–26
51:2796 –2803, 2002
DIABETES, VOL. 53, SUPPLEMENT 3, DECEMBER 2004
Source: http://www.e-asta.cn/asta_pdf/Prevention_%20of_%20type2_%20diabetes.pdf
12690 • The Journal of Neuroscience, September 17, 2014 • 34(38):12690 –12700 Serotonin Affects Movement Gain Control in the Spinal Cord Kunlin Wei,1 Joshua I. Glaser,2,3,4,5 Linna Deng,1 Christopher K. Thompson,5,6 Ian H. Stevenson,2,3,4,5 Qining Wang,1Thomas George Hornby,2,3,4,5,6 Charles J. Heckman,2,3,4,5 and Konrad P. Kording2,3,4,51Department of Psychology, Peking University, Beijing, China 100871, Departments of 2Physical Medicine and Rehabilitation, 3Physiology, and 4AppliedMathematics, Northwestern University, Chicago, Illinois 60611, 5Rehabilitation Institute of Chicago, Chicago, Illinois 60611, and 6Department ofKinesiology and Nutrition, University of Illinois at Chicago, Chicago, Illinois 60607
Ursachen und Therapie der Spastik bei Multipler Sklerose MS und Cannabis Vortrag auf dem Symposium am 26. Mai 2001 von Dr. med. Wolfgang Weihe Meine sehr verehrten Damen und Herren, nachdem Herr Kollege Keller das Schokoladenplätzchen halfen schlag- Thema „Therapie der Spastik" so klar artig und mein Freund überstand die und verständlich dargestellt hat, möch-