Microsoft word - cover
of lo
The Sri Lanka Journal of Haematology
Volume 7, Issue 1, July 2015 ISSN 1391 - 7919
Dr. Hemali W. W. Goonasekera
MBBS, Dip.Path, MD(Haematology)
Dr. Indira Wijesiriwardena
MBBS, Dip.Path, MD(Haematology)
Dr. Arundathi P. Kurukulasuriya
MBBS, Dip.Path. MD(Haematology), FRCPA,
ASTHE, Dip.Buddhist Phil., SFSEDA, FSLCH
Dr. Nishadya N. Ranasinghe
MBBS, Dip.Path, MD(Haematology), FRCPA
The Sri Lanka College of Haematologists
No. 6, Wijerama House
Phone: 0112685088
Printed by
Ananda Press
82/5, Sir Ratnajothi Saravanamuttu Mawatha
Colombo 13
E-mail: [email protected]
The Sri Lanka Journal of Haematology
Volume 7, Issue 1, July 2015
History of bone marrow transplantation
Setting up a blood and marrow transplant (BMT)
program in South Asia: Rewards and challenges
Treatment of elderly acute myeloblastic leukaemia with
azacitidine after failure of decitabine
MB Agarwal
Hospital admission rate, pattern of lower limb deep vein
thrombosis (DVT) and its relationship to acquired risk factors
among patients admitted to Colombo South Teaching Hospital
(CSTH) during the year 2010
HE Alwis, N Ranasinghe
CME article
Theme: Acute trauma coagulopathy and massive
transfusion
HWCK Kulathilake, I Wijesiriwardena
Case report I
Paroxysmal cold haemoglobinuria in a pregnant woman
leading to severe anaemia and fetal loss
EL Asfir, N Senadheera, S Jayasinghe, H Liyanage
Case report II
Lupus anticoagulant – hypoprothrombinaemia syndrome
ONKD Gamage, MM Jayatilaka, PM Punchihewa
Images in
A case of Large Granular Lymphocytosis
MN Dilhani, S Suresh, J Thennakoon
HWW Goonasekera.
SLJH. 2015; 7
(1): 1-4 JH. 2015; 7(1): 1-4
Bone marrow transplantation in Asia – a historical perspective
The healing power of bone marrow (BM) had even
experiment which showed presence of donor cells
been recognized in Greek mythology; which
in a recipient mice tagged with a chromosome
mention the use of bone marrow extracts from
marker.9 The main turning point in determining the
animals to treat injured warriors. In modern
success of BMT was the discovery of the human
medical literature the earliest reports of BM for
leucocyte antigens (HLA) initially described by the
therapy records oral administration to a patient
French scientist Jean Dausset in 195810 and later
with leukaemia in 18961 and intravenous infusion
(IVI) of small volumes of allogeneic BM in 1939 toa 19-year-old girl with aplastic anaemia (AA) from
E. Donnall Thomas based on his own experimental
her sibling.2 The first successful human bone
findings of allogeneic BMT using outbred dogs and
marrow transplant (BMT) was in 1956 by E. Donnall
knowledge of the HLA system; carried out the first
Thomas and his team in New York who adminis-
allogeneic transplant for leukaemia11 and alloge-
tered BM by IVI following total body irradiation (TBI)
neic transplantation for aplastic anaemia by early
to two patients with leukaemia from syngeneic
1970s.12 The first successful matched unrelated
twins;3 their leukaemia initially went into remission,
donor (MUD) transplant was reported by Thomas
but recurred by 7 and 12 weeks in both. Although
et al. in 1980.13 E. Donnall Thomas; who is regarded
the patients did not survive, it demonstrated that
as the father of BMT; for his discoveries in cell
it was possible to induce leukaemia remission by
transplantation for treatment of human disease and
isologous BMT following TBI and irradiation doses
Joseph E. Murray (who performed the first successful
which can induce remission but not produce side
kidney transplant in 1954) were awarded the Nobel
effects such as radiation sickness were described;
Prize in Physiology or Medicine in 1990.14 For their
which was important in the context of the concerns
work on the discovery of the HLA system the Nobel
regarding use of irradiation to treat human disease
Prize in Physiology or Medicine was awarded to
present at that time.
Jean Dausset with Baruj Benacerraf and George D.
Snell in 1980.
The basic foundations for modern day BMT werebased on the seminal experiments carried out by
Transplantation extended to conditions other than
Jacobson et al. in the middle of the last century
leukaemia and the first transplant for immune-
demonstrated that lethally irradiated mice were
deficiency was performed in 1967 on a 5-month-
able to survive if the spleen, or even parts of liver,
old male child diagnosed with severe combined
head and limbs were shielded by lead.4,5 Other
immunodeficiency, from his eight-year-old sister;
animal model experiments followed which also
both peripheral blood and bone marrow were
showed that irradiation followed by marrow
infused intraperitoneally and the patient had
infusion resulted in survival, especially if the
survived.8,15 The first successful use of cryopre-
marrow was derived from mice of similar strain6
served autologous marrow to treat lymphomas
or autologous marrow was used7 and these and
were reported in 197816 and BMT using syngeneic
other experiments proved the hypothesis that a
twins for chronic myelogenous leukaemia (CML)
cellular factor instead of a humoral factor was
with successful eradication of the Philadelphia
responsible for this protective effect8; including the
positive clone was reported in 1979.17 SuccessfulHLA-matched allogeneic BMT for Thalassaemia18and Sickle cell anaemia19 were reported in July 1982and June 1988 respectively.
1Senior Lecturer/Consultant Haematologist,
By early 1990s, BMT became established therapy
Department of Anatomy, Faculty of Medicine,
for malignant and non-malignant haematological
University of Colombo, Sri Lanka.
conditions, immunodeficiency disorders and solid
The Sri Lanka Journal of Haematology
HWW Goonasekera. SLJH. 2015; 7(1): 1-4
tumors.20 In April 1977, Dr. Thomas et al. reported
haematopoietic reconstitution following transfusion
BMT and post BMT sequelae of 100 patients with
of autologous blood cells collected from CML patients
acute leukaemia describing the complications of
prior to chemotherapy and TBI32 and by late 1980s,
BMT and recommended early BMT in acute leu-
the advantages of peripheral blood derived haemato-
kaemia for those who have a HLA matched sibling
poietic stem cells (PB-HSC) over BM derived stem
cells were recognized and autologous transplantsusing PB-HSC started being reported.33,34 In 1981
From the outset, the main factors for successful
Gluckman et al. published the first report of um-
outcomes following BMT were graft-versus-host
bilical cord blood transplantation (CBT) in a boy
disease (GVHD), graft rejection, relapse, infections
with Fanconi's anaemia from his sibling sisters'
and HLA matched donors.8,11,15,21 Cyclosporin A to
cryopreserved cord blood.35 Since then by 2009 over
prevent GVHD was first described by Powles et al.
20,000 CBTs have been done, with establishment
in 198022 and prevention of GVHD using a
of cord blood banks.36
combination of cyclosporine with methotrexatewas reported in 1986.23 Additionally in 1980s T-cell
Bone marrow transplantation (BMT) has finally
depleted donor marrow to prevent GVHD wasdescribed.24 Use of donor lymphocyte infusion
taken firm roots in Sri Lanka with starting off of
(DLI) were initially described in relapsed patients
BMT programmes in two leading private hospitals
with CML in 199025 and further modifications to
and plans are underway to set up BMT units in the
improve the efficacy of DLI is being explored.26
main paediatric hospital, Lady Ridgway Hospital for
Use of recombinant granulocyte-macrophage
Children and the leading cancer care centre, Cancer
colony-stimulating factors to reduce morbidity and
Institute, Maharagama; which are two leading
mortality following transplantation was initially
Government Hospitals, in the near feature. In this
described in late 1980s and its effectiveness in
context, Dr. Rajkumar's leading article which
lymphoid malignancies were proved by Nemunaitis
appears in this issue of the Sri Lanka Journal of
et al. in 1991.27 As allogeneic BMT transplants
Haematology is timely since he eloquently describes
became more widely used donor registries were
the background and factors pertaining to BMT in the
established to find a suitable donor; the Anthony
leading article titled "Setting up a blood and
Nolan trust in London became the first registry of
marrow transplant (BMT) program in south Asia:
unrelated bone marrow donors, established by the
Rewards and challenges". Dr. Kumar's article also
mother whose son had Wiskott-Aldrich syndrome.28
includes details pertaining to BMT programmes in
By the year 2013, over 25,000 allogenic BMTs were
our region which will be useful for the Haemato-
being performed worldwide and marrow donor
logists who are currently in the process of setting
programs and marrow transplant registries having
up of BMT programmes in the above mentioned
been established with over 20 million registered
hospitals as well as the Haematology trainees who
volunteer unrelated donors.29
will have to take up the challenge of carrying theseinitiatives forward once they qualify and become
In the latter part of the last century advances made
Consultant Haematologists in local BMT units.
in genetic technology rapidly became incorporatedinto the field of BMT enabling better transplant
Furthermore, Dr. Agarwal's perspective on treat-
outcomes. Shifting of HLA typing from serological
ment for leukaemia will be read with enthusiasm
to molecular methods ensured less donor mismatch
especially by the Haematologists who are actively
and a better chance of marrow engraftment.30 In
involved in treating haemafo-oncology patients.
1988 minimal residual disease (MRD) monitoringusing polymerase chain reaction technology inplace of conventional cytogenetics was reported
and with further advances in technology it was
1. Quine WE. The remedial application of bone marrow.
possible to quantitate MRD in CML using real-time
JAMA 1896; 26: 1012-13.
quantitative PCR by late 1990s and it soon became
2. Osgood EE, Riddle MC, Mathews TJ. Aplastic anemia
used in other haematological malignancies.31
treated with daily transfusions and intravenous
marrow; case report. Ann Intern Med. 1939; 13(2):
In 1981 Goldman et al. described successful
357-67. doi: 10.7326/0003-4819-13-2-357.
The Sri Lanka Journal of Haematology
HWW Goonasekera. SLJH. 2015; 7(1): 1-4
3. Thomas ED, Lochte HL Jr. , Cannon JH, Sahler OD,
17. Fefer A, Cheever MA, Thomas ED, Boyd C, Ramberg R,
Ferrebee JW. Supralethal whole body irradiation and
Glucksberg H, Buckner CD, Storb R. Disappearance
isologous marrow transplantation in man. J. Clin.
of Ph1-positive cells in four patients with chronic
Invest. 1959 Oct; 38: 1709-16.
granulocytic leukemia after chemotherapy, irra-
4. Jacobson LO, Simmons EL, Marks EK, Eldredge JH.
diation and marrow transplantation from an
Recovery from irradiation injury. Science. 1951; 12:
identical twin. N Engl J Med. 1979 Feb 15; 300(7):
5. Jacobson LO, Marks EK, Robson MJ, Gaston EO, Zirkle
18. Thomas ED, Buckner CD, Sanders JE, Papayannopoulou
RE. Effect of spleen protection on mortality following
T, Borgna-Pignatti C, De Stefano P, Sullivan KM, Clift
x-irradiation. J Lab Clin Med. 1949; 34: 1538-43.
RA, Storb R. Marrow transplantation for thalassaemia.
Lancet. 1982 July 31; 320(8292): 227-29.
6. Lorenz E, Uphoff D, Reid TR, Shelton E. Modification
of irradiation injury in mice and guinea pigs by bone
19. Vermylen C, Fernandez Robles E, Ninane J, Cornu G.
marrow injections. J. Natl. Cancer Inst. 1951; 12:
Bone marrow transplantation in five children with
sickle cell anaemia. Lancet. 1988 Jun 25; 1(8600):
1427-8.
7. Mannick JA, Lochte HL Jr, Ashley CA, Thomas ED,
Ferrebee JW. Autografts of bone marrow in dogs
20. Armitage JO. Bone marrow transplantation. N Engl J
after lethal total-body radiation. Blood. 1960 Feb;
Med. 1994 Mar 24; 330(12): 827-38.
15: 255-66.
21. Thomas ED, Buckner CD, Banaji M, Clift RA, Fefer A,
8. de la Morena MT, Gatti RA. A history of bone marrow
Flournoy N, Goodell BW, Hickman RO, Lerner KG,
transplantation. Hematol Oncol Clin North Am. 2011
Neiman PE, Sale GE, Sanders JE, Singer J, Stevens M,
Feb; 25(1): 1-15. doi: 10.1016/j.hoc.2010.11.001.
Storb R, Weiden PL. One hundred patients with acuteleukemia treated by chemotherapy, total body
9. Ford CE, Hamerton JL, Barnes DW, Loutit JF. Cytological
irradiation, and allogeneic marrow transplantation.
identification of radiation-chimaeras. Nature. 1956
Blood. 1977; 49: 511-33.
Mar 10; 177(4506): 452-4.
22. Powles RL, Clink HM, Spence D et al. Cyclosporin A to
10. Dausset J. [Presence of A & B antigens in leukocytes
prevent graft-versus-host-disease in man after
disclosed by agglutination tests]. C R Seances Soc
allogeneic bone-marrow transplantation. Lancet.
Biol Fil. 1954 Oct; 148(19-20): 1607-8. [Article in
1980; 1: 327-9.
23. Storb R, Deeg HJ, Whitehead J, Appelbaum F, Beatty P,
11. Appelbaum FR. Hematopoietic-Cell Transplantation
Bensinger W, Buckner CD, Clift R, Doney K, Farewell
at 50. N Engl J Med. 2007 Oct 11; 357(15): 1472-5.
V, et al. Methotrexate and cyclosporine compared
12. Thomas ED, Storb R, Fefer A, Slichter SJ, Bryant JI,
with cyclosporine alone for prophylaxis of acute graft
Buckner CD, Neiman PE, Clift RA, Funk DD, Lerner KE.
versus host disease after marrow transplantation
Aplastic anaemia treated by marrow transplantation.
for leukemia. N Engl J Med. 1986 Mar 20; 314(12):
Lancet. 1972 Feb 5; 1(7745): 284-9.
13. Hansen JA, Clift RA, Thomas ED, Buckner CD, Storb R,
24. Prentice HG, Blacklock HA, Janossy G, Gilmore MJ,
Giblett ER. Transplantation of marrow from an
Price-Jones L, Tidman N, Trejdosiewicz LK, Skeggs DB,
unrelated donor to a patient with acute leukemia. N
Panjwani D, Ball S, et al. Depletion of T lymphocytes
Engl J Med. 1980 Sep 4; 303(10): 565-7.
in donor marrow prevents significant graft-versus-
14. Thomas ED. The Nobel Lectures in Immunology. The
host disease in matched allogeneic leukaemic
Nobel Prize for Physiology or Medicine, 1990. Bone
marrow transplant recipients. Lancet. 1984 Mar 3;
marrow transplantation – past, present and future.
Scand J Immunol. 1994 Apr; 39(4): 339-45.
25. Kolb HJ, Mittermüller J, Clemm C, Holler E, Ledderose
15. Gatti RA, Meuwissen HJ, Allen HD, Hong R, Good RA.
G, Brehm G, Heim M, Wilmanns W. Donor leukocyte
Immunological reconstitution of sex-linked lympho-
transfusions for treatment of recurrent chronic
penic immunological deficiency. Lancet. 1968 Dec
myelogenous leukemia in marrow transplant
28; 2(7583): 1366-9.
patients. Blood. 1990 Dec 15; 76(12): 2462-5.
16. Appelbaum FR, Herzig GP, Ziegler JL, Graw RG, Levine
26. Maury S, Redjoul R, Cabanne L, Vigouroux S, Legros L,
AS, Deisseroth AB. Successful engraftment of
Cohen JL. Regulatory T-cell depletion in donor
cryopreserved autologous bone marrow in patients
lymphocyte infusions for haematological malignancies:
with malignant lymphoma. Blood. 1978 Jul; 52(1):
long-term outcomes from a prospective study. Br J
Haemat. 2014; 166: 452-5.
The Sri Lanka Journal of Haematology
HWW Goonasekera. SLJH. 2015; 7(1): 1-4
27. Recombinant Nemunaitis J, Rabinowe SN, Singer JW,
decades of transplantation for chronic myeloid
Bierman PJ, Vose JM, Freedman AS, et al. Recombinant
leukemia: what have we learned? Blood. 2011 Jan
Granulocyte-Macrophage Colony-Stimulating Factor
20; 117(3): 755-63. doi: 10.1182/blood-2010-08-
after Autologous Bone Marrow Transplantation for
301341. Epub 2010 Oct 21.
Lymphoid Cancer. N Engl J Med. 1991 Jun 20; 324:
32. Goldman JM, Catovsky D, Goolden AWG, Johnson
1773-8. DOI: 10.1056/NEJM199106203242504.
Galton DAG. Buffy coat Autografts for patients with
28. Cleaver S. The Anthony Nolan Research Centre and
chronic granulocytic leukaemia in transformation.
other matching registries. In: Treleaven J, Barret J
Blut. 1981; 42: 149-55.
(eds). Bone Marrow Transplantation in Practice.
Churchill Livingstone: Edinburgh, 1992. / Anasetti C.
33. Korbling M , Dorken B, Ho AD, Pezzutto A, Hunstein
Unrelated donor hematopoietic stem cell trans-
W, Fliedner TM. Autologous transplantation of blood-
plantation. In: Atkinson K, Champlin RE, Ritz J, Fibbe
derived hemopoietic stem cells after myeloablative
WE, Ljungman P, Brenner MK, eds. Clinical bone
therapy in a patient with Burkitt's lymphoma. Blood.
marrow and blood stem cell transplantation.
1986; 67: 529-32.
Cambridge, UK: Cambridge University Press; 2004:
34. Bensinger WI, Martin PJ, Storer B, et al. Trans-
plantation of bone marrow as compared with
29. Shaw BE, Chapman J, Fechter M, Foeken L, Greinix H,
peripheral-blood cells from HLA-identical relatives
Hwang W, Phillips-Johnson L, Korhonen M, Lindberg
in patients with hematologic cancers. N Engl J Med.
B, Navarro WH, Szer J. Towards a global system of
2001; 344: 175-81.
vigilance and surveillance in unrelated donors of
35. Gluckman E, Broxmeyer HE, Auerbach AD, et al.
haematopoietic progenitor cells for transplantation.
Hematopoietic reconstitution in a patient with
Bone Marrow Transplant. 2013 Nov; 48(12): 1506-9.
Fanconi's anemia by means of umbilical-cord blood
doi: 10.1038/bmt.2013.104. Epub 2013 Jul 29.
from an HLA-identical sibling. N Engl J Med. 1989;
30. Petersdorf EW, Hansen JA, Martin PJ, Woolfrey A,
321: 1174-8.
Malkki M, Gooley T. Major-histocompatibility-complex
36. Gluckman E. History of cord blood transplantation.
class I alleles and antigens in hematopoietic-cell
Bone Marrow Transplantation 2009; 44: 621-6.
transplantation. N Engl J Med. 2001; 345: 1794-1800.
doi:10.1038/bmt.2009.280; published online 5
31. Pavlu J, Szydlo RM, Goldman JM, Apperley JF. Three
October 2009.
The Sri Lanka Journal of Haematology
Rajat Kumar
SLJH. 2015; . S
7 LJH. 2015;
7(1): 5-14
Setting up a blood and marrow transplant (BMT) program in South Asia:
Rewards and Challenges
Rajat Kumar1
Key words: blood and bone marrow transplant, haematopoietic stem cell transplant, aplastic anaemia,
haploidentical transplants
transfused donor cells also "rescue" the bone
Blood and marrow transplantation (BMT) or
marrow from the effects of chemotherapy. (b)Non-malignant diseases – like aplastic anaemia,
haematopoietic stem cell transplantation (HSCT)
thalassaemia, Gaucher disease, etc. In these
is a life-saving procedure for a number of malignant
conditions the abnormal marrow is replaced by the
and non-malignant life threatening diseases.1,2
healthy donor stem cells.
More than a million procedures have been com-pleted worldwide, and the annual transplant rateis close to 70,000 per annum with approximately
45% being allogeneic.3 The procedure itself has
Stem cell source
many technical variations according to the primarydisease, age of the patient, facilities available and
The three sources of stem cells used in HSCT are
experience of the center. BMT may be autologous
the bone marrow, peripheral blood and cord blood.
or allogeneic. When the patient's own cryopreserved
The three sources differ in the stem cell content,composition and state of activation of immune
haematopoietic stem cells are used to rescue bone
cells. Quantitatively, peripheral blood represents
marrow after high dose chemotherapy, the procedure
the richest stem cell source and cord blood the
is termed as autologous transplantation. Allogeneic
poorest stem cell source. Peripheral blood contains
BMT involves the transplantation of haematopoietic
more lymphocytes than the other two sources. The
stem cells derived from another individual, ideally
most rapid engraftment is observed with peripheral
a human leucocyte antigen (HLA) identical sibling,
blood transplants and the slowest with cord blood
into the patient. In this article, allogeneic HSCT will
transplants. The risk of developing graft-versus-
be discussed. As aplastic anaemia and thalassaemia
host disease (GVHD) also varies with the source of
major are common in South Asia, only these indi-
stem cells. Peripheral blood stem cells (PBSC),
cations will be highlighted.
which contain more T lymphocytes than marrowdoes, increase the incidence and severity of chronic
Indications for HSCT
GVHD compared with bone marrow, while cordblood transplants have a lower risk of GVHD.4,5 The
The indications for allogeneic (allo) haemato-
trends in stem cell source for transplantation are
poietic stem cell transplantation in haematological
changing. A report from the European Group for
disorders can be conveniently divided into two
Blood and Marrow transplantation (EBMT) showed
groups (Table 1): (a) Malignant disorders – like
that in 2011 a total of 35,660 HSCT were reported
leukaemias, myelodysplastic syndromes and
with 41% allogeneic and 59% autologous by 651
lymphomas. In all these indications, the cure is by
centers in 45 countries.6 Peripheral blood stem
a combined effect of the high doses of chemo-
cells were used as a stem cell source in 99% of
therapy or radiation therapy, and a graft versus
autologous and 73% allogeneic HSCT. Bone marrow
tumor effect by the transfused donor cells. The
was used as a stem cell source in allogeneic trans-plantation, primarily for nonmalignant disorders.
Cord blood was used for 6% of allogeneic HSCT,mainly from unrelated donors and no autologous
1 Professor, University of Manitoba, Canada.
cord blood was used.6
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
Table 1. Indications for allogeneic stem cell transplantation
Non malignant disorders
Acute myeloid leukaemia
Thalassaemia major
Acute lymphoblastic leukaemia
Chronic lymphocytic leukaemia
Fanconi's anaemia
Chronic myeloid leukaemia
Sickle cell anaemia
Non-Hodgkin lymphoma
Paroxysmal nocturnal haemoglobinuria
Severe combined immunodeficiency
Multiple myeloma (mainly autologous)
Inborn errors of metabolism
Donor requirement for allogeneic HSCT
Haploidentical related donors
Mendelian genetics dictate that each biologicalparent and each biological child of a patient is HLA-
For an allogeneic BMT, an HLA identical sibling is the
haploidentical, each sibling, half-sibling, aunt or
ideal donor. A sibling who is identical in the HLA-
uncle has a 50% likelihood of being HLA-haplo-
A, B, DR loci is considered HLA identical implying a
identical.3 Thus a haploidentical (haplo) donor can
6/6 match. In spite of HLA identity, there are always
be found for nearly every patient requiring an allo-
variations in the minor histocompatibility loci.
HSCT. Moreover, this is likely to be faster than a
These antigenic differences lead to graft rejection
search for an unrelated donor.
or graft versus host disease unless immunosup-pression is used. It is also possible to have a successfultransplant using a partially matched sibling as a
Choice of donor
donor, or an unrelated HLA identical donor, but the
The best outcomes for allo-HSCT are with a donor
complications of GVHD and graft rejection increase.
who is a HLA-matched sibling. There is 25% chanceof each sibling being HLA-identical, and with the
small family sizes, only 30% chance that a patientwill find a matched sibling donor.
For unrelated transplants, the HLA-C and HLA-DQloci are also tested and a 10/10 match is ideal. For
The next alternative is a matched unrelated donor
unrelated umbilical cord blood transplants, a 6/6
(MUD)7. The unrelated donor pool has expanded
or even a 4/6 match is acceptable as the cord blood
to more than 26 million donors worldwide, with
cells are immunologically naïve and the risk of
an increased number of unrelated allo-HSCTs
GVHD is less. With improvements in HLA typing at
being performed. With improvement in protocols,
the molecular level, results of unrelated transplants
outcomes with matched unrelated donor trans-
are often equivalent to matched sibling transplants
plants rival those after matched sibling tran-
and at times may be preferred. The massive increase
splants3. Suitable matched unrelated donors (MUD)
of unrelated donor registries has increased the
are found for 60% to 80% of white Caucasians but
likelihood of finding a well-matched unrelated
only for 10% of ethnic minorities.
donor in addition, there is increasing evidence thatthe well-matched donor in certain situations might
For those who do not have HLA-matched related
be preferable to a sibling donor, for example, in
or unrelated donors, the options are (a) mis-
the situation of an older male patient with the
matched unrelated donor (MMURD) (b) unrelated
choice between an older female sibling donor and
donor umbilical cord blood or (c) HLA haplo-
a young well-matched unrelated male donor.
identical, related donors.3,7
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
Engraftment is considered established when theperipheral neutrophil count reaches 0.5 x 109/L on
Myeloablative conditioning. The standard
3 successive days.
preparatory regimens given prior to HSCT aremyeloablative. Patients receive extremely high
Peripheral blood stem cell transplantation (PBSCT)
doses of chemotherapy or radiotherapy or both.
The aim is threefold: (a) Eradication of malignant
It is well known that the peripheral blood contains
cells or, in cases of genetic disorders, it is eradication
a small percent of circulating stem cells, approxi-
of the abnormal clone of cells, (b) Suppression of
mately 0.1%. This number can be increased by
the immune system of the host (recipient) so that
administration of colony stimulating factors, like
the allograft is not rejected, and (c) Clearing a
Granulocyte-colony stimulating factor(G-CSF),
"physical space" to allow adequate growth of the
which mobilize stem cells from the bone marrow.
donor stem cells. The conditioning, which is myelo-
For allogeneic donors, administration of G-CSF for
ablative, is also toxic to various organs like the liver,
4 to 5 days results in high circulating stem cells
lungs, kidneys, gastrointestinal tract and repro-
which can be collected by a cell separator. The
ductive system.
procedure requires venous access and takes aboutthree to four hours. The donor need not be admitted,
Non-myeloablative or reduced-intensity con-
does not require anesthesia and is spared the pain
ditioning. The association of GVHD with diminished
of marrow aspiration. Haematopoietic reconstitution
relapse rates following allogeneic HSCT, together
is more rapid and predictable when PBSCs are
with the dramatic responses sometimes seen
used for transplantation. This translates in reduced
following donor lymphocyte infusions demonstrates
duration of neutropenia, fewer platelet transfusions,
the potential of the human immune system to
and shorter hospital stay (Table 2). Immune recon-
eradicate haematological malignancies. The
stitution may be better with PBSCT as there are
curative potential of allogeneic BMT is mediated
more lymphocytes in the graft as compared to
in part by an immune mediated graft-versus-tumor
effect. This has prompted some workers to focuson the use of donor T cells to eradicate both non-
Cord blood stem cell transplantation
malignant and malignant cells of host origin,
Placental blood, which is routinely discarded in
without the use of myeloablative conditioning
clinical practice, is potentially a vast supply of
regimens. This reduced-intensity conditioning (RIC)
allogeneic foetal haematopoietic stem cells. Cord
aims to suppress the immunity of the recipient
blood (CB) stem cells have distinctive proliferative
sufficiently to allow allogeneic engraftment,
advantages which include an (a) enriched pro-
without destroying the recipient's marrow, with
portion of immature stem cells, (b) higher clono-
lower regimen related toxicity. This represents an
genic growth advantage, (c) increased cell cycle
important step in capitalizing on the allogeneic
rate, (d) autocrine growth factors production and
(e) increased telomere length.
Technical aspects of allogeneic transplantation
The main limitation of cord blood transplants (CBT)is the limited number of nucleated cells available
Bone marrow transplantation
in a unit. As compared to bone marrow trans-
The actual bone marrow transplant is not com-
plantation, the time for engraftment in cord blood
plicated. The donor's marrow is harvested by
transplantation is much longer, taking a month for
repeated aspiration from the posterior iliac crests,
neutrophilic engraftment and more than fifty days
under general or spinal anaesthesia. The marrow
for platelet engraftment. There is also a higher
is collected in a bag with anticoagulant. The number
incidence of non-engraftment. The nucleated cell
of marrow cells or total nucleated cells (TNC)
dose available in a cord blood unit is critical, being
required for successful engraftment is estimated
1 log less than in a bone marrow transplant. The
to be at least 1 to 3 x 108 per kg of recipient's body
minimum recommended dose for CBT is 2.0 to 2.5
weight. Bone marrow is transfused through the
x 107 nucleated cells /kg for a successful outcome
veins and the donor marrow cells home into the
and at least a 4/6 HLA match. The main advantage
recipient's marrow space and start engrafting.
of CBT is a lower incidence and severity of GVHD.
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
Table 2. The advantages and disadvantages of PBSCT
1. Faster neutrophil recovery
2. Faster platelet recovery
3. Faster immunologic recovery
Higher incidence of chronic GVHD
4. Less IV antibiotics
5. Shorter hospitalization
7. More graft versus tumor effect (?)
1. No general anesthesia
1. Venepuncture or central line
2. No marrow harvest
2. Side effects from growth stimulating
factors, or citrate used for PBSC harvest
3. No hospitalization
PBSCT – Peripheral blood stem cell transplantation, IV – Intravenous, GVHD – Graft-versus-host-disease,PBSC – Peripheral blood stem cell
This allows a 1 to 2 HLA antigen mismatch even in
developed in Italy. The average dose of cells is
unrelated CBT. More than 600,000 cord blood units
>10 x 106 CD34+ cells/kg body weight of recipient.10
have been stored worldwide and over 30,000 CBT have
(2) The GIAC protocol used in China, comprising of
been performed, mainly in the unrelated setting.9
G-CSF stimulation of donor; Intensified immuno-suppression using post-transplant cyclosporine, myco-
The main problem in doing CBT in adults is the
phenolatemofetil and short course methotrexate;
limited number of nucleated cells/CD34+ cells in a
ATG added to conditioning to aid engraftment and
cord blood collection relative to the weight of an
help prevent GVHD; and combination of PBSC and
adult. Different strategies are being investigated
BM allografts11. (3) High dose, post transplantation
for this; these include (a) multiunit cord blood trans-
plantation, (b) ex-vivo expansion of CB haemato-poietic stem cells (c) nonmyeloablative preparative
Post-transplantation cyclophosphamide was first
regimen to reduce the conditioning toxicity5,9.
developed in animal models and finally translatedinto clinical practice by groups at Johns Hopkinsand Fred Hutchinson Cancer Research Center.13
It was shown that cyclophosphamide is nontoxic
In the past, results of haplo-HSCT were poor due
to haematopoietic stem cells because of high
to high incidence of graft failure or GVHD, due to
expression of the detoxifying enzyme aldehyde
bi-directional allo-reactivity. This is due to the high
dehydrogenase. Moreover, cyclophosphamide is
frequency of T lymphocytes that recognize major
selectively toxic to dividing cells.
class I or II HLA disparities between the donor andrecipient.
With post-transplant cyclophosphamide, the firststep is selective killing of proliferating alloantigen-
In the last two decades, the outcomes of haplo-
stimulated T cells. As replicating T cells are uniquely
HSCT have improved and results are comparable
sensitive to cyclophosphamide, both anti-host and
to unrelated HSCT for malignant disease indications.
anti-donor T cells are selectively destroyed. The
There are three main approaches to control graft
quiescent progenitor cells and memory T cells in
failure or GVHD. (1) The megadose HSCT approach
the graft are not affected. Persistence of donor
using PBSCs positively selected for CD34+ cells,
non-alloreactive T cells can provide the transplant
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
recipient with donor-derived immunity to fight
dysplastic syndrome-2 and thalassaemia major-4.
infections. The second step is the development of
The median age was 19 years (range 2.2-46) with
peripheral tolerance. The third step is deletion of
29 male and 11 female participants. The 30-day
donor stem cell derived anti-host T cells in the
mortality was nil, and 100-day mortality was 1
thymus.12 Cylophosphamide is usually given on
(2.5%). This experience suggests that allogeneic
days 3 and 4 post stem cell infusion at doses of
HSCT can be safely performed in non-HEPA filter
50mg/kg on each day.14
rooms in India.16 Updated results confirm that thisapproach is effective in high risk patients.17
This protocol is used widely in the United Statesand many other countries, including India. Number
Venous access. The transplant process typically
of studies have used this protocol in myeloablative
involves the use of a long term, silastic, multi-
as well as reduced intensity conditioning, with BM
lumen, flexible catheter for chemotherapy adminis-
or PBSC as stem cell sources.13,14 This approach has
tration, infusion of stem cells and supportive care
shown acceptable incidence of GVHD and low non
management including frequent blood sampling,
relapse mortality. When myeloablative conditioning
intravenous antibiotics, blood components and
was used, the relapse rate was lower than with
parenteral nutrition.18
RIC and results comparable to those with MUD orcord blood transplant. It is the most attractive
Infections. Infection remains an important cause
protocol for haplo-HSCT in developing countries,
of morbidity and mortality after BMT, with
as no special equipment is needed for stem cell
bacterial, fungal infections and viral infections
manipulation, there is no need for expensive
being the predominant cause.19 The EBMT analyzed
medications, the cost of cyclophosphamide is low and
a large homogeneous group of 14,403 patients
it is given by simple intravenous administration.
transplanted for early leukaemia from an HLA-identical sibling and reported to the EBMT from
1980 to 2001. Of the 597 deaths with infection as
Protective isolation. After transplantation of the
the primary cause of death, 217 (36%), were attri-
marrow, it takes about two to three weeks before
buted to bacteria, 183 (31%) to viruses, 166 (28%)
engraftment occurs, that is the time when the stem
to fungi and 31 (5%) to parasites. The cumulative
cells start producing adequate number of neutro-
incidence of deaths with infection at 5 years was
phils, platelets and erythrocytes. During this
5% with a cumulative incidence of 1.8% attributed
period very intensive support is required. Ideally
to bacteria, 1.6% to viruses, 1.4% to fungi and 0.3%
a high-efficiency particulate arrestance (HEPA)
to parasites19. During the early neutropenic period,
filtered unit should be available for hospitalization
bacterial and fungal infections predominate while
for transplantation. It is emphasized that the risk
viral infections are frequent after engraftment
of infections lasts for almost a year in allogeneic
when the cell mediated immunity is impaired, the
HSCT. Some centers have reported carrying out
most important viruses being cytomegalo virus,
stem cell transplants without protective isolation,
herpes simplex virus, and varicella zoster. Bacterial
or even in outpatient setting, without increase in
infections with encapsulated organisms again
morbidity or mortality.15 This is only feasible if the
predominate after three to six months of engraft-
home offers a clean environment, the patient can
ment, akin to the condition in post splenectomised
be monitored closely and admitted immediately,
patients antimicrobials should be administered
if required. At the All India Institute of Medical
after establishing the cause of infection, but in
Sciences (AIIMS), the department of haematology
practice an aetiological agent is often not identified.
recently published its experience of performing
During the neutropenic phase, early institution of
40 consecutive allogeneic transplants from July
empirical antibiotics to cover gram-negative and
2004 to November 2007 in single non-HEPA filter
gram-positive bacteria, with addition of antifungal
rooms for a variety of indications. Source of stem
drugs like amphotericin or voriconazole if fever
cells was peripheral blood in 33, bone marrow in
persists, is practiced in most centers in India16.
six and combined in one. The indications weresevere aplastic anemia-18, chronic myeloid
Blood component support. After conditioning
leukaemia (CML)-7, acute myeloid leukaemia
therapy, patients require multiple red cell and
(AML)-7, acute lymphoblastic leukaemia-2, myelo-
platelet transfusions during the 2-4 week period
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
of pancytopenia, till engraftment occurs. Patients
are profoundly immunosuppressed and at risk of
In allogeneic HSCT patients, a unique complication
developing transfusion associated-graft versus
occurs: GVHD. There are two types of GVHD, acute
host disease (TA-GVHD) after receiving cellular
and chronic.2 Acute GVHD: This occurs within the
blood products. To prevent this, all cellular blood
first 100 days after transplant. It classically affects
products should be irradiated prior to transfusion,to inactivate the donor lymphocytes. Hence a blood
three tissues, namely the skin, gut and liver and
irradiator is essential for any allogeneic BMT center.
may be accompanied by fever. The severity can begraded according to the extent of skin involve-
Haematopoietic growth factors. Haematopoietic
ment, degree of hyperbilirubinemia and severity
colony stimulating factors like G-CSF are often
of diarrhoea.2 Chronic GVHD: This usually develops
administered to patients after infusion of stem
later than 100 days after transplant and often
cells in order to reduce the duration of neutropenia.
follows acute GVHD but may also develop de novo.
More recently, studies have shown that even
It is classified as limited or extensive chronic GVHD.
without use of these factors there is no adverse
Clinically it resembles autoimmune disorders like
impact on outcome, and many centers use them
scleroderma with skin rash, sicca complex, sclero-
only in cases with delayed engraftment.
sing bronchiolitis and hepatic dysfunction. Themortality varies from 20% to 40%. Management is
Toxicity related to conditioning. The conventional
with immunosuppressive agents like cyclosporine,
myeloablative therapy given before infusion of
prednisolone, tacrolimus, mycophenolate, sirolimus,
bone marrow causes organ toxicity, in addition to
methotrexate and cyclophosphamide in various
myelotoxicity. These are: (a) veno-occlusive
combinations. After a year or more, many patients
disease (VOD) of the liver, more accurately termed
develop self-tolerance and these drugs can be
as "sinusoidal obstruction syndrome". It is charac-
tapered off. GVHD is more common in older patients
terized by (i) jaundice (ii) hepatomegaly and right
and those with one or more HLA mismatches or
upper quadrant pain (iii) ascites or (iv) unexplained
unrelated HLA identical transplants. It is mainly for
weight pain, (b) haemorrhagic cystitis characterized
this reason that elderly patients do not do well
by the presence of haematuria, dysuria, and urinaryfrequency in a patient with sterile urine, (c) seizures
with allogeneic BMT due to severe GVHD. With the
usually drug induced, (d) pulmonary complications
use of PBSC, the time limits are not so well defined
which can be infectious or non-infectious, and (d)
and acute GVHD may occur later while classical
skin and mucosal changes like alopecia, nail changes
chronic GVHD may occur earlier.
and oral mucositis.
Failure of engraftment
A successful BMT does not always mean that the
Failure to engraft after HSCT (graft dysfunction) or
primary disease is cured. A certain number of
to sustain engraftment (graft rejection) is a
patients will relapse from the original malignancy,
formidable complication due to many possible
as the tumor cells survive the chemo/radiotherapy
factors. These include inadequate stem cell
and graft versus tumor effect. Relapses are higher
numbers, infections, graft-versus-host disease and
if the HSCT is performed when the disease is not in
immunological mediated processes. The stem cell
remission, or at an advanced stage, or is aggressive.
graft may get rejected by functional host lympho-cytes which survive the conditioning regimen.
Patients with haematological malignancies who
Fortunately, this complication is uncommon. Multiple
relapse after allogeneic bone marrow trans-
treatment alternatives have been explored includinghaematopoietic growth factors, additional infusions
plantation can be treated by infusing lymphocytes
of stem cells alone, with augmented immuno-
from the original stem cell donor. Donor lymphocyte
suppression or with additional cytotoxic therapy.
infusion (DLI) induces complete remissions in the
The incidence is higher in unrelated donor trans-
majority of patients with CML in early-stage relapse
plantation and whenever there is presence of any
and in less than 30% of patients with relapsed
HLA mismatch. Depleting the graft of T cells also
acute leukemia, myelodysplasia, and multiple
increases graft rejection.
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
Requirements for BMT unit
matched siblings. A total of 134 grafts were PBSC
The complexity of the transplantation procedure
grafts, and 558 were bone marrow grafts. Rates
highlights the need for adequate infrastructure,
of haematopoietic recovery and grades 2 to 4
experience and teamwork, to manage patients
chronic GVHD were similar after PBSC and bone
who can potentially have multiple complications.
marrow transplantations regardless of age at
A multispecialty approach is needed. An efficient
transplantation. In patients older than 20 years,
blood bank and transfusion center with facilities
chronic GVHD and overall mortality rates were
for blood component therapy is critical. Blood
similar after PBSC and marrow transplantations. In
irradiation facilities are essential. As infections are
patients younger than 20 years, rates of chronic
common in early and late phases, facilities for
GVHD (relative risk [RR] 2.82; P=.002) and overall
diagnosis and management of common and rare
mortality (RR 2.04; P=.024) were higher after
bacterial, fungal, viral and parasitic infections are
transplantation of PBSCs than after transplantation
needed. For organ toxicity and GVHD management,
of bone marrow. These authors concluded that
subspecialties of gastroenterology, pulmonology,
bone marrow grafts are preferred to PBSC grafts in
hepatology, cardiology, dermatology, ophthal-
young patients undergoing HLA-matched sibling-
mology, histopathology and others are required.
donor transplantation for SAA.21 A similar con-
Documentation of all cases and prospective
clusion was reached by another EBMT study.22
registries are needed. Guidance may be obtainedfrom the Center for International Blood and
This view is not accepted by many experts in the
Marrow Transplant Research (CIBMTR) or the EBMT.
developing world. Patients with aplastic anemia
As a general guide, a center should be capable of
who come for transplantation in developing
successfully treating patients of AML, before embar-
countries are often multi-transfused and the blood
king on a BMT program.
products they receive are usually not leuco-depleted. They are therefore alloimmunised andhave a high risk of graft rejection. PBSC transplant
Indications for allogeneic transplants
reduces the chances of graft rejection due to a
In recent years, evidence based guidelines have
higher stem cell dose and the higher T cell content.
been formulated for indications in haematologic
Moreover, many patients are infected prior to
disorders. These may change with improvements
coming for transplant and a PBSC graft source has
in non-transplant therapy. As an example, allo-
the advantage of an earlier engraftment as well as
HSCT was the first line treatment for patients of
immune reconstitution. The transplant centers at
CML who were eligible and had a donor, but with
AIIMS New Delhi and Christian Medical College
the availability of tyrosine kinase inhibitors, the
(CMC) Vellore routinely use PBSC as a preferred
indications of transplant have reduced radically.
source for allo-HSCT in aplastic anemia.23,24 Thesuccess rates of 70-80% survival suggest that in the
Indian context, PBSC may be a preferred source ofstem cells in the high risk patients seen in India. A
Severe aplastic anemia (SAA) is potentially curable
recent analysis of 2374 HLA identical sibling
with allo-HSCT, the only limiting factor being the
transplants in SAA across different economic zones,
transplant related morbidity and mortality.
confirmed the observation that overall, BM is a
Guidelines suggest that in young patients with an
better source than PBSC. However, there was no
HLA matched sibling donor, allo-HSCT should be
difference in overall survival between the two graft
first line therapy, as the complications are much
sources in upper-middle-income and lower-middle
less (Table 3). In those who are older than 50 years,
and lower-income countries, hence PBSC may be
immunosuppression should be tried first.20 The
an acceptable alternative in countries with limited
source of stem cells is also controversial. A recent
resources when treating patients at high risk of
study showed better outcome with bone marrow
graft failure and infective complications.25 The use
versus peripheral blood. This was mainly due to a
of haploidentical transplants is considered experi-
higher GVHD in the PBSCT group.21 This study
mental, but in future it may become a preferred
analyzed the outcome of 692 patients with severe
source for those without sibling donors, if the
aplasticanemia receiving transplants from HLA-
problem of graft rejection can be overcome.20
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
Table 3. BMT in aplastic anaemia
If HLA identical sibling available.
The indications of age may be relaxed
(a) Age < 50 yr: BMT 1st line treatment.
(b) Age >50yr: BMT as 2nd line treatment
(a) Patients who are infected and would
if immunosuppression fails
not tolerate immunosuppression
in 3-4 months.
or(b) very severe aplastic anaemia
If only HLA identical unrelated donoravailable.
Age < 50 years: BMT ifImmunosuppression fails.
BMT – Blood and marrow transplantation, HLA – Human leucocyte antigen
countries with limited resources, HSCT is pre-ferentially restricted to allogeneic transplants with
A major indication for allo-HSCT in India is thalas-
stem cells from family donors for non-malignant
saemia major. This disease is potentially curable
indications or chronic leukaemias29.
with an allogeneic transplantation. The results areexcellent if the transplantation is done prior to
In India, the cost of an allogeneic HSCT varies as
the complications of iron overload, transfusion
per the indication and the type of hospital (Govern-
complications and alloimmunisation. Results from
ment funded or private). The cost of an allogeneic
Pesaro, Italy, suggest more than 85% disease free
transplant in AIIMS, New Delhi, varies between
survival for patients transplanted early, in Pesaro
US $6000 to 12,000. The cost of medication and
Class 1.26 In India, similar results have been attained
monitoring after engraftment is additional. In private
at CMC, Vellore.27 When a child is diagnosed with
corporate hospitals, the cost varies between US
thalassaemia major, treatment should be started
$15,000 to 30,000 for initial hospitalization. The
with optimal blood transfusion and iron chelation
variation in cost depends on the conditioning regi-
instituted before there is a significant rise in ferritin
men, complications and the use of anti-infectives
levels. All siblings should be typed for an HLA
and supportive drugs. Thus the use of anti-thymo-
identical match. If a match is available, the child
cyte globulin would significantly increase the cost
should be referred to a transplant center. An allo-
HSCT should be performed as soon as feasible. Forconvenience of nursing and post-transplant care,
In terms of unrelated transplants, the cost of the
allo-HSCT in India is generally performed after the
graft source may have a major impact in choice of
child is more than 3 years of age.
graft in developing countries. The approximate costof an unrelated umbilical cord blood unit is US
$30,000 while the cost for a matched unrelateddonor stem cells varies between US $12,000 to
Haematopoietic stem cell transplantation requires
30,000 based on the registry. From a purely
significant infrastructure. In the first report by the
financial aspect, haplo-identical donor would be
Worldwide Network for Blood and Marrow
cost effective, provided the outcome was similar
Transplantation, it was concluded that no HSCTs
to unrelated donor transplants.
were performed in countries with less than US $680gross national income (GNI) per capita28. Transplantactivity is concentrated in countries with higher
governmental health care expenditures, higher
Allogeneic HSCT should be offered to patients
GNI per capita, and higher team density. In
where the benefits outweigh the risks. Non-
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
transplant therapy should be compared to HSCT,
blood in recipients of matched sibling allogeneic
before making any recommendations. Counseling
transplants for myeloid malignancies. Blood. 2002;
of the patient and patient preference is extremely
important, as HSCT involves considerable expense,
5. Ballen KK. New trends in umbilical cord blood
often prolonged morbidity and potential fatality.
transplantation. Blood. 2005 May 15; 105(10): 3786-
In developing countries such as in South Asia,
92. Epub 2005 Jan 27.
where the cost is usually borne by the patient and
6. Gratwohl A, Baldomero H, Passweg J. Hematopoietic
family, economic factors need consideration. In
stem cell transplantation activity in Europe. Curr Opin
general, early transplant offers better results than
Hematol. 2013; 20(6): 485-93.doi: 10.1097/MOH.
HSCT performed in advanced disease, but in those
disorders where non-transplant therapy offerssimilar outcomes, HSCT is offered when there is
7. Kekre N, Antin JH. Hematopoietic stem cell trans-
plantation donor sources in the 21st century:
failure of alternative therapy. Aplastic anemia and
choosing the ideal donor when a perfect match does
thalassaemia are the most common non-malignant
not exist. Blood. 2014 Jul 17; 124(3): 334-43. doi:
indications for transplant in South Asia. In haemato-
10.1182/blood-2014-02-514760. Epub 2014 Jun 9.
logical malignancies, cytogenetic and molecularprognostic markers usually guide the timing of
8. Slavin S, Aker M, Shapira MY, Resnick I, Bitan M, Or R.
transplantation. Potential transplant candidates
Reduced-intensity conditioning for the treatment ofmalignant and life-threatening non-malignant
should be referred early to a transplant center where
disorders. Clin Transpl. 2003: 275-82.
facilities for assessment are available. For moredetailed disease specific analysis, the original
9. Ballen KK, Gluckman E, Broxmeyer HE. Umbilical cord
articles should be reviewed.
blood transplantation: the first 25 years and beyond.
Blood. 2013 Jul 25; 122(4): 491-98. doi: 10.1182/
blood-2013-02-453175. Epub 2013 May 14.
10. Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A,
Contribution: This is the sole work of Dr. Rajat
Ballanti S, et al. Full haplotype-mismatched hemato-
poietic stem-cell transplantation: a phase II studyin patients with acute leukemia at high risk of
Conflict-of-interest disclosure: The author declares
relapse. J Clin Oncol. 2005 May 20; 23(15): 3447-54.
no conflict of interest
Epub 2005 Mar 7.
Correspondence: Dr. Rajat Kumar MD (Med), DNB
11. Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al.
(Med), FRCP (London), FRCP (Edin), FRCPC
Treatment of acute leukemia with unmanipulated
Professor, University of Manitoba, Cancer Care
HLA-mismatched/haploidentical blood and bone
Manitoba, 675 McDermot Avenue, Winnipeg, MB
marrow transplantation. Biol Blood Marrow
R3E 0V9, Canada.
Transplant. 2009 Feb; 15(2): 257-65. doi: 10.1016/
j.bbmt.2008.11.025
12. Luznik L, O'Donnell PV, Fuchs EJ. Post-transplantation
cyclophosphamide for tolerance induction in HLA-
haploidentical bone marrow transplantation. Semin
1. Armitage JO. Bone marrow transplantation. N Engl J
Oncol. 2012 Dec; 39(6): 683-93. doi: 10.1053/
Med. 1994 Mar 24; 330(12): 827-38.
2. Copelan EA. Hematopoietic stem-cell trans-
13. Reisner Y, Hagin D, Martelli MF. Haploidentical
plantation. N Engl J Med. 2006 Apr 27; 354(17):
hematopoietic transplantation: current status and
future perspectives. Blood. 2011 Dec 1; 118(23):
6006-17. doi: 10.1182/blood-2011-07-338822. Epub
3. Apperley J, Niederwieser D, Huang XJ, Nagler A, Fuchs
2011 Sep 14.
E, Szer J, et al. Haploidentical HCT – A Global Overview:Comparing Asia, EU and U.S. Biol Blood Marrow
14. Ciurea SO, Bayraktar UD. "No donor"? Consider a
Transplant. 2016 Jan; 22(1): 23-6. doi: 10.1016/
haploidentical transplant. Blood Rev. 2015 Mar;
j.bbmt.2015.11.001. Epub 2015 Nov 10.
29(2): 63-70. doi: 10.1016/j.blre.2014.09.009. Epub
2014 Sep 30.
4. Couban S, Simpson DR, Barnett MJ, Bredeson C,
Hubesch L, Howson-Jan K, et al. A randomized multi-
15. Russell JA, Chaudhry A, Booth K, Brown C, Woodman
center comparison of bone marrow and peripheral
RC, Valentine K, et al. Early outcomes after allogeneic
The Sri Lanka Journal of Haematology
Rajat Kumar. SLJH. 2015; 7(1): 5-14
stem cell transplantation for leukemia and
23. Kumar R, Prem S, Mahapatra M, Seth T, Chowdhary
myelodysplasia without protective isolation: a 10-
DR, Mishra P, et al. Fludarabine, cyclophosphamide
year experience. Biol Blood Marrow Transplant. 2000;
and horse anti-thymocyte globulin conditioning
regimen for allogeneic peripheral blood stem cell
16. Kumar R, Naithani R, Mishra P, Mahapatra M, Seth T,
transplantation performed in non-HEPA filter rooms
Dolai TK, et al. Allogeneic hematopoietic SCT
for multiply transfused patients with severe aplastic
performed in non-HEPA filter rooms: initial
anemia. Bone Marrow Transplant. 2006 Apr; 37(8):
experience from a single center in India. Bone Marrow
Transplant. 2009 Jan; 43(2): 115-19. doi: 10.1038/
24. George B, Mathews V, Viswabandya A, Kavitha ML,
bmt.2008.307. Epub 2008 Sep 15.
Srivastava A, Chandy M. Fludarabine and cyclo-
17. Seth T, Kanga U, Sood P, Sharma V, Mishra P,
phosphamide based reduced intensity conditioning
Mahapatra M. Audit of peripheral stem cell trans-
(RIC) regimens reduce rejection and improve outcome
plantation for aplastic anemia in multitransfused
in Indian patients undergoing allogeneic stem cell
infected patients. Transplant Proc. 2012 May; 44(4):
transplantation for severe aplastic anemia. Bone
Marrow Transplant. 2007 Jul; 40(1): 13-8. Epub 2007
18. Lazarus HM, Trehan S, Miller R, Fox RM, Creger RJ,
Raaf JH. Multi-purpose silastic dual-lumen central
25. Kumar R, Kimura F, Ahn KW, Hu ZH, Kuwatsuka Y, Klein
venous catheters for both collection and trans-
JP, et al. Comparing Outcomes with Bone Marrow or
plantation of hematopoietic progenitor cells. Bone
Peripheral Blood Stem Cells as Graft Source for
Marrow Transplant. 2000 Apr; 25(7): 779-85.
Matched Sibling Transplants in Severe Aplastic
19. Gratwohl A, Brand R, Frassoni F, Rocha V, Nieder-
Anemia across Different Economic Regions. Biol
wieser D, Reusser P, et al. Cause of death after
Blood Marrow Transplant. 2016 Jan 18. pii: S1083-
allogeneic haematopoietic stem cell transplantation
(HSCT) in early leukaemias: an EBMT analysis of
26. Lucarelli G, Galimberti M, Polchi P, Angelucci E,
lethal infectious complications and changes over
Baronciani D, Giardini C, et al. Marrow trans-
calendar time. Bone Marrow Transplant. 2005 Nov;
plantation in patients with thalassemia responsive
to iron chelation therapy. N Engl J Med. 1993 Sep 16;
20. Bacigalupo A. Bone marrow transplantation for
acquired severe aplastic anemia. Hematol Oncol Clin
27. Chandy M, Srivastava A, Dennison D, Mathews V,
North Am. 2014 Dec; 28(6): 1145-55. doi: 10.1016/
George B. Allogeneic bone marrow transplantation
j.hoc.2014.08.004. Epub 2014 Oct 5.
in the developing world: experience from a center in
21. Schrezenmeier H, Passweg JR, Marsh JC, Bacigalupo
India. Bone Marrow Transplant. 2001 Apr; 27(8):
A, Bredeson CN, Bullorsky E, Camitta BM, et al. Worse
outcome and more chronic GVHD with peripheralblood progenitor cells than bone marrow in HLA-
28. Gratwohl A, Baldomero H, Aljurf M, Pasquini MC,
matched sibling donor transplants for young patients
Bouzas LF, Yoshimi A, et al. Hematopoietic stem cell
with severe acquired aplastic anemia. Blood. 2007
transplantation: a global perspective. JAMA. 2010
Aug 15; 110(4): 1397-400. Epub 2007 May 2.
Apr 28; 303(16): 1617-24. doi: 10.1001/jama.
2010.491.
22. Bacigalupo A, Socie G, Schrezenmeier H, Tichelli A,
Locasciulli A, Fuehrer M,et al. Bone marrow versus
29. Gratwohl A, Baldomero H, Gratwohl M, Aljurf M,
peripheral blood as the stem cell source for sibling
Bouzas LF, Horowitz M, et al. Quantitative and quali-
transplants in acquired aplastic anemia: survival
tative differences in use and trends of hematopoietic
advantage for bone marrow in all age groups.
stem cell transplantation: a Global Observational
Haematologica. 2012 Aug; 97(8): 1142-48. Epub 2012
Study. Haematologica. 2013 Aug; 98(8): 1282-90. doi:
10.3324/haematol.2012.076349. Epub 2013 Mar 18.
The Sri Lanka Journal of Haematology
MB Agarwal
7 LJH. 2015;
(1): 15-18 7(1): 15-18
Treatment of elderly acute myeloblastic leukaemia with azacitidine after failure
of decitabine
MB Agarwal1
Key words: acute myeloblastic leukaemia, azacitidine, decitabine
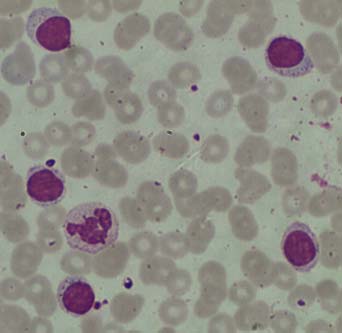
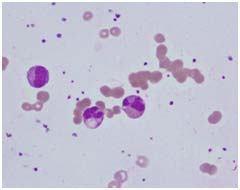
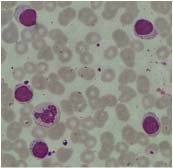
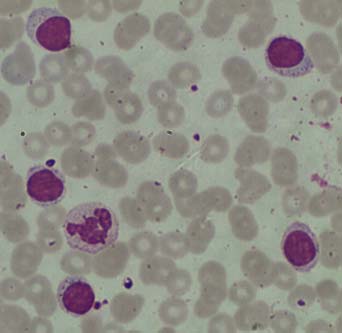
purpuric spots all over the body and oral cavity. His
A 72-year-old man was seen with acute myelo-
haemoglobin (Hb) level was 51 g/L, platelet count
blastic leukaemia (AML) after negligible response
26 x 109/L, WBC count 2.8 x 109/L with 18% blasts in
to four cycles of decitabine. Patient was treated
peripheral blood and 78% blasts in the marrow.
with subcutaneous 5-azacitidine 75 mg/m2 daily x
There were dysplastic changes in all 3 cell lines.
7 days/cycle. Patient achieved complete remission
Immunophenotyping confirmed AML with CD13,
with incomplete recovery of blood counts (CRi)
CD33, CD117, CD34, HLA-DR and cMPO posi-
after 6 cycles and has been on maintenance cycles
tivity. Cytogenetic studies showed 7-monosomy.
with the same schedule for another 8 months so far.
Molecular studies showed no evidence of nucleo-
There is very little data to support use of 5-azacitidine
phosmin (NPM1) gene mutation or FMS-like tyro-
in elderly AML after failure of decitabine and hence
sine kinase-3 internal tandem duplication muta-
this report.
tions (FLT3/ITD) mutation. Patient had performancestatus of two. He had no comorbidities.
Case report
He desired therapy with minimal toxicity over and
A 72-year-old man was seen for AML. He had
above best supportive care. However, he had no
symptoms of weakness and episodic fever. There
interest in standard chemotherapy using 3+7
was easy bruising and one episode of epistaxis.
protocol or reduced intensity transplant. In view
Earlier, at another centre, he was diagnosed as AML
of this, he was started on subcutaneous (SC)
6 months earlier. He had presented with vague
azacitidine 75 mg/m2 x 7 days every 28 days on
systemic symptoms, pancytopenia with marrow
outdoor basis. He was also on levofloxacin and
showing 30% blasts. During those 6 months, he had
voriconazole prophylaxis. The patient had local
received 4 cycles of decitabine 20 mg/m2 daily x 5
reactions at injection sites, episodic significant
days per cycle as intravenous infusion therapy.
gastrointestinal disturbances and continuous
Throughout this period, patient was off and on
requirement of blood products. However, by the
extremely sick due to anaemia and recurrent
end of third cycle, there was significant decrease
infections needing repeated hospitalizations and
in transfusion requirement and peripheral blood
blood component support. Marrow repeated after
counts showed improvement. By the end of 6th
2 cycles had shown 28% blasts and the same after
cycle, he had a Hb level of 92 g/L, platelet count
4 cycles had shown 52% blasts. His subsequenttreatment was abandoned and he was advised
of 86 x 109/L (unsupported), WBC count of 6.4 x
best supportive care.
109/L with absolute neutrophil count (ANC) of 4.9 x109/L and no blasts in peripheral blood. Marrow
At presentation to us, patient was sick, febrile with
examination showed good cellularity, minimal
mild hepatosplenomegaly (1 cm each) and
trilineage dysplasia with blasts < 1%. Cytogeneticstudies showed persistence of 7-monosomy.
Patient was reluctant to continue further treat-
1Professor and Head, Department of Haematology,
ment. However, he was convinced and he con-
Bombay Hospital Institute of Medical Sciences,
tinued the same treatment with almost no toxicity.
Mumbai, India.
By May 2015, he had completed total of 14 cycles
The Sri Lanka Journal of Haematology
MB Agarwal SLJH. 2015; 7(1): 15-18
and he was in complete remission (CR) with Hb
was revived as their use in low dose worked as
level of 124 g/L, platelet count of 136 x 109/L, WBC
differentiating agents with good success and
count of 5.6 x 109/L with ANC of 2.9 x 109/L and no
minimal toxicity. With accumulation of substantial
blasts in the peripheral blood. Bone marrow was
data, 5-azacitidine received United States Food and
not repeated.
Drug Administration (US-FDA) approval for treat-ment of MDS in 2004 and decitabine received the
same in 2006.
This is an interesting case where a number of
Over last few years, HMA were considered as an
lessons could be learnt.
attractive strategy for treating patients of AML whowere otherwise considered unsuitable for 3+7
The incidence of AML in patients over 70 years old
therapy. Azacitidine was compared with various
is > 20 times greater than that observed in younger
conventional care regimens (CCR) which included
subjects. Elderly AML differ from young patients
LD-AraC, intensive chemotherapy or supportive
in various ways; high incidence of poor prognostic cyto-
care (phase 3 trial) in patients with intermediate-
genetic abnormalities, high incidence of therapy-
2 and high-risk MDS. Interestingly, 113 patients in
related leukaemia, association with a prior haema-
this series had blasts between 20% and 29% and
tological disease, often presence of multi-drug
therefore, these were cases of AML with low blast
resistance gene expression and high incidence of
counts. Complete remission rates were similar in
comorbidities and poor tolerance to chemotherapy.
the two arms (18% vs 16%)1.
Overall, there is reluctance in treating elderly AML,
Subsequently, azacitidine vs CCR was studied in
especially in the developing world. Achievement
elderly AML with any blast count. Azacitidine
of CR improves the quality of life and may also add
showed improved median OS (10.4 months vs 6.5
to the duration of life. Hence, it makes sense to
months, p=0.08). This was statistically significant.
have a therapeutic plan with positive intentions
A pre-planned sensitivity analysis censored for
even for such patients.
subsequent AML treatment showed a benefit in
Although, there is no standard treatment regimen,
terms of median OS of 12.1 months vs 6.9 months
elderly AML can be treated with one of the follo-
for azacitidine2. Currently, azacitidine has licensed
wing options; standard induction therapy using 3+7
approval from European Medicines Agency (EMA)
regime consisting of anthracyclin and cytosine
for AML with 20% - 30% blast cell count.
arabinoside (Ara-C) with or without reduced intensitybone marrow transplantation, hypomethylating
Decitabine 20 mg/m2 daily for 5 days per cycle has
agents (HMA), low-dose cytosine arabinoside (LD-
also been studied against CCR in a phase 3 trial of
AraC), best supportive care (BSC) and clinical trial.
485 patients of AML above the age of 65 years.
There was a higher response (CR + CRi 17.8% vs
Standard induction therapy which is best for
7.8%) and better survival. This reached statistical
younger subjects may be the first choice even in
significance (median OS 7.7 vs 5.0 months)3.
elderly AML, however, there is early death of 15%
Currently, decitabine has approval by EMA for
in most of the studies. Development of hypo-
patients of 65 years and above with AML who are
methylating agents (HMA) has brought out a new
not considered candidates for standard induction
ray of hope in this group of AML patients.
Hypomethylating agents were discovered almost
Both azacitidine and decitabine have been
50 years ago. Initially, they were used in high doses
approved by the US-FDA for AML with 20% to 30%
for treating AML. Results with 3+7 protocol were
of blasts. Studies have shown that Ten-Elevan-
superior and hence HMA were almost forgotten.
Translocation-2 (TET2) and DNA methyltransferase
In early part of this century, the interest in HMA
3A (DNMT3A) mutated AMLs benefit from these
for treating myelodysplastic syndrome (MDS)
epigenetic agents4.
The Sri Lanka Journal of Haematology
MB Agarwal SLJH. 2015; 7(1): 15-18
Decitabine has also been used in another more
may be no cross resistance between these two
intensified dose schedule of 20 mg/m2 daily for 10
HMA. Recently, we have used azacitidine + lenali-
days in 53 patients with median age of 74 years
domide after failure of decitabine with good success
and the outcome was encouraging5. Complete
(unpublished observation). Future probably lies
remission rate was 47% and CRIi 17%.
in rationally designed combination therapy inthese otherwise difficult to treat patients.
Dombret et al.6 have published the results ofinternational phase 3 study of azacitidine vs
conventional care regimens in older patients with
Contribution: This is the sole work of Dr. M.B.
newly diagnosed AML with >30% blasts. This is a
study of 488 patients over the age of 65 years withnewly diagnosed AML having over 30% marrow
Conflict-of-interest disclosure: The author declares
blasts. Median overall survival (OS) was longer
no conflict of interest.
with azacitidine vs CCR i.e. 10.4 months vs 6.5
Correspondence: Dr. M.B. Agarwal MD, Professor
months. Univariate analysis showed favourable
and Head, Department of Haematology, Bombay
trends for azacitidine compared with CCR across
Hospital Institute of Medical Sciences, Mumbai,
all subgroups. They concluded azacitidine as an
important treatment option for this difficult to
treat AML population.
Ramos F et al.7 on behalf of European AML investi-
gators have published their observations in using
1. Fenaux P, Mufti GJ, Hellström-Lindberg E, Santini V,
azacitidine as frontline therapy for unfit AML
Gattermann N, Germing U, et al. Azacitidine prolongs
patients. This study includes newly diagnosed unfit
overall survival compared with conventional care
patients of AML treated in France, Austria and Italy.
regimens in elderly patients with low bone marrow
European LeukaemiaNet response was achieved
blast count acute myeloid leukaemia. J Clin Oncol.
in 21.0% of 371 patients. This did not depend on
2010; 28(4): 562-569. DOI: 10.1200/JCO.2009.23.
bone marrow blast cell percentage. Median OS was
9.6 months and 40.6% of patients were alive at one
2. Dombret H, Seymour JF, Butrym A, et al. Results of a
phase 3, multi-centre, randomized, open-label studyof Azacitidine vs conventional care regimens in older
Lao Z et al.8 concluded that treatment of azacitidine
patients with newly diagnosed AML. Haematologica.
in elderly subjects with AML leads to fewer hospi-
2014; 99(S1). Abstract LB6212.
talisation days and infective complications but
3. Thomas XG, Arthur C, Delaunay J, Jones M, Berrak E,
similar survival compared with intensive chemo-
Kantarjian HM. A post hoc sensitivity analysis of
survival probabilities in a multinational phase IIItrial of decitabine in older patients with newly
Outcome of patients with AML who have failed
diagnosed acute myeloid leukemia. Clin Lymphoma
treatment with HMA is poor. Median survival is 6
Myeloma Leuk. 2014 Feb; 14(1): 68-72. doi: 10.1016/
months. There is no established therapy available
j.clml.2013.09.007. Epub 2013 Oct 1.
except allogeneic haematopoietic stem cell
4. Im AP, Sehgal AR, Carroll MP, Smith BD, Tefferi A,
Johnson DE, et al. DNMT3A and IDH mutations in acutemyeloid leukemia and other myeloid malignancies:
The choice between azacitidine and decitabine as
associations with prognosis and potential treatment
the initial treatment of MDS or AML remains in
strategies. Leukemia. 2014 Sep; 28(9): 1774-83. doi:
10.1038/leu.2014.124. Epub 2014 Apr 4.
5. Blum W, Garzon R, Klisovic RB, Schwind S, Walker A,
Our patient is unique from the angle that
Geyer S. Clinical response and miR-29b predictive
azacitidine worked after failure of decitabine. This
significance in older AML patients treated with a 10-
goes to show that there are subjects where there
day schedule of decitabine. Proc Natl Acad Sci U S A.
The Sri Lanka Journal of Haematology
MB Agarwal SLJH. 2015; 7(1): 15-18
2010 Apr 20; 107(16): 7473-8. doi: 10.1073/pnas.
acute myeloid leukemia patients: clinical use and
1002650107. Epub 2010 Apr 5.
outcome prediction. Leuk Res. 2015 Mar; 39(3):296-
306. doi: 10.1016/j.leukres.2014.12.013. Epub 2014
6. Dombret H, Seymour JF, Butrym A, Wierzbowska A,
Selleslag D, Jang JH, et al. International phase 3study of azacitidine vs conventional care regimens
8. Lao Z, Yiu R, Wong GC, Ho A. Treatment of elderly
in older patients with newly diagnosed AML with
patients with acute myeloid leukemia with
>30% blasts. Blood. 2015 Jul 16; 126(3): 291-9. doi:
azacitidine results in fewer hospitalization days
10.1182/blood-2015-01-621664. Epub 2015 May 18.
and infective complications but similar survivalcompared with intensive chemotherapy. Asia Pac J
7. Ramos F, Thépot S, Pleyer L, Maurillo L, Itzykson R,
Clin Oncol. 2015 Mar; 11(1): 54-61. doi: 10.1111/
Bargay J, et al. Azacitidine frontline therapy for unfit
ajco.12331. Epub 2014 Dec 28.
The Sri Lanka Journal of Haematology
WHE Alwis and N Ranasinghe. SLJH. 2015; 7(1): 19-23
SLJH. 2015; 7(1): 19-23
Hospital admission rate, pattern of lower limb deep vein thrombosis (DVT)
and its relationship to acquired risk factors among patients admitted to
Colombo South Teaching Hospital (CSTH) during the year 2010
WHE Alwis1, N Ranasinghe2
Key words: deep vein thrombosis, risk factors, hospital admission
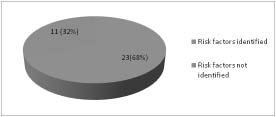
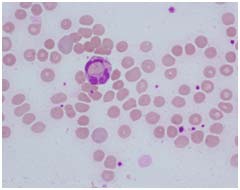
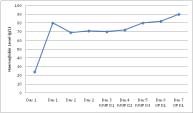
Proximal DVT refers to involvement of poplitealveins or above and isolated calf vein thrombosis is
Deep vein thrombosis (DVT) confers considerable
considered as distal vein thrombosis.1 The clinical
mortality and morbidity. However there is hardly
conundrum is that symptoms (pain and swelling)
any data available on prevalence and pattern of
are often nonspecific or absent. However if left
DVT among the Sri Lankan population. The study
untreated a thrombus could become fragmented
was carried out with the aim of assessing hospital
or dislodged and migrate to obstruct the arterial
admission rate, pattern of lower limb DVT (LL-DVT)
supply to the lungs causing potentially life
and its relationship to acquired risk factors among
threatening pulmonary embolism. Over the past
patients admitted to a tertiary care hospital. Total
25 years the pathophysiology of DVT has become
of 34 patients were identified with LL-DVT for the
much better understood. Over a century ago Rudolf
year 2010. Data were collected from bed head
Virchow described three features which are
tickets of discharged patients, anti-coagulation
critically important in the development of venous
clinic records and doppler ultrasound scan lists. The
thrombosis2; venous stasis, activation of blood
hospital admission rate of LL-DVT among the study
coagulation, and venous damage.
population was 25 per 100,000 admissions per year.
Sixty five percent (n=22) had proximal LL-DVT
These factors are known as the "Virchow Triad".
whereas 21% (n=7) had distal LL-DVT. An acquired
Under normal circumstances a physiologic balance
risk factor was identified in 68% (n=23). Forty eight
is present between factors that promote and retard
percent (n=11) of patients had immobility as an
coagulation. A disturbance in this equilibrium may
acquired risk factor and 26% (n=6) of patients had
result in the coagulation process occurring at an
multiple risk factors. Eight patients (47%) with
inopportune time or location or in an excessive
proximal LL-DVT had non transient risk factors
manner. Numerous factors, often in combination
compared to none of the patients with distal LL-
contribute to DVT. These may be categorized as
DVT. Being more than 40 years and female had
acquired or inherited. Acquired risk factors could
more events of LL-DVT compared to <40 years and
be of two types and include transient acquired risk
males (P<0.05).
factors (e.g. pregnancy, post-operative) and non-transient acquired risk factors (cancer, antiphos-
pholipid syndrome). The diagnosis of DVT histori-
Deep vein thrombosis (DVT) refers to the
cally required venography which is expensive and
formation of one or more thrombi in one of body's
invasive. Even though venography is considered
large veins most commonly in the lower limbs.
the criterion of standard since 1990 most widelyused method for diagnosis is non-invasive sono-graphic examination.3 The simple and cheaper D-
1Speciality Doctor in Haematology, Great Western
dimer test has been validated as an initial scree-
Hospital, Swindon, UK. 2Consultant Haematologist,
ning test and confers a high negative predictive
Colombo South Teaching Hospital, Kalubowila, Sri
value when it is negative with a low clinical pro-
The Sri Lanka Journal of Haematology
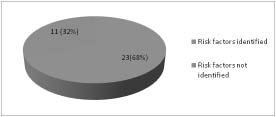
WHE Alwis and N Ranasinghe. SLJH. 2015; 7(1): 19-23
Early recognition and appropriate treatment of DVT
detected were 34. Therefore, the hospital admission
and its complications can save many lives. Similarly
rate of LL-DVT among the study population was 25
recognition of high risk individuals and initiation
per 100,000 admissions per year. The age distri-
of thromboprophylaxis can be not only lifesaving
bution of the study population was from 19 years
but also much more cost effective. There is no
to 81 years and the median age was 41 years (Table
country data for hospital admission rates for DVT
1). Females had significantly more LL-DVT com-
and its pattern in Sri Lanka. The purpose of this
pared to males being 73.5% vs 26.5% (p<0.001).
study was to determine the hospital admission
Proximal DVT was higher than distal DVT (Table 2).
rate, pattern of lower limb DVT and its relationshipto acquired risk factors among patients admitted
Table 1. Age distribution of the
to Colombo South Teaching Hospital during the
Age category
A descriptive cross sectional study was carried out
at the Haematology Department, Colombo SouthTeaching Hospital (CSTH) among patients admitted
during the year 2010 with lower limb DVT (LL-DVT).
All patients with LL-DVT admitted during the year2010 were identified from the doppler ultrasound
Table 2. Distribution of the site
scan list available at the Radiology Department,
CSTH. This was further supported by the anti-coagulation clinic register at the Haematology
Site of LL-DVT
Department, CSTH where there is a record of all
the patients referred for further management and
follow up. Patients' details such as demographicdata, risk factors for LL-DVT and investigations
related to LL-DVT were obtained from their bed
head tickets and the anticoagulation clinic book.
Transient risk factors for LL-DVT such as pregnancy,
(LL - DVT : Lower limb deep vein thrombosis)
postpartum period, immobility, post-operativeperiod, intensive care unit admission, pharma-
An acquired risk factor was present in 68% (n=23)
cological agents, trauma, other co-morbid factors
(Figure 1). A single risk factor was present in 74%
(e.g. presence of uterine fibroids) were recorded.
(n=17) and 26% (n=6) had multiple risk factors.
The non-transient risk factors assessed were anti-
Immobility was the commonest risk factor identi-
phospholipid syndrome (APLS), cancer, varicose
fied, followed by pregnancy and puerperium, and
veins, and congestive cardiac failure, and myelo-
presence of APLS and cancer / a MPN (Table 3).
proliferative neoplasm (MPN). Data collection was
When the risk factors were categorized 52 % (n=12)
done for a period of three months. A data extraction
were transient risk factors and 48% (n=11) were
sheet was used for data collection. All components
non-transient (Table 4).
of the data collection format were manuallychecked and data cleaning and coding was done.
Data entry and statistical analyses were done usingthe software package SPSS (version 15). Ethicalclearance for the study was obtained from theethical review committee of the CSTH.
Total admissions for the year 2010 to CSTH were
Figure 1. Distribution of risk factors in the
136,794. The total number of LL-DVT patients
The Sri Lanka Journal of Haematology
WHE Alwis and N Ranasinghe. SLJH. 2015; 7(1): 19-23
Table 3. Distribution of risk factor types
Risk factor
Pregnancy and puerperium
Intensive care unit admission
Congestive cardiac failure
Table 4. Distribution of risk factors by site
Site of LL-DVT
Non Transient
LL-DVT: Lower limb deep vein thrombosis
In the study population proximal LL-DVT wascommoner than distal LL-DVT or LL-DVT occurring
The annual hospital admission rate of LL-DVT
in both distal and proximal veins (Table 2). Varying
among the study population was 25 per 100,000
results have been reported in the world literature
admissions. This is a rising trend compared to what
for the frequencies of distal versus proximal vein
White et al. reported in 2005 of the rate of DVTamong Asians/Pacific Islanders living in California
thrombosis. Some report as distal DVT being com-
which was 21 per 100,000.4 This may reflect the
moner while others report an opposite view.9,10
rising trend in line with studies done in Singapore
The diagnostic strategies looking mainly into
which concluded that even though DVT is not
proximal vein thrombosis could be a one reason
common in Asians as it is in Caucasians, the pre-
for this observation and it is also well recognized
valence now is much higher than it was earlier.5-7 The
that ultrasound scan being particularly user
relationship of LL-DVT to age and gender was
dependent and detection rates of distal LL-DVT
similar to what is reported in other populations;
vary considerably between operators and depart-
where elderly females have a higher tendency to
ments.11,12 Another contributing factor for this could
be variations in lower limb venous anatomy.13
The Sri Lanka Journal of Haematology
WHE Alwis and N Ranasinghe. SLJH. 2015; 7(1): 19-23
The relationship between LL-DVT and associated
risk factors were analyzed in the study. Majority
Contribution: Both authors contributed equally.
68% (n=23) had acquired risk factors. Immobilitywas the most common risk factor (47.8%), while
Conflict-of-interest disclosure: The authors declare
malignancy/ MPN, pregnancy and APLS were also
no conflict of interest.
among the risk factors (Table 3). These results are
Correspondence: Dr. WHE Alwis, Haematology
similar to data reported in Asian DVT cohorts and
Department, Great Western Hospital, Swindon,
world literature.7,14,15 It is important to note that
SN36B, United Kingdom.
26.1% of patients had multiple risk factors.
It was found that proximal LL-DVT and extensiveLL-DVT (LL-DVT involving both proximal and distalveins) are commonly associated with non-transient
risk factors (malignancy, APLS, congestive heart
The authors would like to acknowledge the director
failure, autoimmune haemolysis and varicose
of Colombo South Teaching Hospital, Kalubowila,
veins). None of the patients with distal LL-DVT had
Sri Lanka for giving permission to carry out this
non-transient risk factors (Table 4). This finding
study. They also gratefully acknowledge the
support reported data on the risk factors on distal
cooperation of all staff and patients involved in
versus proximal thrombosis.9 Approximately equal
percentages of proximal and distal LL-DVT wereassociated with transient risk factors; 41% and 43%respectively in this study. (9/22 patients with
proximal DVT and 3/7 patients with distal DVT had
1. Guidelines on oral anticoagulation with warfarin –
transient risk factors – Table 2 and Table 4). Therefore
fourth edition. Keeling D, Baglin T, Tait C, Watson H,
we cannot conclude that distal LL-DVT is more
Perry D, Baglin C, Kitchen S, Makris M; British
commonly associated with transient risk factors
Committee for Standards in Haematology. Br J
compared to proximal LL- DVT.9
Haematol. 2011 Aug; 154(3): 311-24. doi: 10.1111/
j.1365-2141.2011.08753.x. Epub 2011 Jun 14.
The main limitation of the study was the small
2. Dickson BC. Venous thrombosis: on the history of
sample size. Smoking is well known risk factor
Virchow's triad. University of Toronto Medical Journal.
associated with DVT16. This was not analyzed as
2004; 81: 166-71.
the study was mainly based on case notes and
3. Bates SM, Jaeschke R, Stevens SM, Goodacre S, Wells
patients were not directly interviewed. An
PS, Stevenson MD, et al. American College of Chest
acquired risk factor was not identified in a total of
Physicians. Diagnosis of DVT: Antithrombotic Therapy
11 patients. These patients may have an acquired
and Prevention of Thrombosis, 9th ed: American
risk factor which was not studied or have an
College of Chest Physicians Evidence-Based Clinical
inherited risk factor. Inherited thrombophilia as a
Practice Guidelines. Chest. 2012 Feb; 141(2Suppl):
risk factor was not analyzed during the study.
e351S-418S. doi: 10.1378/chest.11-2299.
4. White RH, Zhou H, Murin S, Harvey D. Effect of
Conclusions and recommendations
ethnicity and gender on the incidence of venousthromboembolism in a diverse population in
It is the standard practice in most of the developed
California in 1996. Thromb Haemost. 2005 Feb; 93(2):
countries including United Kingdom to assess the
risk of thrombosis in hospitalized patients and
5. White RH. The epidemiology of venous throm-
provide appropriate thromboprophylaxis. It is
boembolism. Circulation. 2003 Jun 17; 107(23 Suppl
widely accepted that this is the most cost effective
way of reducing death associated with VTE,
6. Yeo DX, Junnarkar S, Balasubramaniam S, Tan YP, Low
reducing the treatment cost in DVT and treatment
JK, Woon W, et al. Incidence of venous thrombo-
cost in long term complications.17 Therefore it is
embolism and its pharmacological prophylaxis in
important for us to think about a national guideline
Asian general surgery patients: a systematic review.
and protocol based on the guideline for prevention
World J Surg. 2015 Jan; 39(1): 150-7. doi: 10.1007/
of thrombosis.
The Sri Lanka Journal of Haematology
WHE Alwis and N Ranasinghe. SLJH. 2015; 7(1): 19-23
7. Lee LH. Clinical update on deep vein thrombosis in
institution. Thromb Haemost. 2009 Jun; 101(6):
Singapore. Ann Acad Med Singapore. 2002 Mar; 31(2):
13. Quinlan DJ, Alikhan R, Gishen P, Sidhu PS. Variations
8. Silverstein MD, Heit JA, Mohr DN, Petterson TM,
in lower limb venous anatomy: implications for US
O'Fallon WM, Melton LJ 3rd. Trends in the incidence
diagnosis of deep vein thrombosis. Radiology. 2003
of deep vein thrombosis and pulmonary embolism:
Aug; 228(2): 443-8. Epub 2003 Jun 23.
a 25-year population-based study. Arch Intern Med.
1998 Mar 23; 158(6): 585-93.
14. Wakefield TW, McLafferty RB, Lohr JM, Caprini JA,
Gillespie DL, Passman MA. Executive Committee of
9. Galanaud JP, Sevestre-Pietri MA, Bosson JL, Laroche
the American Venous Forum. Call to action to prevent
JP, Righini M, Brisot D, et al. OPTIMEV-SFMVInvestigators. Comparative study on risk factors and
venous thromboembolism. J Vasc Surg. 2009 Jun;
early outcome of symptomatic distal versus proximal
49(6): 1620-3. doi: 10.1016/j.jvs.2009.01.058.
deep vein thrombosis: results from the OPTIMEV
15. Rocha AT, Paiva EF, Lichtenstein A, Milani R Jr,
study. Thromb Haemost. 2009 Sep; 102(3):493-500.
Cavalheiro CF, Maffei FH. Risk-assessment algorithm
and recommendations for venous thromboembolism
10. Labruto F, Westerberg M, Magnusson M. Deep venous
prophylaxis in medical patients. Vasc Health Risk
thrombosis of the lower limb: no difference in
Manag. 2007; 3(4): 533-53.
duration of symptoms between proximal and distal
disease. Clin Appl Thromb Hemost. 2011 Aug; 17(4):
16. Golomb BA, Chan VT, Denenberg JO, Koperski S, Criqui
393-5. doi: 10.1177/1076029610368672. Epub 2010
MH. Risk marker associations with venous throm-
botic events: a cross-sectional analysis. BMJ Open.
2014 Mar 21; 4(3): e003208. doi: 10.1136/bmjopen-
11. Cowell GW, Reid JH, Simpson AJ, Murchison JT. A
profile of lower-limb deep-vein thrombosis: thehidden menace of below-knee DVT. Clin Radiol. 2007
17. NICE guideline CG 92 Venous thromboembolism –
Sep; 62(9): 858-63; discussion 864-5. Epub 2007
Reducing the risk for patients in hospital January
2010. Availabe at https://www.nice.org.uk/guidance/
12. Ng HJ, Lee LH. Trends in prevalence of deep venous
cg92/chapter/Introduction. [Accessed 15 February
thrombosis among hospitalised patients in an Asian
The Sri Lanka Journal of Haematology
SLJH. 2015; 7(1): 24
CME Article (Series III)
Theme: Acute trauma coagulopathy and massive transfusion
HWCK Kulathilake1, I Wijesiriwardena1
Questions 1 and 2 are multiple choice questions to activate your brain cells to the pathogenesis of acute
trauma coagulopathy (ATC) and massive transfusion, as there are new insights into this subject.
Acute trauma coagulopathy
is initiated by vascular endothelial damage
b) protein C activation pathway is one of the major contributors to its pathogenesis
has the same pathophysiology of disseminated intravascular coagulation (DIC)
d) haemodilution is beneficial in prevention of ATC
e) hypothermia aggravates the condition
Complications of massive transfusion include
e) metabolic alkalosis
Answer Grid:
The answers are given in page 33 with the explanations.
1Senior Lecturer, Consultant Haematologist,
Department of Pathology, University of SriJayawardenapura, Sri Lanka.
Correspondence: Dr. I WijesiriwardenaE-mail: [email protected]
The Sri Lanka Journal of Haematology
EL Asfir et al.
. 2015; 7 JH. 2015;
(1): 25-28 7(1): 25-28
Case report I
Paroxysmal cold haemoglobinuria in a pregnant woman leading to severe
anaemia and fetal loss
EL Asfir1, N Senadheera2, S Jayasinghe3, H Liyanage3
Key words: paroxysmal cold haemoglobinuria; steroids; fetal loss
Case report
Paroxysmal cold haemoglobinuria (PCH) is an
A 23-year-old female in her second pregnancy, pre-
autoimmune haemolytic anaemia which gives rise
sented to a local hospital at 32 weeks of gestation,
to intravascular haemolysis and a varying degree
with evidence of intravascular haemolysis and was
of anaemia. Its presentation in pregnancy is rare
transferred to our hospital, a tertiary care women'shospital for specialized care.
but can be potentially fatal to both mother andfetus. This case report describes a pregnant woman
This presentation was while convalescing following
with PCH presenting with acute severe anaemia
a chickenpox infection, and she had developed
which led to fetal loss. The mother was successfully
fever and lower abdominal pain immediately after
managed with blood transfusions and steroid
a cold bath. This was associated with passage of
therapy. We stress the importance of timely
dark urine. On admission to the local hospital, she
intervention when managing similar patients.
was very pale and icteric and the haemoglobin (Hb)level was 54 g/L. As facilities for transfusion wasnot available in this hospital she had to be trans-
ferred to the nearest provincial general hospital.
Paroxysmal cold haemoglobinuria (PCH) is a rare
There the investigations carried out detected a
form of autoimmune haemolytic anaemia more
positive direct antiglobulin test (DAT) and indirect
commonly seen in children. Historically this was
hyperbilirubinaemia. By this time she complained
described in association with syphilis but nowa-
of reduced fetal movements and an ultrasoundscan done showed absence of fetal heart beat con-
days it's mostly seen following viral or bacterial
firming an intrauterine fetal death (IUD). As com-
infections1-5. The haemolysisin PCH is mediated
patible blood for transfusion could not be provided
by a biphasic IgG autoantibody that triggers com-
she was transferred to our hospital.
plement – mediated intravascular haemolysis.1-4In adults, it is rare and represents less than 1% of
On arrival she was drowsy, dyspnoeic, pale, icteric,
all autoimmune haemolytic anaemias.6
blood pressure was 85/50mmHg. The Hb level was24 g/L, packed cell volume (PCV) 6.1%, white cell
We report a case of a pregnant woman who pre-
count (WBC) 17.3x109/L, with neutrophils – 78%
sented with acute severe haemolysis and fetal loss,
and lymphocytes – 21%. Platelet count – 437x109/L,
and diagnosed as having PCH and successfully
indirect bilirubin level – 8.4mg/dL and the potas-
managed with blood transfusions and steroids. To
sium level – 6.8mmol/L. Blood picture showed redcell agglutination, many spherocytes, occasional
our knowledge PCH presenting in pregnancy has
polychromatic cells, occasional fragmented red
been reported only once before in the literature.7
cells and neutrophil erythrophagocytosis. (Figure1 & 2). Absolute reticulocyte count was 0.6 x 109/Land reticulocyte index was 0.2%. Serum LactateDehydrogenase (LDH) level was elevated (3250u/L). The DAT was strongly positive with anti-C3d but
1Senior Registrar, Critical Care Medicine, 2Consultant
negative with anti-IgG. Mycoplasma antibody was
Haematologist, 3Consultant Anesthetist, De Soysa
negative. Indirect Donath-Landsteiner (DL) test was
Hospital for Women, Sri Lanka.
positive confirming PCH.
The Sri Lanka Journal of Haematology
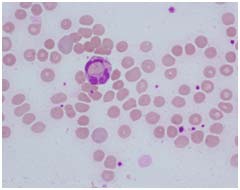
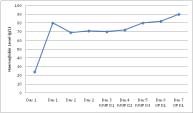
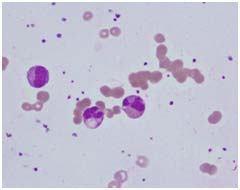
EL Asfir et al. SLJH. 2015; 7(1): 25-28
Figure 1. Peripheral blood smear (Leishman
Figure 2. Peripheral blood smear (Leishman
stain, x 100) – Showing erythrocyte
stain, x 100) – Showing erythrophagocytosis
She was managed in the Intensive care unit as shewas drowsy and dyspnoeic, and then was keptwarm and two units of uncross matched O negativepacked red blood cells were given soon afteradmission via the blood warmer and followed byone unit of cross matched washed O positive redcell concentrates. Folic acid 5 mg daily wascommenced on the same day. At the end of dayone the Hb level increased to 80g/L. The dead fetuswas delivered spontaneously on the following day.
Figure 3. Showing the temporal profile of the
On the second day the Hb level dropped again to
69 g/L, and there was a persistently low absolute
(IVMP – Intravenous methyl prednisolone,
reticulocyte count of 1.7 x 109/L and reticulocyte
OP – Oral prednisolone, LDH – Lactate
index was 0.7%. This day the urine output reduced
dehydrogenase level)
to < 0.5ml/kg/h. Another unit of blood was trans-fused. Despite the blood transfusion the Hb level
continued to fall and dropped from 80 g/L to 71 g/Lthe next 24 hours. Therefore intravenous (IV)
At the time PCH was first described by Donath andLandsteiner in 1904, it was a chronic relapsing
methyl prednisolone (MP) 500mg daily was com-
condition affecting mainly adults and 90% were
menced on day three. Following commencement
secondary to syphilis. Since then the presentation
of IVMP, the Hb level improved over the next four
has changed due to the effective treatment of
days to 90 g/L without any further blood trans-
syphilis and now PCH is seen mostly in children as a
fusions and the LDH level gradually came down to
post viral syndrome commonly following infections
1400U/L (Figure 3). The IVMP was given for 3 days
such as chickenpox, mumps and measles. Less com-
followed by oral prednisolone 40mg daily. On
monly, bacterial infections with Haemophilus
discharge she was referred to the local hospital
influenzae, Escherichia coli and Staphylococcus
for follow up. Prednisolone was tailed off over a
aureus have been implicated3,8. The acute non-
few weeks. Her Hb level remained stable at her
relapsing form of PCH has been documented to
follow up visit to the local hospital.
occur in adults9.
The Sri Lanka Journal of Haematology
EL Asfir et al. SLJH. 2015; 7(1): 25-28
Our patient had typical laboratory findings of PCH.
washed RBC units has not been proven to improve
Her DAT was positive for complement C3d but
transfusion safety, but this can be performed if
negative for IgG. Although DL antibodies are of IgG
patient's condition remains refractory to standard
class, this is a common finding in PCH. There are
warmed blood transfusions.13
also reported cases where DAT has been negative.
Non detection of DL antibodies can be due to low-
The severity of anaemia and the reticulocytopenia
affinity of the IgG, the immunoglobulins being RBC-
prompted the initiation of steroids in our patient
bound, or IgG levels being below the threshold
resulting in a dramatic response. There is no uniform
level of the test. Another postulation is that the IgG
consensus on the role of steroids in the manage-
autoantibodies are directed against reticulocytes
ment of PCH but several reports show that it has
or mature RBC precursors rather than red blood cells,
been used successfully in similar circumstances.10
which is based upon the presence of reticulo-
Usually, a remission can be seen in 1 to 3 weeks.
cytopenia in some cases.10 Use of special blood
Once the haemolysis is controlled, corticosteroids
bank techniques may overcome some of these
can be tapered. Close monitoring for relapses is
false negativities.
required for a few weeks, with slowing of cortico-steroid taper if signs of possible relapse develop.
Our patient had a relative reticulocytopenia whichagain is a known finding in PCH.11 This reflects an
The other available treatment options are plasma-
ineffective erythropoiesis either due to des-
pheresis and rituximab therapy.10,14 Given the
truction of precursor red cells by DL antibodies or
transient and relatively brief production of DL
a result of viral haematopoietic suppression.
antibodies after a viral infection, clearance of theantibody may be possible with plasma exchange.
A striking feature in the peripheral blood film was
Another reason for the effectiveness of plasma-
the erythrophagocytosis by neutrophils. Although
pheresis in this condition is that the antibody pre-
erythrophagocytosis by monocytes occur in autoim-
ferentially binds to the RBC, shifting the antibody
mune haemolytic anaemia of various aetiologies,
equilibrium to the intravascular component,
erythrophagocytosis by neutrophils is most strongly
allowing easy removal.10 Rituximab has also been
associated with PCH.12 Other cases where this has
used successfully to treat relapses of chronic PCH
been reported in are cold haemagglutinin disease,
in an adult patient, where disease was unres-
incompatible blood transfusions, haemolytic disease
ponsive to steroids.14 Splenectomy is usually
of the newborn and potassium chloride poisoning.12
ineffective as the haemolysis is intravascular.
Paroxysmal cold haemoglobinuria is usually self
An important issue which was evident in the
limiting and requires only supportive care during
presentation of this patient was a lapse in the
the period of acute haemolysis. However the degree
emergency transfusion facilities in peripheral
of haemolysis may vary between patients because
hospitals. The DAT positivity can pose problems for
the characteristics of the haemolytic antibody are
the blood bank when selecting red cell units by routine
highly variable. The amount of the antibody and
methods. However it needs to be emphasized that
the affinity of the antibody for the red blood cell
transfusion of uncrossmatched group O blood in
surface are important determinants of the severity
such situations is justified and can be lifesaving15.
of haemolysis. Furthermore, some antibodies mayfix complement less efficiently.6 IgG antibodies cancross the placenta and result in haemolysis in the
fetus. Our patient experienced severe haemolysis
Contribution: All authors contributed equally.
and anaemia leading to IUD of the fetus.
Conflict-of-interest disclosure: The authors declareno conflict of interest.
Management includes avoidance of cold tem-perature, folic acid supplements and transfusion
Correspondence: Dr. N Senadheera, Consultant
of red cell concentrates. Uncross matched group O
Haematologist, De Soysa Hospital for Women,
blood can be given until group compatible blood
Colombo 8, Sri Lanka.
is available after cross matching at 37°C. Utilizing
The Sri Lanka Journal of Haematology
EL Asfir et al. SLJH. 2015; 7(1): 25-28
Blajchman MA. Transient Donath-Landsteiner
haemolyticanaemia. Br J Haematol. 1981; 48(3):
1. Bass GF, Tuscano ET, Tuscano JM. Diagnosis and
classification of autoimmune hemolytic anemia.
Autoimmun Rev. 2014 Apr-May; 13(4-5): 560-4. doi:
9. Papalia MA, Schwarer AP. Paroxysmal cold haemo-
10.1016/j.autrev.2013.11.010. Epub 2014 Jan 11.
globinuria in an adult with chicken pox. Br J Haematol.
2000 May; 109(2): 328-9.
2. Sokol RJ, Booker DJ, Stamps R. Paroxysmal cold
hemoglobinuria and the elusive Donath-Landsteiner
10. Gertz MA. Management of cold haemolytic syndrome.
antibody. Immunohematology. 1998; 14(3): 109-12.
Br J Haematol. 2007 Aug; 138(4): 422-9.Epub 2007
Jun 11.
3. Sokol RJ, Hewitt S. Autoimmune hemolysis: a critical
review. Crit Rev Oncol Hematol. 1985; 4(2): 125-54.
11. Sokol RJ, Booker DJ, Stamps R. Erythropoiesis:
Paroxysmal Cold Haemoglobinuria: A Clinico-
4. Sokol RJ, Hewitt S, Booker DJ. Erythrocyte auto-
Pathological Study of Patients with a Positive Donath-
antibodies, autoimmune haemolysis, and myelody-
Landsteiner Test. Hematology. 1999; 4(2): 137-64.
splastic syndromes. J Clin Pathol. 1989 Oct; 42(10):
1088-91.
12. Mukhopadhyay S, Keating L, Souid AK. Erythro-
phagocytosis in Paroxysmal Cold Hemoglobinuria.
5. Sanford KW, Roseff SD. Detection and significance of
Am J Hematol. 2003 Nov; 74(3): 196-7.
Donath-Landsteiner Antibodies in a 5-year-oldFemale Presenting with Hemolytic Anemia. Lab Med.
13. Roy-Burman A, Glader BE. Resolution of severe
2010; 41(4): 209-12.
Donath-Landsteiner autoimmune hemolytic anemiatemporally associated with institution of plasma-
6. Petz LD. Cold antibody autoimmune hemolytic
pheresis. Crit Care Med. 2002 Apr; 30(4): 931-4.
anaemias. Blood Rev. 2008 Jan; 22(1): 1-15. Epub 2007
14. Koppel A, Lim S, Osby M, Garratty G, Goldfinger D.
Rituximab as successful therapy in a patient with
7. Akpoguma AO, Carlisle TL, Lentz SR. Case report:
refractory paroxysmal cold hemoglobinuria.
paroxysmal cold hemoglobinuria presenting during
Transfusion. 2007 Oct; 47(10): 1902-4.
pregnancy. BMC Hematol. 2015; 15: 3. doi:10.1186/
15. Gongal R. How safe is transfusion of uncross-
s12878-015-0023-7.Epub 2015 Feb 13.
matched group-specific blood. Kathmandu Univ Med
8. Wolach B, Heddle N, Barr RD, Zipursky A, Pai KR,
J (KUMJ). 2005 Jan-Mar; 3(1): 76-8.
The Sri Lanka Journal of Haematology
ONKD Gamage et al.
SLJH. 2015; 7
2015; 7(1): 29-31
Case report II
Lupus anticoagulant – hypoprothrombinaemia syndrome
ONKD Gamage1, MM Jayatilaka2, PM Punchihewa3
Key words: bleeding, lupus anticoagulant, acquired hypoprothrombinaemia, systemic lupus
erythematosus
acquired thrombocytopathy.2-4 Lupus anticoa-gulant – hypoprothrombinaemia syndrome (LA-
Lupus anticoagulant – hypoprothrombinaemia
HPS) is a rare acquired disorder caused by pro-
syndrome (LA-HPS) is a rare acquired disorder
thrombin antibodies, in adults or in children mostly
caused by the combination of lupus anticoagulants
associated with systemic lupus erythematosus (SLE),
and anti-prothrombin antibodies. A 6-year-old girl
has been reported to manifest with a bleeding
was admitted with intractable bleeding from a
diathesis caused by factor II(FII) deficiency.3,4
tooth. Both prothrombin time (PT) and activatedpartial thromboplastin time (aPTT) were prolonged
We report the clinical case of a girl whose onset of
with test to control ratio > 3 and aPTT did not getcorrected following 50:50 mix with pooled normal
SLE was a bleeding manifestation caused by a
fresh plasma (PNP); the inhibition was not time
serious coagulopathy with prolonged PT and aPTT
dependent. The PT got corrected following 50:50
in the presence of LA due to a LA-HPS.
mix. Both dilute Russell viper venom time (dRVVT)and kaolin clotting time (KCT) were strongly positive.
Case report
Antinuclear antibody (ANA) and anti-double
A 6-year-old girl was admitted to ward 09, of the Lady
stranded DNA (anti-dsDNA) were positive. Based
Ridgeway Hospital with history of prolonged and
on the coagulation derangements and positivity
excessive bleeding following an accidental injury to
for the lupus anticoagulant (LA) and ANA and DS/
a tooth. The clinical examination was unremarkable
DNA the diagnosis of the rare lupus anticoagulant-
other than the mild bleeding from the tooth socket.
acquired hypoprothrombinemia syndrome (LA-
The girl had no past history of congenital coagulo-
HPS) was made. The patient was treated with high
pathy or other important illnesses. She had no family
dose corticosteroids and normal coagulation test
history of any bleeding disorder. She did not give a
results were obtained.
history of or have clinical features to indicate SLE.
The laboratory investigations on admission were
Lupus anticoagulant (LA) is a group of antibodies
as follows: Full blood count haemoglobin (Hb)
directed against phospholipid binding proteins.
level 131 g/L, red blood cells (RBC) 4.98 x 1012/L,
These phospholipids are essential for the activation
mean cell volume (MCV) 77.8fL, mean cell haemo-
of main steps of the coagulation cascade.1 The LA,
globin (MCH) 26.2 pg, mean cell haemoglobin con-
results in thrombosis in-vivo than bleeding due to
centration (MCHC) 33.7 g/dl, white blood cell count
activation of phospholipids and binding proteins,
(WBC) 12.6 x 109/L with neutrophils -56%,
endothelial activation and inactivation of natural
lymphocytes -34% and monocytes 4%, and platelet
anticoagulants.1 The LA may manifest with bleeding
count 410 x 109/L. Erythrocyte sedimentation rate
when associated with an acquired factor VIII
(ESR) 74 mm 1st hr. Blood picture: RBC showed
inhibitor or rarely due to thrombocytopenia, or an
moderate rouleaux formation and appeared normo-chromic normocytic. WBC and platelet morphologywere unremarkable. Reticulocyte count was 1%.
1Senior Registrar in Clinical Haematology, University
Serum bilirubin levels were normal. Coagulation
Medical Unit, Faculty of Medicine, Sri Jayawardena-
tests: Bleeding time – 3 minutes (Control 0-6min),
pura, 2Consultant Haematologist, 3Consultant
PT 27.5s (control 11.0s), aPTT 81.7s (control 26.0s),
Paediatrician, Lady Ridgeway Hospital, Colombo,
thrombin time (TT) 18.2s (control 15.6s). Fibrinogen
Sri Lanka.
level (antigen) 3.3 g/L (normal range 1.5- 4.0/L) and
The Sri Lanka Journal of Haematology
ONKD Gamage et al. SLJH. 2015; 7(1): 29-31
fibrinogen activity by Clauss method 372 g/L
lation inhibitor. The presence of a time dependent
(normal range 150- 400g/L). Correction studies with
inhibitor was excluded by the 2 hour incubation
pooled normal fresh plasma (PNP) (50:50 mix): PT
test. Both strongly positive dRVVT and KCT tests
was corrected, and the aPTT remained prolonged
indicated the presence of LA. Positive ANA, ds-DNA
without correction. The inhibitor screening:
and DAT indicated the presence of an autoimmune
negative (difference of aPTT following 50:50 mix
disease. Although the clinical criteria were not
with PNP at and after 2 hours incubation was < 6
fulfilled for SLE and factor II assay and prothrombin
sec). Lupus anticoagulant (LA) screening: dRVVT- LA
antibody level was not performed due to the
ratio 2.3 (normal < 1.2) and KCT test >5 min, control
unavailability of the facilities to test; based on the
82s. Liver function tests and renal function tests were
test results diagnosis of the rare lupus anti-
normal. Urine analysis normal with no red cell casts.
coagulant – acquired hypoprothrombinemia
Direct antiglobulin test (DAT) was positive with C3d
syndrome (LA-HPS) was made. Repeating of the
specificity. Anti-nuclear antibody (ANA) was posi-
ANA, ds-DNA and the dRVVT test was planned to
tive with a titre > 1/80 by direct immunofluorescence
confirm persistent positivity after 12 weeks.
method. The ds-DNA antibody was positive byenzyme linked immunosorbent assay method.
The patient was treated with oral prednisolone1mg/kg/day and the coagulation test results
Prolongation of aPTT without being corrected
reverted to normal within 2 weeks of treatment
following PNP mix indicated presence of a coagu-
Table 1. Coagulation test results from the date of admission
Days Vs Tests
50:50 mix with PNP
50:50 mix with PNP
Inhibitor screening
(aPTT 50:50 mix with PNP)Fresh Mix (At)
Incubated mix (Affter 2hrs)
LA1(Screening test)
LA2 (Confirmation test)
2.3 (1.2) (Stronglypositive)
*50:50 correction = mixture of patient's plasma and pooled normal fresh plasma (PNP)at a ratio of 1:1, PT - prothrombintime, aPTT - activated partial thromboplastin time test, TT - thrombin time, dRVVT = dilute Russell viper venom time,KCT = kaolin clotting time, LA 1 = lupus anticoagulant screening reagent 1, LA 2 = lupus anticoagulant screening reagent 2,S = seconds, Min = minutes
The Sri Lanka Journal of Haematology
ONKD Gamage et al. SLJH. 2015; 7(1): 29-31
Patient was followed up at the paediatric clinic and
patient LA-HPS was the first and the most impor-
the haematology clinic regularly with the assess-
tant clinical sign of the onset of the systemic illness.
ment of clinical parameters and the relevant hae-
Our patient's LA-HPS was successfully treated with
steroids, confirming that this treatment representsthe leading therapy for this coagulopathy.
Lupus anticoagulant is the coagulation based
demonstration of antiphospholipid antibodies by
Contribution: All authors contributed equally.
phospholipid dependent coagulation tests dRVVT
Conflict-of-interest disclosure: The authors declare
and KCT. Hypoprothrombinaemia results in pro-
no conflict of interest.
longation of both PT and aPTT with normal TT andcorrected by mixture of patient's plasma and
Correspondence: Dr. Gamage ONKD, Senior Registrar
normal plasma at a ratio of 50:50 which can be
Clinical Haematology, University Haematology Unit,
confirmed by the factor II level assay.3-6
Colombo South Teaching Hospital, Kalubowila, SriLanka.
The LA-HPS is a rare acquired disorder associated
with haemorrhagic manifestations. It appearsmostly in young females, even in infants. It
presents as a complication of SLE or transient viralinfections.2,3
1. Mackie I, Moore GW, Greer IA, Greaves M. British
Committee for Standards in Haematology. Guidelines
The LA-HPS is characterised by a very strong LA and
on the investigation and management of antiphos-
pholipid syndrome. Br J Haematol. 2012 Apr; 157(1):
presence of polyspecific antibodies. They bind to
the epitopes of the anionic phospholipids and of
Epub2012 Feb 8.
prothrombin, but they do not neutralise pro-thrombin. Therefore, a FII activity deficiency is not
2. Sarker T, Roy S, Hollon W, Rajpurkar M. Lupus anti-
coagulant acquired hypoprothrombinemia syndrome
due to an inhibitor, as suspected, but to an evident
in childhood: two distinct patterns and review of the
factor decrease owing to the higher clearance of the
literature. Haemophilia. 2015 Nov; 21(6): 754-60.
prothrombin-antibody complex in the reticuloen-dothelial system.3,4
3. Vivaldi P, Rossetti G, Galli M, Finazzi G. Severe
bleeding due to acquired hypoprothrombinemia-lupus anticoagulant syndrome. Case report and
Corticosteroid therapy is the treatment of choice
review of literature. Haematologica Haematologica.
for LA-HPS associated with SLE; it normalizes the
1997 May-Jun; 82(3): 345-7.
PT time.2-4 In cases associated with a viral infection,
4. W Collins P, Chalmers E, Hart D, Jennings I, Liesner R,
LA-HPS reverses spontaneously with the resolution
Rangarajan S, et al. United Kingdom Haemophilia
of the infection. Therefore, steroid therapy is not
Centre Doctors' Organization. Diagnosis and manage-
necessary.2-4 Given the complex coagulopathy of
ment of acquired coagulation inhibitors: a guideline
our patient, caused by an acquired inhibitor, and
from UKHCDO. Br J Haematol. 2013 Sep; 162 (6):
the risk of serious major haemorrhage, we com-
758-73. doi: 10.1111/bjh.12463. Epub 2013 Jul 25.
menced steroid therapy and was able to obtain
5. Ghirardello A, Doria A, Ruffatti A, Rigoli AM, Vesco P,
complete normalisation of PT and APTT after of
Calligaro A, et al. Antiphospholipid antibodies (aPL)
two weeks of treatment.
in systemic lupus erythematosus. Are they speci-fictools for the diagnosis of aPL syndrome? Ann
Finally, we conclude that, LA not only produces
Rheum Dis. 1994 Feb; 53(2): 140-2.
APTT prolongation, but may also produce a more
6. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey
complex coagulopathy with PT prolongation-LA-
RL, Cervera R, et al. International consensus state-
HPS type. LA-HPS onset could be haemorrhage
ment on an update of the classification criteria for
related with an added FII deficiency and marked
definite antiphospholipid syndrome (APS). J Thromb
inhibitor effects of APTT dependent factors. In our
Haemost. 2006 Feb; 4(2): 295-306.
The Sri Lanka Journal of Haematology
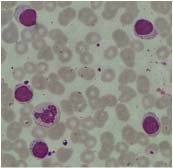
MN Dilhani et al.
SLJH. 2015; 7
2015, 7: 32
Images in Haematology
A case of Large Granular Lymphocytosis
MN Dilhani1, S Suresh2, J Thennakoon3
Figure 1. Peripheral blood smear (Leishman stain, ×100) – a monomorphic population of moderate to large
lymphocytes with abundant pale cytoplasm containing many azurophilic granules, eccentric nuclei with
condensed chromatin.
A 65-year-old previously well female without
with T cell large granular lymphocytic leukemia
lymphadenopathy or organomegaly had peripheral
blood lymphocytosis of 11.6x109/L. Total whitecell, neutrophil and platelet counts were 14.9x109/
LGL proliferations are either nonclonal in aetiology
L, 2.9x109/L,250x106/L respectively. Haemoglobin
(viral infections, auto immune conditions, post
level was 11.4g/dL. Lymphocyte morphology re-
splenectomy, bone marrow or solid organ trans-
sembled large granular lymphocytes (LGL) (Figure
plantation) or clonal (aggressive T-LGL leukaemia
1). Marrow aspirate showed 70% cells with LGL mor-
and chronic or aggressive NK cell leukaemia).
phology, and immunophenotype was CD3+(89%),
Clinical presentation and immunophenotype help
CD8+( 84%), CD4+ (80%), CD57+(80%), CD2+(94%),
to determine the diagnosis.
CD5+(88%), CD56-, CD7-TCRβ+(89%) and TCRγδ-.
Marrow biopsy had a 30% interstitial infiltrate
of lymphocytes being CD 3+, CD5 +, CD 57+ and
1. Swerdlow SH, Campo E, Jaffe ES, Pileri S, Stein H, Thiele
scattered positive for CD20/CD8.
J, Vardiman J. (2008) WHO Classification of Tumoursof Haemopoietic and Lymphoid Tissues, 4th edn.
Cellular morphology favored T or Natural Killer (NK)
International Agency for Research on Cancer Press,
cell disorder. Immunophenotype was compatible
Lyon, France.
1Registrar in Haematology, Department of Pathology, Haematology Unit, Faculty of Medicine Ragama,2,3Consultant Haematologist, Department of Haematology, National Cancer Institute Maharagama,Sri Lanka.
The Sri Lanka Journal of Haematology
Answers for the CME: Acute trauma coagulopathy and massive transfusion
like in DIC but DIC can occur secondarily in ATC.
Coagulopathy of trauma is a distinct entity with
When ATC becomes exacerbated by hypo-
a strong impact on the outcome. Physiological
thermia, acidosis and haemodilution (due to
haemostasis controls blood fluidity and rapidly
the rapid infusion of colloids) it is called IC.
induces haemostatic plug formation in order
This then becomes a vicious cycle, enhancing
to stop bleeding. Primary haemostasis (vascular
more protein C activation and damage to
and platelet mechanism), coagulation and
fibrinolysis are closely linked to each other andprecisely regulated in order to efficiently close
It has been shown that early recognition of
vessel wounds, promote vascular healing and
acute trauma coagulopathy, accompanied by
maintain vessel patency.
appropriate and aggressive management, cancorrect coagulopathy, control bleeding, reduce
There is limited understanding of the mecha-
blood product use and improve outcome in
nisms by which tissue trauma, shock and inflam-
severely injured patients.
mation initiate trauma coagulopathy. Acutecoagulopathy of trauma-shock should be
considered as a distinct entity from disseminated
Massive transfusion is associated with numerous
intravascular coagulation (DIC) as described inother conditions. Rapid diagnosis and directed
and significant complications. In massive
interventions are important in prevention.
transfusion, coagulopathy is frequently seendue to dilution of clotting factors and dilutional
Coagulopathy of trauma is a haemostatic and
thrombocytopenia. This is exacerbated by the
haemodynamic depletion which is now recog-
consumptive coagulopathy triggered by massive
nized as acute trauma coagulopathy (ATC) and
haemorrhage in trauma.
iatrogenic coagulopathy (IC).
Multiple factors contribute to hypothermia in
Acute trauma coagulopathy has recently been
trauma patients. Rapid transfusion of packed
recognized as a multifactorial primary condition.
red cells stored at 4°C will lower the recipient's
The principle drivers of ATC are tissue trauma,
core temperature. Hypothermia leads to de-
inflammation, hypo-perfusion/shock and acute
creased production of clotting factors, platelet
activation of the neurohumoral system. The
dysfunction, impaired haemostasis and de-
principle mechanisms of early ATC are (i) acti-
creased citrate metabolism (citrate toxicity).
vation of the protein C pathway (ii) endothelialinjury (iii) hyperfibrinolysis (iv) platelet dys-
Hypocalcaemia occurs due to citrate in additive
function. Activation of the protein C pathway
solution in packed red blood cells (PRBC), fresh
and endothelial damage initiates the coagu-
frozen plasma and platelets, especially in the
lation system which ultimately leads to primary
presence of hypothermia.
hyperfibrinolysis in ATC.
Potassium concentration increases in stored
Endothelial injury may also be linked to
PRBC, due to membrane Na+-K+ ATPase pump
‘autoheparinisation' as the entire endothelial
inactivation. Therefore, transient hyperkalemia
glycocalyx contains approximately 1 liter of non
is common with rapid transfusions. Hypo-
circulating plasma with significant amount of
kalemia has been noted with massive trans-
‘heparin like substances'. When degranulated
fusion due to restoration of membrane ATPase
this automatically leads to autoheparinisation.
pump thus allowing potassium to re-enter the
Therefore, initially the pathophysiology is not
The Sri Lanka Journal of Haematology
Citrate undergoes hepatic metabolism to
and treatment of coagulopathy in massive hemor-
bicarbonate and during a massive transfusion
rhage and hemodilution. Anesthesiology. 2010 Nov;
a metabolic alkalosis may occur.
3. Sihler KC, Napolitano LM. Complications of massive
transfusion. Chest. 2010 Jan; 137(1): 209-20. doi:
1. Maegele M. The coagulopathy of trauma. Eur J Trauma
Emerg Surg. 2014 Apr; 40(2): 113-26. doi: 10.1007/
4. Maxwell MJ, Wilson MJA. Complications of blood
s00068-014-0389-4. Epub 2014 Mar 18.
transfusion. Contin Educ Anaesth Crit Care Pain. 2006;
2. Bolliger D, Görlinger K, Tanaka KA. Pathophysiology
6(6) 225-9. doi: 10.1093/bjaceaccp/mkl053.
The Sri Lanka Journal of Haematology
The Sri Lanka Journal of Haematology is the official publication of the Sri Lanka College of Haematologists.
All views expressed in the Journal are those of the individual authors/contributors and the publisherdoes not take any responsibility for the views expressed or the material submitted by the authors/contributors.
Information and copies could be obtained from the Editors, Sri Lanka College of Haematology, No. 06,Wijerama Mawatha, Colombo 07.
The Journal will publish original articles, perspectives, case reports and images in haematology. Lettersto the Editor are also welcome. Review articles and leading articles will be solicited by the Editors.
Author Guidelines are available in the College website http://www.slchaem.lk/.
Publications by the Sri Lanka College of Haematologists:
Thalassaemia – M. Nanada Prematileke
Anticoagulation with unfractionated heparin – Arundathi P. Kurukulasuriya
Warfarin – Mala Tudawe
Guidelines for the treatment of bleeding in haemophilia – Sudharma Vidyatilake
What you should know about haemophilia (in Sri Lanka) – Sudharma Vidyatilake
What you should know about ITP (in Sri Lanka) – Sudharma Vidyatilake
What you should know about ITP (in Sri Lanka) (English, Sinhala and Tamil translations)
– Dammika Gunawardena
Source: http://www.slchaem.lk/wp-content/uploads/2016/05/Journal-of-Haematologist-2015.pdf
ERT Conditions for Productive Learning in Networked Learning Environments: Leadership Report Main author: Lone Dirckinck-Holmfeld (UAalborg) Nature of the milestone: Report Dissemination level: Public Planned delivery date: November 2007 No part of this document may be distributed outside the consortium / EC without
The African Review of Physics (2013) 8:0062 463 Linear and Non Linear Optical Effects of Pyrimethamine and Sulfadoxine: Ab-initio and Density Functional Study Geh Wilson Ejuh1, 2,* and Ndjaka Jean Marie1 1University of Dschang, IUT Bandjoun, Department of General and Scientific Studies, Bandjoun, Cameroon 2Université de Yaoundé I, Faculté des Sciences, Département de Physique, Yaounde, Cameroun