Dec2003community.pdf
54. Summerson JS, Konen JC, Dignan MB. Race related differences in metabolic control among
66. Robinson CH, Lawler MR, Chenoweth WL,
et al. Normal and Therapeutic Nutrition. 7th ed New
adults with diabetes.
S Afr Med J 1992;
85: 953-956.
York: Macmillan, 1986: 759.
55. Rasmussen OW, Gregersen S, Dorup J,
et al. Day to day variation of blood glucose and
67. Thornburn AW, Brand JC, Truswell AS. The glycaemic index of foods.
Med J Aust 1986;
144:
insulin responses in type 2 diabetic subjects after starch-rich meal.
Diabetes Care 1992;
15: 522-
68. Jackson RA, Blick PM, Matthews JA,
et al. Comparison of peripheral glucose uptake after oral
56. Castillo MJ, Scheen AJ, Jandrian B,
et al. Relationship between metabolic clearance rate of
glucose loading and a mixed meal.
Metabolism 1983;
32: 706-710.
insulin and body mass index in a female population ranging from anorexia nervosa to severe
69. Porte D, Sherwin RS.
Ekkenberg and Rifkin's Diabetes Mellitus: Theory and Practice. 5th ed. USA:
obesity.
Int J Obes Relat Metab Disord 1994;
18: 47-53.
Appleton and Lange, 1997: 366.
57. Marion JF. Nutritional care in diabetes mellitus and reactive hypoglycemia. In: Krause MV,
70. Wolever TMS, Jenkins DJA, Jenkins AL. The glycemic index: methodology and clinical
Mahan LK, eds
. Krause's Food, Nutrition and Diet Therapy. 8th ed. Philadelphia: WB Saunders,
implications.
Am J Clin Nutr 1991;
54: 846-854.
1984: 479-509.
71. Bantle JP, Laine DC, Castle GW,
et al. Postprandial glucose and insulin responses to meals
58. Weyman-Daum M, Fort P, Recker B,
et al. Glycemic response in children with insulin-
containing different carbohydrates in normal and diabetic subjects.
N Engl J Med 1983;
309: 7-
dependent diabetes mellitus after high- or low-glycemic-index breakfast.
Am J Clin Nutr 1987;
46: 798-803.
72. Nuttal FQ, Moorandian AD, DeMarais R,
et al. The glycemic effect of different meals
59. Jenkins DJA, Wolever TMS, Jenkins AL,
et al. The glycaemic index of foods tested in diabetic
approximately isocaloric and similar in protein, carbohydrate and fat content as calculated
patients; a new basis for carbohydrate exchange favouring the use of legumes.
Diabetologia
using the ADA exchange lists.
Diabetes Care 1983;
6: 432-435.
1983; 24: 257-264.
73. Gannon MC, Nuttal FQ, Krezowski PA,
et al. The serum insulin and plasma glucose response
60. Inoescu-Tîrgoviste C, Popa E, Sîntu E,
et al. Blood glucose and plasma insulin responses to
to milk and fruit products in type 2 (non-insulin dependant) diabetic patients.
Diabetologia
various carbohydrates in type 2 (non-insulin dependant) diabetes.
Diabetologia 1983; 14: 80-84.
1986;
29: 784-791.
61. Venter CS, Vorster HH, Van Rooyen A,
et al. Comparison of the effects of maize porridge
74. Laine DC, Thomas W, Levitt MD,
et al. Comparison of predictive capabilities of diabetic
consumed at different temperatures on blood glucose, insulin and acetate levels in healthy
exchange lists and glycemic index of foods.
Diabetes Care 1987;
10: 387-394.
volunteers.
South African Journal of Food Science and Nutrition 1990;
2: 2-5.
75. Reaven GM, Chen Y-DI, Golay A,
et al. Documentation and hyperglucagonemia throughout
62. Truswell AS. Glycaemic index of foods.
Eur J Clin Nutr 1992;
46S: S91 - S101.
the day in nonobese and obese patients with non-insulin dependant diabetes mellitus.
J Clin
63. Thompson DG, Wingate DL, Thomas M,
et al. Gastric emptying as a determinant of the oral
Endocrinol Metab 1987;
64: 106-110.
glucose tolerance test.
Gastroenterology 1982;
82: 51-55.
76. Coulston AM, Hollenbeck CB, Swiskocki ALM,
et al. Effect of source of dietary carbohydrate
64. Krezowski PA, Nuttal FQ, Gannon MC,
et al. Insulin and glucose responses to various starch-
on plasma glucose and insulin responses to mixed meals in subjects with NIDDM.
Diabetes
containing foods in type 2 diabetic subjects.
Diabetes Care 1987;
10: 205-212.
Care 1987;
10: 395-400.
65. Hunt SM, Groff JL.
Advanced Nutrition and Human Metabolism. New York: West, 1990.
77. Hollenbeck CB, Coulston AM, Reaven GM. Glycemic effects of carbohydrates: a different
perspective.
Diabetes Care 1986;
9: 641-647.
A community-based growth monitoring model to
complement facility-based nutrition and health practices in
a semi-urban community in South Africa
Serina E Schoeman, Muhammad A Dhansay, John E Fincham, Ernesta Kunneke, A J Spinnler Benadé
Objective. To assess the feasibility of a community-based
monitoring system. The community-based growth
growth monitoring model in alleviating the shortcomings in
monitoring system increased growth monitoring coverage of
health and nutrition surveillance of preschool-aged children
preschool children by more than 60%. Attendance of
as practised by the health services.
preschool children aged 12 months and older varied between
Method. Baseline community and health facility practice
10% and 14% at the health facility practice compared with 80
surveys and interactive workshops with the community were
- 100% in the community-based growth monitoring system.
conducted before the study. Eleven women were trained to
This made the system more conducive for monitoring and
drive the community-based growth monitoring project.
targeting of malnourished children for health and nutrition
Health facility practice information was collected before and
after establishment of the community-based growth
Conclusion. The community-based growth monitoring model
monitoring system.
demonstrated that community participation and mobilisation
Results. The health facility practice reached 12 - 26% of the
can increase preschool child growth monitoring coverage
preschool population per month compared with 70 - 100%
extensively and contribute to improved health and nutrition
per 3-week session in the community-based growth
Nutritional Intervention Research Unit, Medical Research Council, Parow, W Cape
Parasitology Group, Medical Research Council, Parow, W Cape
Serina E Schoeman, BA Cur
John E Fincham, BVSc
Muhammad A Dhansay, FCP
Department of Dietetics, University of the Western Cape, Bellville, W Cape
A J Spinnler Benadé, DSc
Ernesta Kunneke, MSc
Nov./Dec. 2003, Vol. 16, No. 4
SAJCN

Inadequacies in preschool child growth monitoring (GM)
perceptions of nutrition, while the CBGM model was the action
coverage at health facility practices (HFPs) have been described
component that developed after analysis of the baseline survey
in several studies.1,2 Maternal perceptions of HFPs, and service
data presented at a ZOPP (Ziel Orientierte Projekt Planung or
providers emphasising a curative approach are key factors
objective oriented project planning) workshop.10 The baseline
influencing health care coverage of the preschool child. In the
survey and the CBGM model will be discussed simultaneously
absence of disease or clinical symptoms, mothers regard the
to illustrate the impact of the model.
childhood immunisation schedule as the main reason forvisiting the HFP. The curative approach emphasised by the
HFP fosters the perception among people that health care
The study population consisted of ± 250 children aged 0 - 72
equals curative care, which is a fallacy.3 Health care is often
months and their mothers, living in Langebaan, a small urban
associated with ‘the provision of doctors, drugs, ambulances
town on the west coast of the Western Cape, 136 km from Cape
and hospitals', while preventive measures are less appreciated.3
Town. It has a population of approximately 4 000 people, and a
After primary completion of the childhood immunisation
preschool population of ± 350 children. Children were
schedule at 9 months, GM and preschool attendance decline
identified for the project using registrations from the HFP, the
drastically at HFPs. HFPs are biased in favour of children
community survey and birth records. The annual birth rate is
between 0 and 24 months of age, and do not assess height-for-
approximately 45 - 50 births and the prevalence of low birth
weight (less than 2 500 g) remains at between 17% and 22%.
Underweight, which peaks after 18 months, and stunting are
Most inhabitants earn their living through fishing and have a
often not detected because of sporadic attendance and poor
low income. The town is also a big tourist attraction. A small,
GM at HFPs.1,2,4,5 Strategies such as GM and growth promotion,
richer group in the town generates income mainly through
oral rehydration therapy, breast-feeding, food supplementation
accommodating tourists in holiday homes or guesthouses.
and education of women to promote and strengthen the healthfacility-based nutrition component, are therefore seriously
Community baseline survey
The survey was conducted over 7 months.
A community-based growth monitoring (CBGM) system in
rural areas with inadequate health services appears to be a
viable cost-effective option for monitoring growth, nutritional
Eleven women from the local community were trained by staff
status and health of children.9 To determine whether such a
of the Nutritional Intervention Research Unit (NIRU) of the
model could also be implemented in an urban setting with
Medical Research Council (MRC) to administer questionnaires
established health systems, required further investigation. An
to determine caregivers' perceptions on disease, nutrition and
opportunity to pursue this issue arose when the Child Welfare
health practices. The information was obtained from parents or
Society requested assistance from the Nutritional Intervention
guardians of preschool children during house-to-house visits.
Research Unit (NIRU) of the Medical Research Council (MRC),
Breast-feeding information was obtained in a separate study.
because of perceived problems of malnutrition amongpreschool children in towns on the west coast, South Africa.
Langebaan was selected as a suitable community that could beresearched to identify possible causal factors for the suspected
The women's training also involved anthropometry and GM.
nutritional situation. The purpose of this study was to
Children were weighed with minimal clothing on an electronic
determine whether a CBGM model could be established in an
load cell scale to the nearest 0.05 kg, and height and length
urban setting to alleviate shortcomings of the local HFP in
were measured to the nearest 0.1 cm using wooden measuring
terms of health and nutrition surveillance of preschool
boards. Recumbent length for children under 2 years old, and
measurements in the standing position for children 2 years andolder were obtained.11,12
A calibrated 10 kg weight was used to assess the accuracy of
Materials and methods
the scales before GM sessions.
Study design
A member of the research team randomly selected children
To develop the CBGM model a cross-sectional baseline survey
for cross-checking. Anthropometric information was used to
was done and the results were used in conjunction with the
calculate z-scores using Epi-Info version 6.04.
community's perceptions of priority needs. The baseline surveycomprising community-based and health facility-based
Health facility practices survey
components, was conducted to assess preschool children's
The survey comprising preschool children attending the HFP
nutritional status, nutrition and health practices and maternal
was conducted over 12 months. The HFP survey ran
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN
concurrently with the CBGM model for the last 5 months of the
immunisation schedule identified from the RTHC, complaints
year. Information on preschool child attendance, disease
from mothers of a child being sick or chronically ill, and
prevalence and health and nutrition practices was obtained
suspected problems of child neglect or abuse. The
from the professional nurse as part of the information routinely
infrastructure of the CBGM system allowed for additional
collected at the HFP.
activities such as nutrition and health education, biochemical
The information was recorded on structured sheets specially
and parasitological analysis, management of iron deficiency
drawn up by the researcher. Mother's reason for visiting the
and worm infection, and blanket deworming of preschool
HFP, procedures performed, group or individual health
children, which will be reported separately.
education topics and outcomes of visit were recorded for eachchild. Client status such as visitor, first or follow-up visit, was
also indicated. Food supplementation data were obtained froma register held at the HFP and growth plotting practices were
Community baseline survey
observed from children's road-to-health cards (RTHCs).
Maternal reasons for visiting the HFP
Information was calculated monthly by listing items according
Sixty-three per cent of mothers indicated that visiting the HFP
to a coding system.
after completion of the immunisation schedule was onlynecessary if the child was sick, while 17% said they would
ZOPP workshop and the establishment of the
attend for general assessments, information, or weighing
CBGM model
children, and 20% did not deem it necessary at all.
The ZOPP workshop was facilitated by the NIRU as the
process allows maximum involvement, and an equal
Seventy-nine per cent of the mothers initiated breast-feeding,
opportunity for all participants to determine priority needs and
but none of the infants was exclusively breast-fed. Formula
to participate in the planning and implementation of an
feeding was introduced soon after birth and solids from 0.5 -1.3
intervention project. The workshop participants comprised
months of age.
stakeholders from the Departments of Health and Education,the local municipality, non-governmental organisations, health
committees, women's committees, reconstruction and
Maternal perceptions on food supplementation were not
development programme committees, and NIRU staff.
Information collected during the baseline survey was used as astarting point and combined with the participant's information
GM practices and anthropometry
to construct a problem tree, and to develop a causal and
Z-scores below –2 standard deviations (SD) of the National
objective model. This process pre-empted the establishment of
Centre for Health Statistics reference median indicated stunting
the CBGM model.
prevalence rates of 13%, underweight 7% and wasting 2.2%.
Women who were originally trained to do anthropometry
Although 60% of the mothers could recognise a downward
and GM for the baseline community survey, volunteered to
growth curve and associated it with a problem or the child
manage the CBGM system. Five health stations to serve as a
being sick, 81% of the mothers were not familiar with the
facility for preschool CBGM were volunteered by
concept of GM.
representatives of a church, school, crèches, the municipality
HFP survey
and individual families in the community.
Mothers' reasons for visiting the HFP
An appointment system was used to accommodate mothers
in geographical areas nearest to the CBGM points to ensure
Weighing of children was the most important reason for
effective functioning. Appointments were confirmed 1 week
visiting the HFP (41%) and peaked in the 0 - 23-month-old
before the GM sessions. GM was performed 4-monthly, while
group. Ill health was the second most important reason (31%),
nutritionally at-risk children detected during the GM sessions
and peaked in the 12 - 23-month-old group. Childhood
were monitored more than once a month and referred to the
immunisation was the third most important reason (23%), and
HFP for further management. Information was collected and
exceeded ill health only during the first 12 months. Only 5% of
128 entered into a separate folder for each child. A simplified
the parents mentioned health assessments, screenings for
growth chart was used for documentation, plotting and
tuberculosis, or general health information as primary reasons
interpretation of weight to avoid interfering with the RTHC
for visiting the HFP. From 48 months, 6 out of 8 children visit
used at the HFP. Nutritional risk criteria at the CBGM included
the HFP mainly due to ill health. These findings are biased in
weight and height below the 3rd percentile (scale of reference
favour of mothers whose infants were in the 0 - 12-month-age
at the HFP), low birth weight, growth faltering, incomplete
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN

Breast-feeding practices
HFP information regarding breast-feeding practices wasinconsistently recorded. Individual breast-feeding counsellingof mothers was indicated mainly if the mother experiencedproblems with her breasts or with breast-feeding. Exclusivebreast-feeding practices were not indicated.
Protein energy malnutrition scheme food supplement at the
HFP
Results indicated that only 21 out of 36 preschool children(58%) with weight below the 3rd percentile and growthfaltering were entered in the PEM scheme register before, and afurther 11 after, referral from the CBGM system. Of the 32children entered in the 1996 PEM scheme register, 37.5%received the food supplement more than once, while 62.5%received it only once. The results also indicated that only 12.5%received the food supplement at uninterrupted monthlyintervals for ± 3 consecutive months, while 87.5% received less
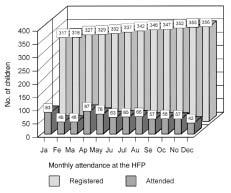
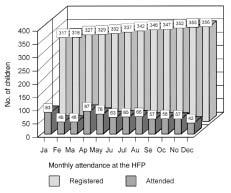
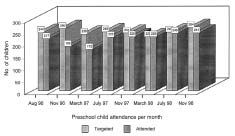
Fig. 1. Coverage of preschool children at the health facility practice
than four food supplements at intervals varying from 2 to 10
(January - December 1996 Langebaan).
GM practices
The ZOPP workshop and the CBGM model
A growth chart study of 51 randomly selected RTHCs
The establishment of the CBGM system that was pre-empted
indicated an average of 5 weight plots between 0 and 6 months
by the ZOPP workshop resulted in sustained GM and health
(1 or no plot per month), 2 plots between 7 and 12 months,
and nutrition surveillance of preschool children. The model
1 plot between 13 and 24 months and 1 or no plots per year
complemented the existing HFP while primary health care was
after the age of 24 months. Height was mainly measured at
managed in the usual way by nursing staff under the
birth and height plotting was not required on the RTHC.
governance of the local authority. Although the CBGM system
Preschool child coverage at the HFP
approach was research-orientated, while the HFP was service-orientated, these findings could serve to enhance policy
Age-specific attendance for preschool children after the age of
12 months varied between 0 and 10, 1 and 8, and 2 and 6 permonth over the respective months and attendance in the 0 - 12-
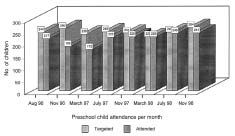
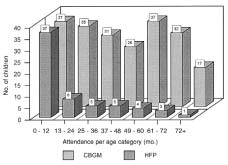
Coverage of preschool children in the CBGM system
month age group tended to decline over the 4-monthly
Preschool coverage in the CBGM system varied between 71%
intervals as the year proceeded (Table I). The preschool
and 100%, sustaining a high average coverage of 80 - 85% over
attendance of 12 - 26% per month was constant throughout the
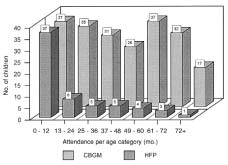
a period of 3 years (Fig. 2). Age-specific attendance after the
year. Average monthly attendance was ± 17% (Fig. 1).
age of 12 months varied between 17 and 37 children per sessionin the CBGM system compared with 1 - 8 children per monthat the HFP (Fig. 3).
Table I. Age-specific coverage of preschool children at the HFP
(April, August, December 1996, Langebaan)
Number of chidren
attending the HFP
* Best attendance pattern.
† Worst attendance pattern.
Fig. 2. Coverage of preschool children in the CBGM system (August1996 - November 1998).
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN
preschool visits, which impact negatively on childhoodnutrition and health as well as health care practices. Thisresults in the HFPs missing the majority of mothers shortlyafter weaning is initiated, and the child's risk of malnutritionand infectious diseases increasing.
HFP and GM practices
Irregular and inaccurate measuring of weight and height andpoor plotting and interpretation of children's weight at theHFPs is a reality.1,2,5,15,16 This results in under-detection ofretarded growth and underweight. Weighing a child withoutplotting is often regarded as synonymous with GM, whilefailing to plot weight deprives nursing staff of the opportunityto promote child growth and development.17,18 Lack of heightassessments deprives stunted children from being targeted for
Fig. 3. Comparison of age-specific attendance at the HFP and in the
appropriate interventions. Discontinuous GM of preschool
CBGM system (August 1996).
children hampers detection and targeting of nutritionally at-
GM practices and anthropometry (November 1996,
risk children, and therefore control of malnutrition and
November 1997 and November 1998)
infectious diseases.
The CBGM system was successful in nutrition surveillance of
Food and iron supplementation and breast-feeding
preschool children as reflected by the results. Average z-scores
at the HFP
of children aged 0 - 12 months for November 1996, 1997 and1998, revealed height-for-age of –1.2 SD, –0.8 SD, and –1.1 SD
The PEM scheme register revealed that the HFP could not
and weight-for-age of –0.4 SD, –0.3 SD, and –0.1 SD. Weight-
successfully detect, target and monitor nutritionally at-risk
for-age z-scores deteriorated further after 18 months, while
preschool children. More than 40% of preschool children with
height-for-age z-scores for preschool children older than 12
growth faltering were not detected and targeted for food
months remained the same. Average height- and weight-for-
supplementation before referral from the CBGM system. The
age z-scores remained consistently below the reference median.
number of children who received less than four food
Annual low birth weight prevalence rates varied between 17%
supplements in 12 months at intervals varying from 2 to 10
and 22%. Stunting prevalence rates among the preschool
months, reflected a failure rate of 87.5%. Failure of 62.5% of the
population varied between 14% and 15%, underweight 5 - 7%,
mothers to return for follow up reflect the low priority of the
and wasting 0.5 - 1%.
PEM scheme programme at the HFP.
Despite well-planned nutrition strategies, the prevalence of
low birth weight remains high (20%), and exclusive breast-feeding practices and iron deficiency among preschool children
Impact of the HFP on nutrition and health care
in Langebaan remain a problem.7,8,13,19,20 Iron requirements for
The prevailing low preschool attendance and low priority
low-birth-weight infants (less than 2.5 kg) or infants born
given to preventive health care should not be allowed as they
before 37 weeks are increased, and iron supplementation from
influence health practices negatively. The CBGM system using
the age of 6 weeks is therefore recommended.21 Guidelines to
women from the community has strengthened preventive
support these recommendations and criteria that are effective
health practices and should therefore not be seen as an
in targeting high-risk pregnant mothers for food and/or iron
obstacle, but rather as a mechanism to improve comprehensive
supplementation need to be communicated clearly for effective
health care delivery. The increased prevalence of tuberculosis
implementation of nutrition programmes at the HFPs.7,8,13,20,22
and HIV infection limits the capacity of nursing staff at the
Nutrition programmes at the HFPs which include the PEM
HFP, which signals a need for such models to enhance social
scheme, have functioned poorly during the past decade and are
130 development, improve nutrition and health care delivery and
largely attributed to poor GM and promotion and sporadic
reduce disease recurrence.3, 8,13,14
preschool coverage for GM.6,7,8,13,20 The HFPs can potentiallyreach all preschool parents during their infants' first 9 months
Sporadic preschool attendance at the HFP
of life to promote nutrition and health through accurate GM as
Nursing staff emphasising curative care and the mothers'
this is part of routine health practice. Despite this, GM and
wrong perceptions of the HFPs contribute largely to sporadic
nutrition practices remain unsatisfactory.23,24 Berg's questioningof operational nutritionists and academics for golden
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN

opportunities lost, misdirected efforts, and ignoring local needs
Briend and Bari25 believe that mothers who recognise
and preferences, is therefore justified.24
abnormal growth might be prompted to take action to preventtheir child's death. The positive effect of the CBGM system in
The ZOPP workshop and impact of the CBGM
growth promotion, as measured by the increased number of
model on nutrition and health care
mothers who reported for GM, is encouraging.
The ZOPP workshop demonstrated that attitudes such as
Advantages of the CBGM model
health professionals claiming the monopoly on healthknowledge and management could be eliminated through
The CBGM model is not a blueprint, but can be recommended
acknowledgement, involvement and joint commitment by
for alleviating shortcomings of HFPs in urban areas. It has the
health professionals, the community and stakeholders in
capacity for large-scale implementation, monitoring, follow-up
programme planning from the initial stage.14 Alternative
and evaluation of programmes on a sustained basis, viz.
solutions for priority needs identified could be debated and
nutrition surveillance, and vitamin A, iron and food
accepted collectively. The NIRU staff of the MRC facilitated the
supplementation. It provides accurate and representative data
establishment of the CBGM system, while the community
on nutritional status and ensures comprehensive detection and
committed itself to addressing priority needs and providing
targeting of high-risk groups for intervention. The cost of
venues to serve as additional health stations for GM and
appointing three women on a part-time basis three times a year
important interventions. Training of women to drive the
varied from R8 000 to R10 000 (10 days), while exposure to
process facilitated transfer of knowledge and skills to the
medico-legal risks or impingement on physical resources was
community; this allowed inadequacies related to GM, health
and nutrition surveillance to be addressed, and facilitated 4-
Although proposals for iron supplementation, screening, and
monthly deworming of children 2 years and older. This
free deworming at HFPs have not yet been implemented either
complemented the HFP in preventive care delivery.
regionally or nationally, the model has successfully facilitated
Although three women could comfortably operate the
screening and management of iron deficiency and mass
CBGM system, training an additional eight ensured continuity
deworming.20,26,27 Mass deworming was found to be of
and future benefits to the community. The sustained CBGM
immediate benefit in high-risk populations for the effective
contributed to the achievement of national health objectives as
prevention of worm infections and the harmful effects of
it encompasses the principle of community participation, an
Trichuris-dysentery syndrome on growth in children.27-30
essential element for the transformation of health services in
Overcrowding, poverty and malnutrition that precipitate
South Africa.8 In this way, the model demonstrated that the
disease are often obscured in well-serviced urban areas with
perceptions of passive recipients of health care could be
the requisite health facilities. Enlisting complementary systems
such as the CBGM model could potentially reduce theepidemic proportions of tuberculosis and HIV infections and
The CBGM model and GM practices
the high prevalence of low birth weight in disadvantaged
The HFP survey ran concurrently with the CBGM model for
urban communities.
the last 5 months of the year and demonstrated differences inGM practices and preschool child coverage for GM between
the two systems before and after establishment of the model.
The 4-monthly GM improved the average coverage of
Considering the results of studies done in Alexandra, the
preschool children by more than 60%. It also improved the
Eastern Cape, Eersterust and KwaZulu-Natal, one would
detection and targeting of nutritionally at-risk and
assume that the situation in Langebaan is not unique, but could
malnourished preschool children by more than 40%.
be indicative of a countrywide situation. The 3-year evaluationof the CBGM model in Langebaan has demonstrated that
This system improved health and nutrition surveillance of
shortcomings in terms of health and nutrition surveillance
the preschool population and indicated that infants were
could be eliminated and the HFP could be complemented with
nutritionally compromised before their birth as reflected by the
guidance and minimal supervision. This is necessary for
high prevalence rate of low birth weight, and mean height-for-
improving the quality of health care of South Africans in
age z-scores below the reference median from birth. It is
believed that stunting reflects serious problems associated withpoor environmental and socioeconomic factors, repeated
The authors acknowledge co-workers Ms Vera Arendse, Mrs
exposure to adverse conditions and chronic malnutrition in
Deirdré Sickle, Mrs Karen Koegelenberg and Miss Lesleen Adonis;
populations. Height assessment, which is neglected, should
statisticians Mrs J A Laubscher and Dr C Lombard; technical
therefore receive more priority. 2,11
support Mr De Wet Marais, Mrs Martelle Marais, Ms Johanna VanWyk, Mr Eldrich Harmse, Ms E Strydom and Mrs A Potgieter; and
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN
Langebaan nutrition monitors Mrs Joan Blake, Mrs Jeremien
12. Jeliffe DB, Jeliffe EFP. Community Assessment with Special Reference to Less Technically Developed
Countries. Oxford University Press,1989.
Blaauw, Mrs Donitha Cupido, Ms Gertrude Engelbrecht, Ms
13. South African Health Review. Durban: Health Systems Trust and Henry J Kaizer Foundation,
Denelda Ocks, Mrs Eileen Ocks, Mrs Rhona Ocks, Mrs Wilna
1996: 141-150.
Pholman, Mrs Doreen Tango and Mrs Daphne Van Der
14. De Villiers MR, De Villiers PJT. Lessons from an academic comprehensive primary health
care centre. S Afr Med J 1996; 86: 1385-1386.
15. Gerein NM, Ross DA. Is growth monitoring worthwhile? An evaluation of its use in three
child health programmes in Zaire. Soc Sci Med 1991; 32: 667-675.
Financial support was received from Sanlam Insurance
16. Kuhn L, Zwarenstein M. Weight information on the ‘Road to Health' card inadequate for
Company and the South African Sugar Association. Special
growth monitoring. S Afr Med J 1990; 78: 495-496.
acknowledgements go to Mr Andy Evans for his sacrifice,
17. World Health Organisation. Guidelines for Training Community Health Workers in Nutrition. 2nd
ed. Geneva: WHO, 1986.
enthusiasm and dedication to the project and the people of
18. Thaver IH, Midhet F, Hussain R. The value of intermittent growth monitoring in Primary
Langebaan and to Dr Henk Tichelaar as independent reviewer.
Health Care Programmes. Journal of the Pakistan Medical Association 1993; 43: 129-133.
Dietary Practices and Iron Status of Preschool Children in Langebaan (Report to Sugar
Association). Parrowvallei: Medical Research Council, 1998; 1-28.
20. South African Vitamin A Consultative Group (SAVACG). Anthropometric, vitamin A, iron
and immunisation coverage status in children 6 - 71 months in South Africa 1994. S Afr Med
1. Chopra M, Sanders D. Growth monitoring — is it a task worth doing in South Africa? S Afr
J 1996; 86: 354-356.
Med J 1997; 87: 875-877.
21. Ireland JD, Power DJ, Woods DL. Primary Care for Paediatric Clinical Nurses. Cape Town:
2. Coetzee DJ, Ferrinho P. Nutritional status of children in Alexandra Township. S Afr Med J
University of Cape Town Press, 1981: 63-67.
1994; 84: 413-415.
22. Dhansay MA, Schoeman SE, Dixon M, Kunneke E, Laubscher JA, Benadé AJS. Risk markers
3. Tarin EU, Thunhurst C. Community participation with provider collaboration. World Health
for low birth weight in women attending an antenatal clinic in Bishop Lavis, a low socio-
Forum 1998;
economic area (abstract). S Afr J Food Sci Nutr 1996; 8: Suppl, 14.
19: 72-75.
4. Yach D, Martin G, Jacobs M, eds Towards a National GOBI-FFF Programme for South Africa
23. Fry J, Hassler J, eds. Primary Health Care 2000. Edinburgh: Churchill Livingstone, 1986:
(Proceedings of the Health Seminar, Cape Town). Parowvallei: Medical Research Council,
Chapters 6, 10.
24. Berg A. Sliding toward nutrition malpractice: time to reconsider and redeploy. Am J Clin Nutr
5. Harrison D, Heese de V, Harker H, Mann MD. An assessment of the ‘Road to Health Card'
1992; 57: 3-7.
based on perceptions of clinic staff and mothers. S Afr Med J 1998; 88: 1424-1428.
25. Briend A, Bari A. Critical assessment of the use of growth monitoring for identifying high
6. Kuhn L, Zwarenstein MF, Katzenelenbogen J. Village health-workers and GOBI-FFF:
risk children in PHC programmes. BMJ 1989; 298: 1607-1611.
evaluation of a rural programme. S Afr Med J 1990; 77: 471-475.
26. Dhansay MA, Sickle DM, Van Stuijvenberg ME, Fincham JE, Schoeman SE, Benadé AJS. Iron
7. Department of Health. Protein Energy Malnutrition Scheme. Western Cape Provincial Update,
deficiency and iron deficiency anaemia in infants, toddlers, school children in the Western
Circular No. 68 of 1996. Provincial Administration, Western Cape.
Cape and KwaZulu-Natal. XVth Meeting of the International Society of Haematology —Africa and European division, Durban, 18-23 Sep 1999: 64.
8. White Paper for the transformation of the health system in South Africa. Government Gazette
382 (17910); 1997: 26-46.
27. Fincham JE, Evans AC, Dhansay MA, Yach D, Schoeman SE. The Case for Mass Deworming.
Durban: Health Systems Trust Update, 1996: 20.
9. Faber M, Oelofse A, Benade AJS. A model for a community-based growth monitoring
system. Afr J Health Sci 1998;
28. Callender JE, Walker SP, Grantham-McGregor SM, Cooper ES. Growth and development four
5: 72-78.
years after treatment for the trichuris dysentery syndrome. Acta Paediatr 1998; 87: 1247-1249.
10. Oelofse A, Muslimuslimatun S, Schultink W. The Ziel Orientierte Projekt Planung (ZOPP)
Procedure. South African Journal of Clinical Nutrition 2000;
29. Savioli L. Treatment of trichuris infection with Albendazole. Lancet 1999; 353: 237-238.
13: 40-43.
11. Gorstein J, Sullivan K, Yip R, et al. Issues in the assessment of nutritional status using
30. Winstanley P. Albendazole for mass treatment of asymptomatic trichuris infections. Lancet
anthropometry. Bull World Health Organ 1994;
1998; 352: 1080-1081.
72: 273-283.
Nov./Dec. 2003, Vol. 16, No. 4 SAJCN
CONTINUING PROFESSIONAL DEVELOPMENT ACTIVITY FOR DIETITIANS
SAJCN CPD activity No 23 – December 2003
You can obtain 3 CPD points for reading the article: "A community-based growth monitoring model to complement facility-based
nutrition and health practices in a semi-urban community in South Africa" and answering the accompanying questions.
This article has been accredited for CPD points for dietitians. (Ref number: DT 04/3/002/12)
HOW TO EARN YOUR CPD POINTS
1. Check your name and HPCSA number.
2. Read the article and answer all the questions.
3. Indicate your answers to the questions by coloring the appropriate block(s) in the cut-out section at the end of this questionnaire.
4. You will earn 3 CPD points if you answer more than 75% of the questions correctly. If you score between 60-75% 2 points will be
allocated. A score of less than 60% will not earn you any CPD points.
5. Make a photocopy for your own records in case your form is lost in the mail.
6. Send the cut-out answer form by mail, NOT BY FAX to: SASPEN Secretariat, SAJCN CPD activity No 23, c/o Department of Human
Nutrition, PO Box 19063, Tygerberg, 7505 to reach the office not later than 5 March 2004. Answer sheets received after this date will
not be processed.
PLEASE ANSWER ALL THE QUESTIONS
(There is only ONE correct answer per question.)
1. The community-based growth monitoring (CBGM) system
After completion of the immunising schedule, most mothers visit
reached 70-100% of preschool children for growth monitoring
the health facility:
for weighing of the child
because the child is sick
Mothers associated a downward growth curve with a problem or
Preschool children's clinic attendance increase after the age of
a child being sick.
Most mothers understand the concept of growth monitoring.
The community-based growth monitoring (CBGM) system
increased preschool coverage by more than 60%.
10. What percentage of children received food supplements for 3
consecutive months?
Underweight tends to peak:
11. The community-based growth monitoring (CBGM) system
The recumbent position is used to measure:
replaced existing growth monitoring (GM) practices:
children under 2-years-old
children up to 6-months-old
children over 2-years-old
12. What activity was successfully facilitated through the
Which of the following was used as risk criteria in the
community-based growth monitoring (CBGM) system?
community-based system?
treatment of tuberculosis
weight-for-age < 97th percentile
weight-for-age > 3rd percentile
weight-for-age < 3rd percentile
✁ Cut along the dotted lines and send to: SASPEN Secretariat, SAJCN CPD activity No 23, c/o Department of Human Nutrition,
PO Box 19063, Tygerberg, 7505 to reach the office not later than 5 March 2004
HPCSA number: DT
Surname as registered with HPCSA: Initials:
Postal address: _
Full member of ADSA: yes no If yes, which branch do you belong to?
134 Full member of SASPEN: yes no Full member of NSSA: yes no
"A community-based growth monitoring model to complement facility-based nutrition and health practices in a semi-urban
community in South Africa"
SE Schoeman, MA Dhansay, JE Fincham, E Kunneke, AJS Benadé
Please color the appropriate block for each question
(e.g. if the answer to question 1 is a: 1) a b)
Source: http://sajcn.co.za/index.php/SAJCN/article/viewFile/43/39
Antiviral Research 71 (2006) 154–163 Antiviral drugs for cytomegalovirus diseases Department of Clinical Virology, Division of Virology, GlaxoSmithKline Inc., RTP, NC, United States Received 15 March 2006; accepted 4 May 2006 Dedicated to Prof. Erik De Clercq on the occasion of reaching the status of Emeritus-Professor at the Katholieke Universiteit Leuven in September 2006
Design of the HIV Prevention Trials Network (HPTN) Protocol 054: A cluster randomized crossover trial to evaluate combined access to Nevirapine in developing countriesJim HughesUniversity of Washington, [email protected] Robert L. GoldenbergUniversity of Alabama, [email protected] Catherine M. WilfertElizabeth Glaser Pediatric AIDS Foundation/Duke University, [email protected]