Splcenter.org
Prisoner Diabetes Handbook
A Guide to Managing Diabetes—
for Prisoners, by Prisoners
published by the southern poverty law center
Why A Handbook for Prisoners With Diabetes?
Diabetes is important.
It is common, chronic, and can cause disabling complications.
What you do for yourself to take care of your diabetes is the most
important factor in your diabetes being well controlled. Very little diabetes education is provided in prisons. There are few organized programs for prisoners with diabetes.
Experience has shown that others with diabetes are a good source
of information about the disease. By cooperating and sharing,
diabetics can help each other.
A diabetes support group has been meeting at Great Meadow
Correctional Facility in Comstock, New York since 1997. This
group helps prisoners with diabetes to improve their diabetes
management. People in the
group learn from the experi- Diabetics at Comstock Prison would
ences of other prisoners with be lost without the support group to
diabetes. There is a lot of sup-
port and good fellowship in help them learn about diabetes.
the diabetes group.
Sometimes the group chooses
a project to do together. In the fall of 2003 we decided to write
a handbook to share what we learned about diabetes self care
in prison.
This handbook is by prisoners, for prisoners.
Our goal is to help you manage your diabetes better yourself.

Type 2 Diabetes
FACTS ABOUT DIABETES
The pancreas makes too little insulin and the insulin doesn't
Diabetes is not just one disease but several different diseases that
all cause the same basic problem: too much sugar in the blood.
Type 2 is usually treated with diet and exercise early in the dis-
ease. As time goes on, medicines must be added (usually pills)
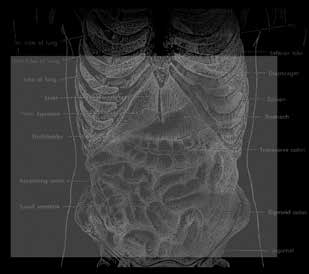
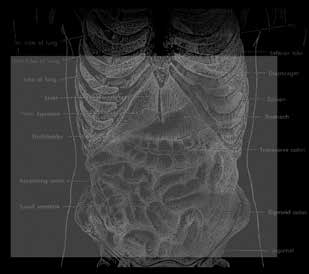
Biology of Diabetes
and eventually most people with type 2 diabetes will also need
The sugar in the blood is called glucose.
insulin. (Although some people with type 2 diabetes may need
All cells in the body use glucose to make energy to live.
insulin soon after diagnosis.)
All sugars and starches we eat are made into glucose.
People are usually middle aged when type 2 starts, but it can
begin in adolescence.
Glucose moves around the body in the blood to get to the cells
where it is used.
Often many people in the same family have type 2 diabetes.
Insulin is a hormone that helps move glucose out of the blood into
Type 2 diabetes often occurs in people who are overweight and
the cells. Insulin is made in the pancreas, an organ located behind
losing even 10-20 pounds will really improve the diabetes. Get-
and below the stomach.
ting weight down to normal (especially early in the disease) may
The more you know about diabetes,
even cure type 2 diabetes for awhile.
Different types of diabetes re-
the more you can help yourself
sult from different problems in
More women than men have type 2 diabetes.
insulin production and insulin
Type 2 is more common among Blacks, Native Americans and
Herb effectiveness:
• Type 1: the body makes no insulin at all
Nine out of ten people with diabetes have
• Type 2: the body makes too little insulin, and the insulin doesn't
type 2 diabetes.
Many people don't know they have type
• Gestational Diabetes: diabetes during pregnancy
2 diabetes, because they don't feel sick
and haven't had a blood sugar test.
Type 1 Diabetes
Someone with type 1 diabetes must always take insulin because
his/her pancreas makes no insulin at all.
This type of diabetes occurs during preg-
nancy in a woman who did not have dia-
People are usually young when they get type 1 diabetes, often
betes before.
under 20 years of age, but it can begin at any age.
In gestational diabetes, the pancreas
One out of ten people with diabetes has type 1 diabetes.
makes insulin normally but the insu-
There is no cure for type 1 at this time.
lin does not work well in the pregnant
woman's body.
Gestational diabetes usually goes away when the baby is born,
Find Out If You Have Diabetes
but it means that the woman is more likely to get type 2 diabetes
Many people who have type 2 diabetes don't know they have it.
They don't feel sick and may never have had a blood sugar test.
Which type of diabetes do you have? If you're not sure, ask
Know who is at risk for diabetes.
the doctor.
If you are at risk, get a blood sugar test.
Diabetes Causes Medical Complications
Tell others so they can get tested too.
Over years, the high blood sugar of poorly managed diabetes
damages the body in many ways.
Who are at greatest risk? People with one or more of these
There can be damage to eyes, kidneys, nerves and arteries causing
risk factors are more likely to get type 2 diabetes:
blindness, kidney failure, foot infections, heart attack, stroke, leg
• Other family members who have diabetes
cramps, pneumonia, gum disease and other complications.
I didn't even know my
Importance of Blood Sugar Control
• Get little or no exercise
sister and aunt had
Keeping blood sugar at near normal levels helps prevent the
• Black, Hispanic, Native American, or Asian/
long-term complications like blindness, kidney failure, foot am-
diabetes. It was a
Pacific Island ethnicity
putations, heart attacks and strokes.
hush-hush thing that
You cannot tell how good your blood sugar control is just by
was unheard of to talk
how you feel.
about. They only told me
Feeling good and not peeing a lot is not good enough control to
But anyone can get diabetes, even if they have
prevent the long-term complications of diabetes. And if your
none of these risk factors
when I started to talk
blood sugar is often high, you may get used to high blood sugars
about my new diagnosis.
and feel fine, even though the sugar is hurting your body.
Symptoms of undiagnosed diabetes:
There may be no symptoms at all. You may
You must get two kinds of blood tests to know how well your
not suspect anything is wrong.
management is working:
Or you may have one or more of the following symptoms:
1. Blood sugar tested before a meal is a measure of daily control
and should be between 80 and 130 most of the time.
• Urinating a lot, especially after eating sweets or a big meal.
2. The A-1-C test is a measure of control over the last 3 months
• Being very thirsty.
and should be under 7.0%
• Having blurry vision from time to time
What is your A-1-C? If you're not sure, ask the doctor.
• Feeling tired and not having much energy.
• Losing weight without trying.
• Having numb or tingling feet.

Survival in prison requires self-control
A fasting blood sugar test is used to diagnose diabetes.
Some prisoners survive well in prison by living a highly dis-
ciplined life. People with diabetes need to be disciplined too
When was your last blood sugar test? What was the result? Were
and manage their blood sugar with knowledge, self-control and
you fasting (nothing to eat or drink for at least 8 hours) when
the blood was drawn?
A person who has diabetes needs Prison will make you or break
A fasting blood sugar of 126 or higher indicates someone who
to be disciplined in order to be able
probably has diabetes.
you. There are people who can
to follow consistent daily routines.
A fasting blood sugar between 100 and 125 indicates someone
This is truer in prison than out- and people who can't. We are
who may be developing diabetes. A fasting blood sugar under
side, since choices in prison are here in the diabetes group be-
cause we are the people who
If the fasting blood sugar is 100 or higher, it should be repeated.
Healthy eating, especially in pris-
on, requires self-control.
can, who have taken charge of
Help Others Get Diagnosed
Self-control is a necessity that our fate.
Tell people at risk to get their blood sugar tested.
people who manage diabetes suc-
cessfully get comfortable with.
Tell people about the symptoms.
The importance of regular daily routines
Get Serious About Your Diabetes
You need a daily schedule because following a
daily routine is one way people live well with di-
Prison challenges your determination to survive
abetes and achieve good blood sugar control.
So does diabetes.
Regular meal times and regular physical activity
help control blood sugars.
Diabetes can destroy your health slowly while you do your time.
But ignoring diabetes is dangerous. So get diagnosed, learn to
Daily routines in prison are well established
control your blood sugar, and stay healthy.
and consistent so the rigid structure of the cor-
rectional day can support your efforts to follow
a regular daily activity plan.
Diabetes is with you all day every day.
Losing my feet is my greatest fear. I want to
Find the right balance for you.
beat the system and walk out of here on my
own two feet.
Get serious about blood sugar control
Remember, good blood sugar control prevents complications of
diabetes such as blindness, amputations, kidney failure, heart
attacks and strokes.
Stress, Loneliness and Frustration Can Sabotage
Get Right with Yourself
Your Determination
Stress and frustration can cause you to lose focus and your
How you feel affects your diabetes plus how you feel influences
what you are able to do for yourself.
Hopelessness affects your will power and discipline.
You need mental strength to manage diabetes in prison day after
You may go back to old eating habits, stop testing, skip medicine,
or miss healthcare appointments.
Prison is a highly stressful environment
Responding to the stress
You need a mellow frame of
In prison, it's hard to relax and hard to feel safe, even locked in
Recognize anger and feelings.
mind to handle what we have
Find ways to relax.
to deal with here all the time.
Stress affects everything about daily life in prison.
Exercise and music help the body and Overcome it mentally. Create
Stress affects your diabetes control physically and emotionally.
mind to relax.
the state of mind. Make it
Change conditions to reduce stress;
find where there is less noise and positive.
You're never alone, yet always being with strangers is often
fewer threats.
Quiet is better. You need a chance to
You're disconnected from family, friends, and home.
get into yourself to relax.
When the letter you are waiting for doesn't come, when packages
One person in our diabetes group learned meditation from a
and visits stop, you can feel alone and hopeless.
Buddhist volunteer in another prison.
Frustration
Sometimes people get frustrated and upset about diabetes or
What You Can Do To
frustrated with other people's responses.
Manage Your Diabetes
It is frustrating when sugar stays high even though you have
Diabetes needs your attention every day.
tried to improve it.
Successful management is finding the right balance of diet, ac-
And frustrating when people invade your privacy by saying "You
tivity and medicine to control blood sugar and keep your A-1-C
shouldn't eat that."
It is frustrating to feel like a freak and be ashamed and fed up
Getting there is a process. It takes time, effort, and monitoring
with the needles.
so you can see how you are doing.
Diabetes management includes:
They can give you advice about diabetes and can adjust your
medicines to improve control.
• Education: Learn about taking care of diabetes
They can give you access to things you need like blood sugar
• Eating healthy foods: Choose meals that help control blood
tests, the medical diet, and specialist referrals. But you have to
sugar and blood fats
convince them to work with you so you can get what you need.
• Being Active: Use regular exercise to help manage blood sugar
You may have to show them that you are seri-
• Taking Medicine: Shots or pills replace what is missing from
ous about your diabetes.
Diabetes management is harder in prison
• Monitoring: Test your blood sugar and notice how you feel
There is only limited variety and quality of
• Health care: Get support from doctors and nurses; get lab
foods available in prison and access to blood
sugar testing is limited.
Management is often things you do for yourself
There is also limited availability of impor-
tant services like diabetes education, medical
• Education: You educate yourself by seeking out information
nutrition therapy, podiatric care, and dental
• Food: You choose what you eat even though your choices are
Insulin is rarely given more than twice a day
• Activity: You choose what you do and how hard and frequently
and the timing may not be the best. Plus some medicines and
you do it much of the time
devices, such as insulin pumps, are not available.
• Medicine: Doctors prescribe medicine, but
You can't "shop" for professionals you trust. Furthermore, it's
you choose to take it
hard to get to the specialty appointments you need or hard to do
what you have to in order to get to those appointments.
• Monitoring: You monitor yourself the best
you can; you go to medical to get blood sugar
Set your own diabetes management goals
You need to set your own diabetes goals and work to achieve
• Health care: You have to know and advocate
for the services you need; you request blood
sugar, A-1-C, other monitoring tests and spe-
You can't get the A-1-C from 13% to under 7% instantly. It takes
cialty appointments from the doctor
time and effort.
You need realistic short and long-term goals:
Nurses and doctors can help with your
diabetes management
Short-term goals for today
Nurses and doctors who care can help you to
Medium-term goals for the next three months
improve your diabetes management.
Long-term goals for life

For example:
Family: Talk to your family about your diabetes. Your mother
and your sister may know a lot about diabetes.
Goals for today might be: avoid candy; eat more fruit.
Others with diabetes: Talk to others who have diabetes when
Goals for the next 3 months might be: lower your A-1-C from 13
you are in clinic together to get insulin
shots or at meals together.
Goals for life might be: no amputation, no kidney failure, no
The more you know about the
Professionals: Ask nurses or doctors
disease, the more you can
about diabetes. Find out who has a
Begin with what is most important to you, today, right now.
special interest in helping people with help yourself.
Improve your diabetes management starting there.
Read: Find pamphlets, books, and
Attitude of staff and friends makes a difference
magazines to read about diabetes. Look in the prison library for
If someone says, "You're dumb and you're doing it all wrong,"
health books.
that doesn't help you at all.
Write: Diabetes organizations will send you information if you
But when someone says, "Let me
write to them and ask for publications.
tell you how I do it so you can do
Starting today I can think
it better," that supports your own
Good reading material
more about what I eat to try best efforts.
Diabetes Forecast: published by the
to get my A-1-C test below 11.
American Diabetes Association, PO
Success helps too. When you see
Box 363, Mount Morris, IL 61054-8303.
the positive results that your self-
James discipline can achieve, it gives you
Diabetes Health: published by King's
strength to go on.
Publishing, PO Box 15368, N. Holly-
wood, CA 91615-5368.
Lower blood sugar tests, lower A-1-C, fewer low blood sugar
episodes, or weight loss are good measures of success.
Centers for Disease Control and Pre-
vention, Take Charge of Your Diabetes,
3rd edition, Atlanta: U.S. Department
of Health and Human Services, 2002.
(FREE). This and other materials are
Ignorance creates anxiety.
available by calling 1-800-232-4636, option 4.
Learning what to do creates confidence.
Education helps overcome fear.
People with diabetes can educate each other.
Knowledge helps you establish control.
In a support group, people with diabetes share their experience
How does a prisoner learn about diabetes?
and knowledge.
Seek information wherever you can find it:
Ask the health staff at your prison to sponsor a diabetes support
BUT, many people with diabetes find it is easier to reach their
Food and Nutrition
blood sugar goals when they stop drinking regular soda and large
amounts of fruit juice and stop eating candy and other foods that
Freedom to choose your own food
are almost entirely sugar.
Choosing what to eat may be one of the last freedoms a prisoner
There are medical nutrition goals based on each person's needs,
has left. The restrictions of a medical diet can be hard for people
such as carbohydrate controlled meals, reduced fat and choles-
who are locked up.
terol, reduced salt, high fiber, or weight loss.
A prisoner with diabetes may resist letting diabetes take away
You should think about what you eat, and choose foods that
his last freedom. But having diabetes doesn't mean you can't
support your goals.
have your favorite foods. Knowledge about food and nutrition will help you to choose
Why low saturated fat and low cholesterol diets?
Animal fat is mostly saturated fat and cholesterol therefore eat
Be strictly disciplined if you want, or be self indulgent in an
less animal fat because a diet with less saturated fat and less
intelligent way if that is what you want.
cholesterol is healthier.
A low saturated fat diet helps prevent heart attacks.
Diet Goals
A low saturated fat diet helps prevent strokes.
The American Diabetes Association recommends:
A low fat diet has fewer calories to prevent weight gain.
• Foods containing carbohydrate from whole grains, fruits, vege-
tables, and low-fat milk should be included in a healthy diet.
How do I eat a low saturated fat, low cholesterol diet?
• Eat less fat, especially animal fat, to reduce the risk of heart
Eat fewer fatty foods like sausages, bacon, cheeseburgers and
attack and stroke.
• Eat less salt and sodium to help control blood pressure.
Eat leaner meats like skinless chicken or turkey breast and fish,
• Eat fewer total calories for weight loss if you are overweight.
if available.
Eat less high cholesterol foods like egg
There Is No "Diabetic Diet"
yolks and liver.
You can eat whatever you
There is no "diabetic diet" and there are no "forbidden" foods.
Cream is an animal fat that contributes want. You just can't eat as
If you are on medicines that lower blood sugar (like insulin and
to heart disease and stroke.
sulfonylureas), you should eat consistent amounts of starch and
much as you want, whenever
Because 1% milk or skim milk has less
sugar (carbohydrate) at each meal or snack.
cream, it is better for you.
If you control your diabetes with exercise and diet, or if you are
Also, eat lower fat cheeses like part
on medicines that don't lower the blood sugar, avoid eating a
skim milk mozzarella, if available.
large amount of carbohydrate at one time. In other words, spread
your carbohydrates throughout the day.
Why a low salt diet?
If weight loss is your goal, eat smaller portions.
Salt is made of sodium chloride and contributes to high blood
Learn how to salvage an adequate diet from what they feed you,
by choosing well and trading with others, if allowed, for more
of what you need.
For a lower salt diet use little or no salt from the salt shaker on the
table. Always rinse canned vegetables to remove some of the salt
Adjust when you eat to prevent low blood sugar
used in canning. Also limit salty snacks like chips and salted nuts.
And, if you drink tomato or V8 juice, get the low salt kind.
If possible, spread food out throughout the day in meals and
Commissary: If you buy snacks from the "store":
If you take medicine for diabetes, don't miss a meal or planned
Read the nutrition labels on packaged foods purchased from the
commissary. Labels tell you how much carbohydrate, saturated
Eat enough carbohydrates to prevent low blood sugar when
fat, cholesterol and salt are in each packaged food item.
insulin is most active.
Many prisoners like to eat the whole package all at once. But,
It is important to know that there are different kinds of insulin
usually there are 2 or 3 "servings" per package.
used in shots and they work at different times during the day:
Figure out how much carbohydrate or saturated fat is in the
Morning REGULAR insulin acts after breakfast and lasts through
One fruit pie has almost 500 calories. A whole fruit pie is not a
Morning NPH insulin acts after lunch and lasts through dinner.
good choice for a snack at night because it has too many carbo-
Evening REGULAR insulin acts after dinner and lasts until late
evening. Evening NPH acts around midnight and lasts through-
But an athlete who has diabetes might need a large snack like a
out the night.
whole fruit pie before and during an extremely strenuous work-
out to prevent his blood sugar from dropping too low.
People who take insulin for diabetes may need 1 or 2 snacks to
prevent low blood sugar. These snacks should be at the times
when their insulin works the hardest, or just before they have
How To Improve Your Diet
been having the low blood sugar reactions.
Low blood sugars in the middle of the night? Try a snack around
What to eat?
Choose healthy foods with less sugar, less fat, less salt, and more
Blood sugar too high at 4PM? Eat less starch at lunch or skip
that afternoon snack.
Eat fruit and vegetables, especially raw vegetables, whenever
they are available.
Adjust diet to anticipated activity:
Try to be consistent about the amount of starch or sweet foods
Muscles use blood sugar for energy during exercise.
(carbohydrate) that you eat each day and at each meal or

So, before a major workout plan to eat a larger lunch with enough
Don't reject all foods with dressings
carbohydrate to prevent low blood sugar when exercising.
At first people in the diabetes group said,
Eat snacks with some carbohydrate during and after exercise.
"The cole slaw is rotten and they're cover-
ing it up with that thick dressing." But it is
However, during times of inactivity, such as watching a movie,
one of the few sources of raw vegetables
if you plan to eat candy, then eat a smaller meal.
which is on the menu frequently. One man
tried it and reported back that it was ok.
Choose What You Eat
Many of them now eat coleslaw as often
Most prisoners have little choice at mealtime. But, even if you
as they can.
get one tray, you can choose what to eat off the tray.
Don't get bored with the same fresh fruit
Know what is in the food you eat. Use nutrition labels, common
all the time:
sense, or read books about food and nutrition to learn more.
One man in the diabetes group said, "They
Remember to eat fewer sweets and fats and eat to satisfaction,
apple you to death here."
but don't overeat.
But apples are the only fresh fruit that is
Increase fiber by eating more fresh
regularly available on the menu.
or raw fruits and vegetables, whole
I cheat; I eat less bread when grains, beans, bran and oatmeal,
Make the most of it in spite of the monotony.
I want to eat some cake.
when available.
Trade with others, if allowed, to improve your diet:
Try to substitute foods. For example,
Trade away high carbohydrate or high fat items in exchange
if you want syrup on that pancake?
for fruit, vegetables (especially raw vegetables) and high fiber
Use sugar free diet syrup. Or can't
(But it's not "cheating"; it's
get any diet syrup? Ok then, use a
little sugar syrup, but eat fewer pan-
Examples of high fiber foods available in some prison menus
Want a small piece of cake for dessert? It's ok. Eat less starch
General diet: apples, cole slaw, three-bean salad, oatmeal,
(potato, bread, pasta, rice) with the meal to compensate for the
sugar in the dessert.
Medical diet: raw carrots, raw celery, prunes, non-white breads
Don't reject foods that are mixtures
Commissary: canned beans, canned vegetables, instant oatmeal,
At first people in the diabetes group said, "3 bean salad is garbage
all mixed up to hide what's in it." But it provides vegetables and
fiber that you need in your diet. The recipe calls for 3 different
What About Snacks?
beans to be mixed up together. Most of the men were unfamiliar
People who take insulin may need a snack (especially before bed)
with this type of salad, so they thought it was all leftovers. Now
to prevent low blood sugar. But not everyone who has diabetes
many of them eat 3 bean salad to improve their diet.
needs to have snacks.
If you are trying to lose weight, snacks may help or hurt your
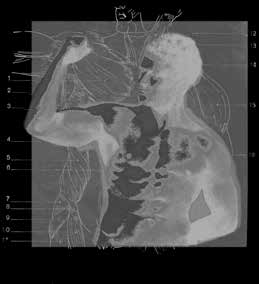
Learn ways to work out in your cell.
ability to lose weight.
David's Exercises to Do In Your Cell
If it is allowed, you may need to stockpile food for evening and
1. Push-ups on the floor.
nighttime snacks. In some places, limited amounts of food may
be carried out of the mess hall: one apple; 4 slices of bread. If you
2. Sit-ups: Wrap a belt around the end
are able to, collect fruit when you can (apples; unripe bananas)
of the bed loosely, lock feet through
and eat them as snacks over several days. But you can get a ticket
the belt to hold legs down, then do
for a rule violation if you take too much food out of the mess hall
for snacks later.
3. Pull-ups: Use a towel to pull your-
self up on the bars; or stand your bed
Exercise and Activity
straight up and pull yourself up.
4. Crunches can be done on the bed
Benefits of exercise
or on the floor.
• Healthy heart
5. Dips can be done by standing be-
• Healthy blood pressure
tween the locker and the bed post,
support your weight on your hands
• Relax the body and mind
on the locker and bedpost, bend legs I eat a larger lunch to get
• Control your weight
at the knee to move lower legs out of
the way behind you, then do dips up my sugar a little high when
• Better blood sugar control
and down with arms.
I'm planning a big afternoon
Issues related to exercise
6. Do "dead weights" by using water workout. Then I eat a snickers
filled buckets as weights, lifting in uni-
Don't overdo it.
son with both arms.
bar during the workout, and
Choose an exercise program that is comfortable for you
7. Walk in place.
sometimes another one right
Be alert to the risk of low blood sugar during, shortly after, and
8. Do stretches by placing feet on after I finish.
hours after a strenuous workout. Plan ahead how you will pre-
vent low blood sugar during and after exercise. Eat more before
and/or while exercising and have some sugar with you.
9. Calf exercises: Stand in place while
holding onto bars, move whole body
On the other hand, if your blood sugar is too high, exercise can
up and down by standing up on your
bring it down to a better level. You can use exercise to correct
(This works for Paulie because
toes. Can be done standing with toes
high blood sugar.
on books, so that the ankle tendons are he has type 1 diabetes, is not
The yard can be dangerous, so exercise where you feel safe.
stretched when the heel goes down overweight, and works out
to the floor while the toes stay up on
Because access to the gym is limited, take advantage of a gym
strenuously for a long time.)
Mix up the exercises to work 10. Lunges: step forward and bend
and Nateglinide (Starlix). Possible side effects are low blood
on different muscle groups at knee; repeat on opposite side.
sugar and weight gain.
different times. Don't let it 11. "Cherry picking": legs about 2 feet
• Medicine (biguanides) that slows down the amount of sugar
apart; arms reach up high, then down
made by the liver called Metformin (Glucophage, Riomet, Glu-
to shoulder level, then bend down to
cophage XR, Fortamet, Glumetza). Possible side effects include
touch the toes, repeat.
diarrhea, nausea, upset stomach, metallic taste in the mouth,
and weight loss.
• Medicines that help your body use its own insulin better. These
Medicines
medicines (thiazolidinediones) are not used in people who have
active liver disease or those who have had congestive heart
Oral Medications for Type 2 Diabetes
failure. These medicines are Rosiglitazone (Avandia) and Pio-
People who have type 2 diabetes may need to take one or more
glitazone (Actos). Possible side effects include liver problems,
medicines to help control their blood sugar, in addition to being
weight gain, and swelling of the feet and legs. These medicines
active & choosing healthy food.
take 2-4 weeks to begin to work when you start the medicine
and to stop working when the medicine is stopped.
The longer a person has type 2 diabetes, the more effort (and
medicine) it takes to control it.
• Medicines that slow the digestion of carbohydrates (sugar and
starches) in the small intestines are called alpha-glucosidase
People with type 2 diabetes tend to have two problems:
inhibitors. These include Acarbose (Precose) and Miglitol
1. they don't make enough insulin and
(Glyset). Side effects are common and include bloating, diar-
2. the cells of their bodies are unable to use the insulin as
• Because the medicines work in different ways to lower blood
glucose, they are often used together. Some combination drugs
There are different kinds of diabetes pills that work in a vari-
are Glucovance, Avandamet, Metaglip and ActoPlus Met.
ety of ways to help the body deal with these problems. There
is no "best" pill or treatment for type 2 diabetes. You may
Injected Medicines for Type 2 Diabetes
need to take more than one type of pill or pills plus insulin.
• Insulin is a hormone that lowers blood glucose by moving
The different types of diabetes pills are:
glucose from the bloodstream into the body's cells. If you have
type 2 diabetes you may need to start taking insulin based on
• Medicines that help the pancreas make more insulin. These
several factors – how long you have had diabetes, how high
medicines are called sulfonylureas and include Glyburide
your blood glucose levels are, what other medicines you take
(Diabeta, Micronase, Glynase Prestab) Glipizide (Glucotro1,
and your overall health. Taking insulin does not mean that you
Glucotrol XL) and Glimepiride (Amaryl). Possible side effects
now have type 1 diabetes. Many people with type 2 diabetes
include low blood sugar, weight gain, upset stomach, skin rash,
need to take insulin sooner or later.
• Scientists are developing new medicines for diabetes all the
• Other medicines (meglitinides) help the pancreas make more
time. In 2006, two new injectable medicines became available.
insulin, especially after meals. They are Repaglinide (Prandin)
The first is an "incretin memetic" called Exenatide (Byetta). It
boosts insulin release when the blood glucose is high, prevents
THE DIFFERENT TYPES OF INSULIN
the body from releasing too much sugar from the liver, and
Type & Name
Onset after injection
slows emptying of the stomach after meals. It often leads to
weight loss. The second is called Pramlintide (Symlin). This is
About 5-10 minutes
About 1 hour later
a copy of a human hormone called amylin and is only used in
(inject immediately
combination with insulin. It slows stomach emptying, stops the
before a meal – do not
liver from producing too much sugar, and stimulates feelings
of "fullness" after eating.
About 30 minutes
Medicines to treat Type I Diabetes
• Insulin is ALWAYS used to treat type 1 diabetes. Pills are not
useful or effective in type 1 diabetes.
• To treat type 1 diabetes, insulin may be given from 2-4 times
No peak; works the
• There are three characteristics of insulin – Onset (when the
Glargine (Lantus)
insulin starts to work), Peak (when the insulin is working the
Detemir (Levemir)
hardest) and Duration (how long the insulin works).
Combines rapid-act-
• If you take rapid, short, or intermediate-acting insulin, you need
70/30 (70% inter-
ing or short-acting
to eat on time and match your meals (and possibly snacks) and
mediate & 30% short
mealtime insulin and
intermediate-acting
your insulin injections. Your insulin should peak at the same
insulin. Designed
time blood sugar levels from meals are also peaking.
to be taken before
75/25 (75% interme-
• You may need extra insulin to lower your blood sugar if it is
diate with 25% rapid
• Pramlintide (Symlin) (see above) is also used, in combination
with insulin in type 1 diabetes.
Insulin can cause low blood sugar reactions.
• Insulin already injected can't be stopped from working.
• If you take insulin, don't skip meals.
• If your sugar is too low, you may suddenly feel shaky, sweaty,
weak, confused. You need some sugar to raise your blood sugar
(for example, ½ cup of juice, 5-7 pieces of chewable candy, 3-5
glucose tablets, 1 tube of liquid glucose, ½ cup of regular — non-
diet — soft drink)

Self-Injection of Insulin
Self-monitoring: You already do it — you just don't know it
Some prisoners with diabetes want to give their own injec-
Read your body's signs and pay atten-
tion to what it is telling you.
I can tell my sugar is ok by
However, there is no self-injection of insulin at some prisons.
Learn to recognize your feelings as- how my body feels; I don't
sociated with highs and lows.
Choosing where to inject and how to inject is very personal.
have to get up at night; I
Any person who has diabetes can
Sometimes nurses fill syringes before patients come in for their
don't have to drink a lot of
have high blood sugar.
shot. Some prisoners with diabetes worry about the accuracy of
water; it's not bothering me.
the dose and type of insulin. They
People treated with insulin and some
I always say, ‘Now that's 10 would prefer to draw up the dose
pills can have low blood sugars.
themselves and inject themselves.
units of Regular and 38 units If that's not allowed, do what you
High Blood Sugar (hyperglycemia):
can to make sure you are getting the
If your blood sugar is high, you might If I'm peeing a lot I know my
right kind and amount of insulin.
notice you have blurred vision, leg
sugar is too high.
cramps, headache, fatigue, thirst, fre-
One man described how he didn't
quent urination.
want to have two insulin shots a day because he hated the
needle. But, finally he agreed to try it. In less than two weeks,
But your sugar may be too high even
he was feeling a lot better in general, so he agreed to keep the
if you feel fine.
two shots after that.
You need to test your blood sugar
regularly to see if it is "in target" or
under 140 most of the time. You need
to test your blood sugar more than
What is monitoring?
once a day to fine tune sugar to the
Monitoring is what you do to assess how well you are managing
normal range.
your diabetes. There is the monitoring you do yourself, and there
are other types of monitoring that doctors and nurses have to
Low Blood Sugar (hypoglycemia):
do for or with you.
If your blood sugar is low, you might
notice feeling shaky, sweaty, dizzy,
It helps you know when something has to change to get better
confused, or aggressive. You might
blood sugar control.
have nightmares, have a seizure, or
Blood sugar testing and the A-1-C test give you feedback about
go unconscious. The quickest way
how you are doing with your diabetes management. If these tests
to raise your blood glucose is with
are not as good as you want them to be, something needs to be
some form of sugar, such as 3-5 glu-
changed in your management plan to improve control.
cose tablets, ½ cup of fruit juice or
5-7 pieces of hard candy or ½ cup of
Also, lab tests can identify complications of diabetes so they can
regular — not diet — soft drink .
Blood sugar testing lets you know how well you are doing
• Other lab tests monitor for complications of diabetes.
Keep a log of your blood sugar tests. Include date, time, any
Blood lipids like cholesterol and triglycerides assess risk for heart
unusual activities or meals over the last four hours before the
attack and strokes.
Urine protein or microalbumin test assesses for early signs of kid-
Note changes from your usual routine on the log, such as extra
ney damage.
exercise or missed meals, which may explain unexpected lows,
• Doctors should order specialty consultations to assess for com-
or extra food or sweets you may have eaten that may explain an
plications in the eyes and feet.
unexpected high blood sugar.
Prisoners with Type 2 Diabetes who take pills for diabetes
Look for patterns of highs or lows:
often don't get monitored as much as those with Type 1
Always low in the morning? Maybe you need a late night
Prisoners with type 2 diabetes often
Always high before dinner? Maybe you need more medicine.
If I could measure my blood
have trouble getting regular blood
sugar tests. There is often more
Unexpected low before dinner? Was there an extra hard workout
sugar I could know what to
concern by health staff for those on
eat and what not to eat.
insulin who are seen every day for
Always high after pizza lunch? Eat fewer slices next time.
Use your Blood Sugar Monitoring to Help You Make Better
Food Choices
Management of Diabetes
Notice how much food makes your next sugar test too high.
Learn how to eat from observing the effect of particular foods
on the blood sugar.
People with diabetes have a particularly hard time during
Eat less or eat something else the next time that meal is on the
During lockdown, the usual routines are disrupted.
Very limited meals such as cold cereal and milk or cheese sand-
wiches may be provided in cells. Plus, it might be difficult to get
• Doctors and nurses should do clinical assessments like blood
medicine and go to sick call.
pressure measurement to assess for hypertension (high blood
If you are prepared, you have con-
pressure) and foot exams to assess for numbness, injury or
I'm prepared for it, and I'm
in control of my situation.
It feels good if you don't have to ask
• Doctors should order lab tests to monitor the effectiveness of
anyone for things you need.
blood sugar control. Lab tests to monitor blood sugar control
include the A-1-C test every 3-6 months and fasting blood sugar
Medical Care
During lockdown, the trip to medical for injections could occur
Successful diabetes management requires good self-care. But it
also requires good health care from professionals familiar with
Insulin may be given at different times every day and not be
coordinated with meals at all.
Be serious
Be aware that there is a greater risk of bad low blood sugars when
insulin is not coordinated with meals.
Be serious about your medical problems.
If they see that you are concerned about your blood sugar and
really serious about your health, they are more likely to do things
During lockdown, you may not get as much food and meals may
not be well-balanced.
You have to be sincere. Stand out from the crowd as someone
You will probably get enough carbohydrate from the meals they
special, not someone who is always complaining or trying to
But, you can't trade with others to get more fruit and vegeta-
Don't ever refuse to go to a medical appointment; if you later
complain about medical care, they will point out your missed
You may need to provide your own snack and supplement with
protein (canned tuna or mackerel) and fruit (canned fruit).
Be informed
If possible, stockpile carbohydrate and protein foods in the event
Information empowers you as a patient.
you have lows during lockdowns.
Get as much information as you can about diabetes.
Some examples of carbohydrates are ramen noodles, rice, and
Doctors and nurses may assume you are ignorant about your
disease and dismiss you, unless you show them you know what
Some examples of proteins are peanut butter, canned fish or
is going on. Then they treat you differently.
seafood, nuts and beans.
Be active
Don't be afraid to ask.
During lockdown, because usual daily activities are disrupted,
you need to be active in the cell.
A passive convict is unlikely to get care because the medical
programs are usually passive too, waiting for the prisoner to
Learn to exercise all muscle groups alone in the cell with sit-ups,
ask for care.
dips and pull-ups off the bed. If you can, stand up bed frame on
end next to sink to make room to exercise.
Find out if tests are abnormal, what do they mean? Ask the doctor
what changes in therapy he/she is recommending and what you
should do to improve your diabetes management.
Together, passive patients and passive health staff equals inad-
• Dental cleanings
I want these things because I
equate care.
am diabetic and I am entitled
Be positive
• Pneumococcal vaccine
Advocate for yourself and learn how to present yourself to health
How to get the care you need when
staff effectively.
you are turned down
Think about what your health issues
When a diabetic patient is
Don't give up. Go up the chain of command to take your needs to
are and practice describing them.
the people who have the authority to address the problem.
serious and informed about
Learn to take advantage of the ser-
Use the grievance system. Go to sick call and request medical
his disease, health staff have vices that are available.
care. Wait 2 weeks for the medical call out. If it doesn't come, go
to be on their toes. They pay Don't be afraid to ask questions about
back to sick call and ask again. Wait some more.
your symptoms: why is this happen-
more attention.
If you are still not seen, write to the warden or whoever is the right
ing? You have to ask for what you
person in your prison to request necessary medical attention.
need. If you don't stand up for your-
James self, they will keep putting you off.
When they know you know the rules and who to
Be focused at each visit
write to, they respect you.
What is bothering you the most about your diabetes today?
Professional Monitoring
What you should be getting from medical:
Consultations with
• Blood sugar tests
• Blood pressure
Outside trips are difficult
The indignity of it all: up early, miss meals, chained up all day,
• Lipid profile (LDL-cho-
traveling and waiting for hours for just a "3 minute" consult.
lesterol, HDL cholesterol,
Then it takes days for your wrists to stop hurting from the hand-
• Dilated eye exams
Prepare well for the trip:
• Urine microalbumin (test
Go to the bathroom before you leave and dress warmly and wear
for very small amounts of
clean clothes.
protein in the urine)
Try to bring your own snack, a candy bar, stick of gum, glucose
Introduction to Diabetes
tablets, anything, in case you miss a meal and have to support
your blood sugar.
Specialists Help with Diagnosis and Management
There are day-to-day complications, called short-term or acute
You might need a specialist consultant for:
There are complications that accumulate over years, called long-
Complicated diabetes — an endrocrinologist can evaluate difficult
term or chronic complications.
to control diabetes.
Good blood sugar control helps prevent both types of complica-
To assess and treat long-term damage to other organs — eye,
nerve, or kidney specialist would be seen.
Maintenance procedures — a podiatrist cuts nails, or shaves corns
and calluses on feet.
Low blood sugar is the most common acute complication.
Specialist referrals maybe for appointments at clinics on-site or
Other acute complications are uncommon and likely to occur
to outside doctor offices.
only when type 1 diabetics don't get any insulin at all.
Approval for special or costly tests and procedures — specialist
Long-term complications include:
"gatekeepers" need to make determinations.
Eye disease: Diabetic damage to the retina (retinopathy), the
Be smart: don't refuse to go to the consult or any medical ap-
lens (cataract), and the optic nerve (glaucoma) can cause blurred
vision, cloudy vision, halos or blindness.
Remember, the appointment is in response to your request for
Kidney disease: Diabetic kidney disease first shows up as protein
care or the doctor's referral. If you refuse to go, they have an
in the urine and can progress to kidney failure and dialysis. There
excuse to never give you another chance.
are no early symptoms of kidney disease.
Use your self-control and be patient throughout the process.
Nerve damage: Diabetic nerve damage can effect sensory nerves
(tingling, numbness, or pain); motor nerves (weakness); or au-
Make the most of the consultant's opinion
tonomic nerves (dizziness, slow digestion).
Ask the consultant questions: What is the diagnosis? What treat-
Diseases of arteries: Diabetics have more diseases caused by
ment does he recommend?
blocked arteries, such as heart attacks, strokes, and cramps in
Get a copy of the consultant report and study it.
leg muscles occurring during activity.
Go to sick call after the consult and ask your facility doctor ques-
Foot problems: Diabetics have more foot problems, like sores and
tions so you can understand the consultant's report.
wounds that won't heal, infections and amputations.
Demand the treatment that was recommended by the specialist.
Attitude of staff and friends makes a difference:
Carry glucose, crackers, or candy to use when you feel low.
"He got kidney failure because he didn't take care of himself"
Be alert to the symptoms of low blood sugar so you can act to
is a common attitude.
treat it early.
Punitive attitudes like that don't help people do better.
Know how to help a diabetic who has low blood sugar
"He got kidney failure in spite of every thing he could do," is
Early: he's feeling shaky, sweaty: feed him.
more supportive.
Later: he's confused, dull witted: convince him to eat candy or
Working together, we can all do better.
glucose tablets right away.
Severe: he's out of his head: try glucose gel between the lips and
Acute Complications:
gums if you have it; try sugar packet between lips and gums if
that is all you have.
Low Blood Sugar
Emergency: he's seizing or unconscious: he needs an emergency
Recognize low blood sugar when it happens to you. Often you
glucagon shot from medical. Once he wakes up, he needs to eat
can feel it.
a large snack with both protein and carbohydrate.
Recognize low blood sugar in others. You may see it before he
or she feels it.
Chronic Complications: Feet
Know how to help, especially when someone has a seizure from
extreme low blood sugar.
The Feet of People with Diabetes Are In Danger
Feet become vulnerable after you have had diabetes for a few
Know the causes of low blood sugar:
years. Diabetic nerve damage causes numbness and injuries
Low blood sugar can be caused by:
occur due to the lack of a pain warning system.
• too much insulin
Poor circulation causes slow healing and poor resistance to infec-
tion. A minor injury may become an infected sore. If infection
• too much exercise without attention to supporting the blood
spreads out of control, amputation may become necessary.
Foot care is focused on preventing sores and infections from
• too little food such as missing a meal
starting, and, finding sores early when they do occur so treatment
• poor coordination of diet and exercise with insulin peak
can be started before the problem gets out of hand.
Self examination and hygiene
Know how to avoid lows:
Wash feet daily and inspect feet daily for sores, blisters, cuts, or
Never skip meals.
tender spots.
Eat planned small snacks throughout the day and plan ahead to
You need prompt treatment of foot sores and infections so get
support your blood sugar.
medical attention if you find any of those symptoms.
Foot exams at every medical visit
Foot fungus
The feet of people with diabetes should
Foot fungus and toe fungus are often not paid attention to.
be examined by the doctor or nurse at
But, there are lots of athlete's foot and toenail fungus in prisons.
every visit.
Always wear closed toe sandals in showers and locker rooms
You can help make sure this happens by
because walking barefoot can expose you to fungus.
taking your shoes and socks off before
the doctor comes in to see you.
Treatment of Foot Infections
Treatment of foot infections in dia- I put athlete's foot powder in
They should test sensation with a stiff
betics can be difficult.
plastic filament or tuning fork at least
my socks once a day to prevent
once a year.
Get professional help as soon as a those sore cracks between my
blister or sore is found on your daily
Nail care
foot inspection. Management of se- toes from athlete's foot. A
Try to get an experienced professional to cut your nails.
rious infections often requires a lot bad infection could start there.
of nursing care and attention: like
Don't cut nails too close because if feet are numb, you can't feel
dressing changes or soaks several
the painful warning when cutting too close. An injured nail bed
times a day.
is a possible source of infection.
It may require infirmary care or plastic surgery.
Corns and calluses
It may be hard to get all the care you need, even in an infirmary,
Don't try to shave them yourself. Get an experienced health
even when ordered by a consultant or facility physician.
professional, like a podiatrist, to shave them for you.
Don't let it go. Do as much as you can for yourself, but try to get
Foot wear
professional help as soon as you can.
My foot infection started Don't wear shoes that don't fit and never
as a blister.
Foot ulcers take a long time to heal
go barefoot.
Foot ulcers heal better if you don't walk on them. If you have a
Steve Empty shoes before putting them on. A
foot ulcer, you need to be off programs and resting off your feet
pebble in the shoe can cause a terrible sore
as much as possible.
if you walk on it all day. This could easily happen when the feet
A health professional needs to remove dead skin or callus from
are numb from diabetic nerve damage.
the edges of the ulcer weekly. The ulcer has to be kept clean and
dry with daily dressing changes.
Nerve damage reduces natural oils in the skin of the lower legs
If you have an infection or a foot ulcer, it is even more important
and feet. This causes dry, cracked skin that can result in infec-
to keep your blood sugar as normal as possible.
tion.
Skin creams and moisturizers can help prevent cracking.
Know the risk
Chronic Complications: Eyes
Dilated eye exams should be done annually by an eye specialist.
Diabetes is the most common cause of blindness in adults.
Get specialist treatment before vision is noticeably damaged
Prevent eye complications with good blood sugar control.
because damage may occur before you are aware of vision prob-
The lower the A-1-C the lower the risk of diabetic eye disease.
Control eye damage with early diagnosis. Get an annual dilated
eye exam by an eye specialist.
Chronic Complications: Kidneys
Three types of eye disease occur with diabetes: cataract; glau-
Diabetes is the most common cause of kidney failure, dialysis
coma; retinal disease.
and transplant.
Cataract is a cloudy spot in the lens in
Know the risk and remember that good blood sugar control
the front of the eye and cataract causes
prevents kidney damage.
blurred vision or halos around lights.
Serious damage is occurring without any symptoms at all
Glaucoma is increased pressure in the
front part of the eye.
The first evidence of kidney damage is when protein starts leak-
ing into the urine. Eventually the damage gets so severe it causes
Eventually the pressure damages the op-
kidney failure, dialysis and a transplant is needed.
tic nerve, causing blindness.
Diabetic diseases of the retina begin with
Screen annually for microalbumin, a small
excess growth of blood vessels on the
amount of protein leaking into the urine
retina in the back of the eye. Bleeding and
Treatment with medicine called "ACE Inhibi-
scarring eventually can cause detach-
tors" or "ARBs" slows the progress of diabetic
ment of the retina and blindness.
kidney disease.
Treat eye complications
Control your blood pressure to preserve
Treat eye complications early, before serious damage has already
your kidneys
occurred. Start treatment before you have any symptoms that
Diabetic kidney disease gets worse much faster
would warn you. The only way to make an early diagnosis is to
when you have both diabetes and hypertension.
have a dilated eye exam by an eye professional every year.
Remember that a low salt diet and medicine
help control blood pressure.
Treatment depends on what the examination shows
Diabetics need tighter control of their blood
Possible treatments for eye problems are:
pressure than other people do because of the
Medicated drops to treat glaucoma.
greater risk to the kidneys and blood vessels.
Your blood pressure should be less than 130 for the top or first
Laser surgery to treat overgrowth of blood vessels on the retina.
number and less than 80 for the bottom or second number.
Cataract removal when vision is seriously effected.
Chronic Complications: Arteries
Chronic Complications: Infections
Diabetics are at greater risk for heart attack, stroke and other
The prison environment can become easily contaminated with
problems related to poor circulation like cramps in the legs.
infectious diseases due to overcrowding and poor hygiene.
Control all risk factors including cholesterol, smoking, hyperten-
Greater risk of infection in diabetics
sion, blood sugar, and inactivity.
Lung infections more common in prison include influenza, bacte-
Do you know your lipid profile?
rial pneumonia, and tuberculosis. Because tuberculosis is more
common in prisons, get screened annually.
Your lipid profile includes: Total cholesterol, LDL cholesterol,
HDL cholesterol, Triglycerides.
Poor circulation, numbness and high
sugar all contribute to foot infections.
Improve lipid profile with a low saturated fat, low cholesterol
Don't use needles for tattooing or shoot-
ing up because contaminated needles in
Add medicine ("statins") if diet doesn't get lipids into target
prison are more likely to transmit HIV,
hepatitis C and hepatitis B.
Target total cholesterol is below 200.
Protect yourself by maintaining good
Target LDL-cholesterol is below 100.
personal hygiene
What to do to reduce the risk of heart attack and stroke
Don't touch the handrails.
Stop smoking.
Wash hands frequently and always wash
hands when you come back to your cell
Exercise regularly.
before you touch anything.
Eat less animal fat like butter, cream, poultry skin, fatty meats
Floors, especially in showers, are con-
and sausage products.
taminated with foot fungus. So never go
Eat less cholesterol, which is in foods like eggs and liver.
barefoot and always wear closed toe sandals in the shower.
Eat more fruits and vegetables, especially raw vegetables.
Protect yourself by getting immunized
Eat more high fiber foods like whole grains and oats.
Influenza is common in winter. Get the flu vaccine when it is
Get blood tests to measure the fats in the blood so you know if
you have a problem.
Diabetics are more prone to bacterial pneumonia. Get the pneu-
movax vaccine when it is offered.
Take medicine to reduce fats in the blood if they are too high
and cannot be controlled with diet and activity.
Prisoners are more likely to be exposed to hepatitis A and B. Get
the hepatitis A vaccine and the hepatitis B vaccine series of three
shots if they are offered.
Chronic Complications:
Teeth and Gums
Diabetics are at greater risk for gum disease
and need meticulous oral hygiene and more
frequent cleanings.
If you can't get dental hygienist care? Do bet-
ter self-care.
Make sure to do prolonged brushing twice a
day and if available, use an electric toothbrush,
floss regularly twice a day, and use an antiseptic
Different types of nerves can be involved
Motor nerves: Causes weakness.
Sensory nerves: Causes pain, numbness or tingling.
Autonomic nerves: Causes dizziness right after standing up, stom-
ach fullness for hours after meals, inability to have an erection.
BLOOD SUGAR DIARY >> NAME:
HEALTH TESTS >> NAME:
ATES AND RESUL
ovider about these tes
our blood sugar r
t the amount and an
ve eaten, the times and types of
eactions and gener
." Lis ed "Insulin.
, in the comments section. Describe
our life with diabetes
o Use the Blood Sug
e copies of these pages and write y
M the bo insulin tak of special or unusual foods y exer your feelings
• Annual dental examination and cleaning;
The Legal Right to Medical Care
• Regular, scheduled, chronic care appointments with a doctor
The Eighth Amendment to the U. S. Constitution gives con-
or specially trained nurse;
victed inmates the right to adequate medical care; the Due
Process Clause gives this same right to pretrial detainees.
• Annual flu shot.
This means that, as a person with diabetes, you probably
If you are not getting this care, you may want to file a griev-
have the right to the following, which is minimally adequate
ance or, if necessary, a lawsuit to protect your rights under
medical care: (See also the American Diabetes Association's
the Eighth Amendment. To bring a lawsuit based on the
"Diabetes Management in Correctional Institutions" which
Eighth Amendment, you need to know the following:
is reprinted at the end of this booklet.)• If you use insulin, at least twice-daily finger sticks to check
The Four Elements of an Eighth Amendment
your blood sugar levels; if you do not use insulin, finger sticks
Medical Care Claim
as often as necessary for adequate diabetes control;
There are four things you must prove in order to win a
medical care claim: (1) a serious medical need; (2) the prison
• A treatment plan which includes treatment targets for blood
official's actual knowledge of your serious medical need; (3)
that prison official's failure to reasonably respond by provid-
• A1C testing every three to six months, depending on how well
ing you adequate treatment (this is called "deliberate indif-
your blood sugar is controlled;
ference"); and (4) that the official's "deliberate indifference"
caused you an injury or is likely to injure you in the future.
• Insulin and other medications needed to help control your
1. Serious Medical Need
• Referral to specialists when necessary to treat complications
The Constitution gives inmates a right to treatment only for
resulting from your diabetes (like an eye doctor, kidney doc-
medical needs that are "serious." Many medical conditions
endanger a person's life and are clearly serious, such as dia-
• Access to prompt treatment for hypoglycemia (low blood
betes, HIV/AIDS, tuberculosis, cancer, broken bones, open
wounds. But a medical condition does not have to be life-
threatening to be considered serious. A medical need is seri-
• Access to prompt treatment in the event of high blood sugar
ous when it "has been diagnosed by a physician as mandating
treatment or . . is so obvious that even a lay person would
• Annual dilated eye exams;
easily recognize the necessity for a doctor's attention."
• Foot exams as part of regular diabetes chronic care appoint-
2. Official's Knowledge of Need
ments and special footwear when medically necessary;
If you become sick or injured, you need to do everything you
• Annual urine protein testing (microalbumin test) for kidney
can to tell officials about your problem, such as filing written
grievances. You have no right to medical treatment if no one
knows about your problem.
• Lipid level testing;
3. Failure to Provide Treatment
Once officials know about your serious medical need, they
must respond reasonably. What kind of response does the
This handbook is a summary of the ideas and experiences
Constitution require? Ideally, you should be promptly exam-
discussed during the approximately ten years of regular
ined by qualified medical personnel, prescribed or ordered
meetings of the diabetes support group at Great Meadow
the necessary treatment, given that treatment properly, and
Correctional Facility in Comstock, NY. Many people contrib-
then provided follow-up attention as needed. As you know,
uted to this handbook. The most important contributors are
however, life in jail or prison is sometimes far from ideal.
the past and present group participants. Prisoners at Great
According to the Supreme Court, officials only violate the
Meadow joined the group for various reasons. Some had
Constitution when they intentionally deny or delay access to
diabetes themselves and wanted to learn more about how
medical care, provide grossly inadequate treatment, or inten-
to take care of themselves. Others had family members with
tionally interfere with prescribed treatment.
diabetes and wanted to understand more about their family
members' health needs. Through their willingness to share
4. Causation And Injury
their stories, concerns, and lessons learned, they taught us a
lot about how to live with diabetes in very difficult circum-
Finally, to win a medical care claim, you must show that the
officials' deliberate indifference caused you, or is likely to
cause you, an injury or serious medical harm, such as blind-
To write the handbook, we started with notes taken by Mi-
ness, amputation, or kidney failure.
chael Cohen during the group sessions, sorted the ideas by
subject, and ordered them logically for presentation. Then,
For more information, you can order a book published by the
each section of the handbook was reviewed, discussed and
Southern Poverty Law Center, called Protecting Your Health
improved in the diabetes support group.
and Safety: A Litigation Guide for Inmates. To order a copy,
send a check or money order for $10.00 (this covers postage
We are also deeply grateful to Rhonda Brownstein and Rosi
and handling) to:
Smith of the Southern Poverty Law Center, who not only
wrote the section on legal rights, but responded with imme-
Protecting Your Health & Safety
diate enthusiasm and support for publishing the handbook.
Prison Legal News
Lake Worth, FL 33460
—Michael D. Cohen, MD
and Kathryn Godley, MS, RN, CDE
Be sure to include your name, prison identification number,
mailing address, and any other necessary information for get-
For additional FREE copies of the Prisoner Diabetes
ting the book to you.
Handbook please write to:Prison Legal News
Lake Worth, FL 33460
Be sure to include your name, prison identification number, mailing ad-dress, and any other necessary information for getting the book to you.
Diabetes Management in
Correctional Institutions
AMERICAN DIABETES ASSOCIATION
At any given time, over 2 million people are incarcerated in prisons and jails in the U.S. (1). It is estimated that nearly 80,000 of these inmates have diabetes, a prevalence of 4.8% (2). In addition, many more people pass through the corrections system in a given year. In 1998 alone, over 11 mil-lion people were released from prison to the community (1). The current estimated prevalence of diabetes in correctional institutions is somewhat lower than the overall U.S. prevalence of diabetes, perhaps because the incarcerated population is younger than the general population. The preva-lence of diabetes and its related comorbidities and complications, however, will continue to increase in the prison population as current sentencing guidelines continue to increase the number of aging prisoners and the incidence of diabetes in young people continues to increase.
People with diabetes in correctional facilities should receive care that
meets national standards. Correctional institutions have unique circum-stances that need to be considered so that all standards of care may be achieved (3). Correctional institutions should have written policies and procedures for the management of diabetes and for training of medical and correctional staff in diabetes care practices. These policies must take into consideration issues such as security needs, transfer from one facil-ity to another, and access to medical personnel and equipment, so that all appropriate levels of care are provided. Ideally, these policies should encourage or at least allow patients to self-manage their diabetes. Ulti-mately, diabetes management is dependent upon having access to needed medical personnel and equipment. Ongoing diabetes therapy is important in order to reduce the risk of later complications, including cardiovascular events, visual loss, renal failure, and amputation. Early identification and intervention for people with diabetes is also likely to reduce short-term risks for acute complications requiring transfer out of the facility, thus improving security.
This document provides a general set of guidelines for diabetes care in
correctional institutions. It is not designed to be a diabetes management manual. More detailed information on the management of diabetes and
Originally approved 1989. Most recent review, 2006.
related disorders can be found in the American Diabetes Association (ADA)
Abbreviations: CBG, capillary blood glucose; DKA, diabetic ketoacidosis; GDM, gestational
Clinical Practice Recommendations, published each year in January as the
diabetes mellitus; MNT, medical nutrition therapy.
first supplement to Diabetes Care, as well as the "Standards of Medical Care
DOI: 10. 2337/dc07-S077
in Diabetes" (4) contained therein. This discussion will focus on those areas
Copyright 2007 American Diabetes Association.
where the care of people with diabetes in correctional facilities may differ,
From Diabetes Care® Vol. 30, 2007; S77-S84Reprinted with permission from The American Diabetes Association
and specific recommendations are made at the end of each section.
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
INTAKE MEDICAL ASSESSMENT
Within 1-2 hrs. RECEPTION SCREENING
• Identify all inmates with diabetes currently using insulin
Reception screening
therapy or at high risk for hypoglycemia
Reception screening should emphasize patient safety. In particular, rapid identification of all insulin-treated persons with diabetes is essential in
• ALL insulin treated patients: screening CBG and urine ketone
test (as clinically indicated)
order to identify those at highest risk for hypo-and hyperglycemia and diabetic ketoacidosis (DKA). All insulin-treated patients should have a
• Any patient exhibiting signs/symptoms consistent with hypo-
glycemia: immediate CBG
capillary blood glucose (CBG) determination within 1–2 h of arrival. Signs and symptoms of hypo- or hyperglycemia can often be confused with in-
• Continue usual meal schedule and medication administration
toxication or withdrawal from drugs or alcohol. Individuals with diabetes exhibiting signs and symptoms consistent with hypoglycemia, particularly
Within 2-24 hrs. INTAKE SCREENING
altered mental status, agitation, combativeness, and diaphoresis, should
• Type and duration of diabetes
have finger-stick blood glucose levels measured immediately.
• Confirm current therapy
Intake screening
• Presence of complications
Patients with a diagnosis of diabetes should have a complete medical history
• Family history
and physical examination by a licensed health care provider with prescrip-tive authority in a timely manner. If one is not available on site, one should
• Pregnancy screen in all female patients of childbearing age
be consulted by those performing reception screening. The purposes of this history and physical examination are to determine the type of diabetes, cur-
• Assess alcohol use
rent therapy, alcohol use, and behavioral health issues, as well as to screen
• Identify behavioral health issues such as depression, distress,
for the presence of diabetes-related complications. The evaluation should
suicidal ideation
review the previous treatment and the past history of both glycemic control
• Assess prior diabetes education
and diabetes complications. It is essential that medication and medical nutrition therapy (MNT) be continued without interruption upon entry
All subjects with diabetes should have physician evaluation.
into the correctional system, as hiatus in either medication or appropriate
If no physician available, physician should be consulted.
nutrition may lead to either severe hypo- or hyperglycemia that can rapidly progress to irreversible complications, even death.
INTAKE PHYSICAL EXAM LABORATORY—
2 hrs. – 2 weeks
Intake physical examination and laboratory
All potential elements of the initial medical evaluation are included in
Complete exam including:
Table 5 of the ADA's "Standards of Medical Care in Diabetes," referred to
• Height, weight
• A1C and glucose
hereafter as the "Standards of Care" (4). The essential components of the initial history and physical examination are detailed in Fig. 1. Referrals
• Blood pressure
• Lipid Profile
should be made immediately if the patient with diabetes is pregnant.
• Eye (retinal) exam
• Microalbumin screen (Alb/Cr ratio)
• Urine ketones (as clinically indicated)
• Patients with diagnosis of diabetes should have a complete medical
• Peripheral pulses
• AST/ALT (as clinically indicated)
history and undergo an intake physical examination by a licensed
• Foot and neurologic exam
• Creatinine (as clinically indicated)
health professional in timely manner. (E)
• Insulin-treated patients should have CBG determination within
1–2 h of arrival. (E)
Figure 1—Essential components of the initial history and physical examination.
• Medications and MNT should be continued without interruption upon
Alb/Cr ratio, albumin-to-creatinine ratio; ALT, alanine amino-transferase;
entry into the correctional environment. (E)
AST, aspartate aminotransferase.
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
Table 1—Summary of recommendations for adults with diabetes
SCREENING FOR DIABETES
Consistent with the ADA Standards of Care, patients should be evaluated
for diabetes risk factors at the intake physical and at appropriate times thereafter. Those who are at high risk should be considered for blood glucose
screening. If pregnant, a risk assessment for gestational diabetes mellitus
Preprandial capillary plasma glucose
90–130 mg/dl (5. 0–7. 2 mmol/l)
(GDM) should be undertaken at the first prenatal visit. Patients with clinical
Peak postprandial capillary plasma glucose† <180 mg/dl (<10. 0 mmol/l)
characteristics consistent with a high risk for GDM should undergo glucose
testing as soon as possible. High-risk women not found to have GDM at the initial screening and average-risk women should be tested between 24 and 28 weeks of gestation. For more detailed information on screening for both
Lipids‡
type 2 and gestational diabetes, see the ADA Position Statement "Screening
<100 mg/dl (<2. 6 mmol/l)
for Type 2 Diabetes" (5) and the Standards of Care (4).
<150 mg/dl (<1. 7 mmol/l)
>40 mg/dl (>1. 0 mmol/l)§
MANAGEMENT PLAN
Glycemic control is fundamental to the management of diabetes. A manage-
Key concepts in setting glycemic goals:
ment plan to achieve normal or near-normal glycemia with an A1C goal of <7% should be developed for diabetes management at the time of initial
• A1C is the primary target for glycemic control
medical evaluation. Goals should be individualized (4), and less stringent
• Goals should be individualized
treatment goals may be appropriate for patients with a history of severe
• Certain populations (children, pregnant women, and elderly) require special
hypoglycemia, patients with limited life expectancies, elderly adults, and
individuals with comorbid conditions (4). This plan should be documented
• More stringent glycemic goals (i. e., normal A1C, <6%) may further reduce
in the patient's record and communicated to all persons involved in his/her
complications at the cost of increased risk of hypoglycemia
care, including security staff. Table 1, taken from the ADA Standards of Care,
• Less intensive glycemic goals may be indicated in patients with severe or fre-
provides a summary of recommendations for setting glycemic control goals
quent hypoglycemia
for adults with diabetes.
• Postprandial glucose may be targeted if A1C goals are not met despite reaching
People with diabetes should ideally receive medical care from a physi-
preprandial glucose goals
cian-coordinated team. Such teams include, but are not limited to, physi-cians, nurses, dietitians, and mental health professionals with expertise
*Referenced to a nondiabetic range of 4. 0–6. 0% using DCCT-based assay. †Postprandial
and special interest in diabetes. It is essential in this collaborative and
glucose measurements should be made 1–2 h after the beginning of the meal, generally peak
levels in patients with diabetes. ‡Current NCEP/ATP III guidelines suggest that in patients
integrated team approach that individuals with diabetes assume as active
with triglycerides ≥200 mg/dl, the "non-HDL cholesterol" (total cholesterol minus HDL) be
a role in their care as possible. Diabetes self-management education is an
utilized. The goal is ≤130 mg/dl (121). §For women, it has been suggested that the HDL goal
be increased by 10 mg/dl.
integral component of care. Patient self-management should be emphasized, and the plan should encourage the involvement of the patient in problem solving as much as possible.
It is helpful to house insulin-treated patients in a common unit, if this
NUTRITION AND FOOD SERVICES
is possible, safe, and consistent with providing access to other programs
Nutrition counseling and menu planning are an integral part of the multi-
at the correctional institution. Common housing not only can facilitate
disciplinary approach to diabetes management in correctional facilities. A
mealtimes and medication administration, but also potentially provides
combination of education, interdisciplinary communication, and monitoring
an opportunity for diabetes self-management education to be reinforced
food intake aids patients in understanding their medical nutritional needs
by fellow patients.
and can facilitate diabetes control during and after incarceration.
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
Nutrition counseling for patients with diabetes is considered an es-
sential component of diabetes self-management. People with diabetes
Severe hyperglycemia in a person with diabetes may be the result of inter-
should receive individualized MNT as needed to achieve treatment goals,
current illness, missed or inadequate medication, or corticosteroid therapy.
preferably provided by a registered dietitian familiar with the components
Correctional institutions should have systems in place to identify and refer
of MNT for persons with diabetes.
to medical staff all patients with consistently elevated blood glucose as well
Educating the patient, individually or in a group setting, about how
as intercurrent illness.
carbohydrates and food choices directly affect diabetes control is the first
The stress of illness in those with type 1 diabetes frequently aggravates
step in facilitating self-management. This education enables the patient
glycemic control and necessitates more frequent monitoring of blood glucose
to identify better food selections from those available in the dining hall
(e.g., every 4–6 h). Marked hyperglycemia requires temporary adjustment
and commissary. Such an approach is more realistic in a facility where the
of the treatment program and, if accompanied by ketosis, interaction with
patient has the opportunity to make food choices.
the diabetes care team. Adequate fluid and caloric intake must be ensured.
The easiest and most cost-effective means to facilitate good outcomes
Nausea or vomiting accompanied with hyperglycemia may indicate DKA,
in patients with diabetes is instituting a heart-healthy diet as the master
a life-threatening condition that requires immediate medical care to pre-
menu (6). There should be consistent carbohydrate content at each meal,
vent complications and death. Correctional institutions should identify
as well as a means to identify the carbohydrate content of each food selec-
patients with type 1 diabetes who are at risk for DKA, particularly those
tion. Providing carbohydrate content of food selections and/or providing
with a prior history of frequent episodes of DKA. For further information
education in assessing carbohydrate content enables patients to meet the
see "Hyperglycemic Crisis in Diabetes" (8).
requirements of their individual MNT goals. Commissaries should also
help in dietary management by offering healthy choices and listing the
Hypoglycemia is defined as a blood glucose level <60 mg/dl. Severe hy-
carbohydrate content of foods.
poglycemia is a medical emergency defined as hypoglycemia requiring
The use of insulin or oral medications may necessitate snacks in order
assistance of third party and is often associated with mental status changes
to avoid hypoglycemia. These snacks are a part of such patients' medical
that may include confusion, incoherence, combativeness, somnolence,
treatment plans and should be prescribed by medical staff.
lethargy, seizures, or coma. Signs and symptoms of severe hypoglycemia
Timing of meals and snacks must be coordinated with medication ad-
can be confused with intoxication or withdrawal. Individuals with diabetes
ministration as needed to minimize the risk of hypoglycemia, as discussed
exhibiting signs and symptoms consistent with hypoglycemia, particularly
more fully in the MEDICATION section of this document. For further
altered mental status, agitation, and diaphoresis, should have their CBG
information, see the ADA Position Statement "Nutrition Principles and
levels checked immediately.
Recommendations in Diabetes" (7).
Security staff who supervise patients at risk for hypoglycemia (i.e., those
on insulin or oral hypoglycemic agents) should be educated in the emergency
URGENT AND EMERGENCY ISSUES
response protocol for recognition and treatment of hypoglycemia. Every attempt should be made to document CBG before treatment. Patients must
All patients must have access to prompt treatment of hypo- and hyperglyce-
have immediate access to glucose tablets or other glucose-containing foods.
mia. Correctional staff should be trained in the recognition and treatment
Hypoglycemia can generally be treated by the patient with oral carbohy-
of hypo- and hyperglycemia, and appropriate staff should be trained to
drates. If the patient cannot be relied on to keep hypoglycemia treatment on
administer glucagon. After such emergency care, patients should be referred
his/her person, staff members should have ready access to glucose tablets
for appropriate medical care to minimize risk of future decompensation.
or equivalent. In general, 15–20 g oral glucose will be adequate to treat
Institutions should implement a policy requiring staff to notify a physi-
hypoglycemic events. CBG and treatment should be repeated at 15-min
cian of all CBG results outside of a specified range, as determined by the
intervals until blood glucose levels return to normal (>70 mg/dl).
treating physician (e.g., <50 or >350 mg/dl).
Staff should have glucagon for intramuscular injection or glucose for
intravenous infusion available to treat severe hypoglycemia without re-quiring transport of the hypoglycemic patient to an outside facility. Any
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
episode of severe hypoglycemia or recurrent episodes of mild to moder-
of supervision necessary. When needed, this skill should be a part of patient
ate hypoglycemia require reevaluation of the diabetes management plan
education. Reasonable syringe control systems should be established.
by the medical staff. In certain cases of unexplained or recurrent severe
In the past, the recommendation that regular insulin be injected 30–45
hypoglycemia, it may be appropriate to admit the patient to the medical
min before meals presented a significant problem when "lock downs" or
unit for observation and stabilization of diabetes management.
other disruptions to the normal schedule of meals and medications occurred.
Correctional institutions should have systems in place to identify the
The use of multiple-dose insulin regimens using rapid-acting analogs can
patients at greater risk for hypoglycemia (i.e., those on insulin or sulfonylurea
decrease the disruption caused by such changes in schedule. Correctional
therapy) and to ensure the early detection and treatment of hypoglycemia.
institutions should have systems in place to ensure that rapid-acting insulin
If possible, patients at greater risk of severe hypoglycemia (e.g., those with
analogs and oral agents are given immediately before meals if this is part
prior episode of severe hypoglycemia) may be housed in units closer to the
of the patient's medical plan. It should be noted however that even mod-
medical unit in order to minimize delay in treatment.
est delays in meal consumption with these agents can be associated with hypoglycemia. If consistent access to food within 10 min cannot be ensured,
rapid-acting insulin analogs and oral agents are approved for administration
• Train correctional staff in the recognition, treatment, and appropriate
during or immediately after meals. Should circumstances arise that delay
referral for hypo-and hyperglycemia. (E)
patient access to regular meals following medication administration, poli-
• Train appropriate staff to administer glucagon. (E)
cies and procedures must be implemented to ensure the patient receives
• Train staff to recognize symptoms and signs of serious metabolic
appropriate nutrition to prevent hypoglycemia.
decompensation, and immediately refer the patient for appropriate
Both continuous subcutaneous insulin infusion and multiple daily insu-
medical care. (E)
lin injection therapy (consisting of three or more injections a day) can be
• Institutions should implement a policy requiring staff to notify a physi-
effective means of implementing intensive diabetes management with the
cian of all CBG results outside of a specified range, as determined by
goal of achieving near-normal levels of blood glucose (9). While the use of
the treating physician (e.g., <50 or >350 mg/dl). (E)
these modalities may be difficult in correctional institutions, every effort
• Identify patients with type 1 diabetes who are at high risk for DKA.
should be made to continue multiple daily insulin injection or continuous
subcutaneous insulin infusion in people who were using this therapy before incarceration or to institute these therapies as indicated in order to achieve
MEDICATION
blood glucose targets.
It is essential that transport of patients from jails or prisons to off-site
Formularies should provide access to usual and customary oral medica-
appointments, such as medical visits or court appearances, does not cause
tions and insulins necessary to treat diabetes and related conditions. While
significant disruption in medication or meal timing. Correctional institutions
not every brand name of insulin and oral medication needs to be available,
and police lockups should implement policies and procedures to diminish
individual patient care requires access to short-, medium-, and long-acting
the risk of hypo-and hyperglycemia by, for example, providing carry-along
insulins and the various classes of oral medications (e.g., insulin secre-
meals and medication for patients traveling to off-site appointments or
tagogues, biguanides, a-glucosidase inhibitors, and thiazolidinediones)
changing the insulin regimen for that day. The availability of prefilled insulin
necessary for current diabetes management.
"pens" provides an alternative for off-site insulin delivery.
Patients at all levels of custody should have access to medication at dos-
ing frequencies that are consistent with their treatment plan and medical
direction. If feasible and consistent with security concerns, patients on
• Formularies should provide access to usual and customary oral medica-
multiple doses of short-acting oral medications should be placed in a "keep
tions and insulins to treat diabetes and related conditions. (E)
on person" program. In other situations, patients should be permitted to
• Patients should have access to medication at dosing frequencies that
self-inject insulin when consistent with security needs. Medical depart-
are consistent with their treatment plan and medical direction. (E)
ment nurses should determine whether patients have the necessary skill and responsible behavior to be allowed self-administration and the degree
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
• Correctional institutions and police lock-ups should implement poli-
(75–162 mg/day) in all adult patients with diabetes and cardiovascular
cies and procedures to diminish the risk of hypo-and hyperglycemia
risk factors or known macrovascular disease. Current national stan-
during off-site travel (e.g., court appearances). (E)
dards for adults with diabetes call for treatment of lipids to goals of LDL <_100, HDL >40, triglycerides <150 mg/dl and blood pressure to level of <130/80 mmHg.
ROUTINE SCREENING FOR AND MANAGEMENT OF
DIABETES COMPLICATIONS
MONITORING/TESTS OF GLYCEMIA
All patients with a diagnosis of diabetes should receive routine screening for diabetes-related complications, as detailed in the ADA Standards of
Monitoring of CBG is a strategy that allows caregivers and people with
Care (4). Interval chronic disease clinics for persons with diabetes provide
diabetes to evaluate diabetes management regimens. The frequency of
an efficient mechanism to monitor patients for complications of diabetes.
monitoring will vary by patients' glycemic control and diabetes regimens.
In this way, appropriate referrals to consultant specialists, such as optom-
Patients with type 1 diabetes are at risk for hypoglycemia and should have
etrists/ophthalmologists, nephrologists, and cardiologists, can be made on
their CBG monitored three or more times daily. Patients with type 2 dia-
an as-needed basis and interval laboratory testing can be done.
betes on insulin need to monitor at least once daily and more frequently
The following complications should be considered.
based on their medical plan. Patients treated with oral agents should have CBG monitored with sufficient frequency to facilitate the goals of glycemic
• Foot care: Recommendations for foot care for patients with diabetes
control, assuming that there is a program for medical review of these data
and no history of an open foot lesion are described in the ADA Stan-
on an ongoing basis to drive changes in medications. Patients whose dia-
dards of Care. A comprehensive foot examination is recommended
betes is poorly controlled or whose therapy is changing should have more
annually for all patients with diabetes to identify risk factors predictive
frequent monitoring. Unexplained hyperglycemia in a patient with type 1
of ulcers and amputations. Persons with an insensate foot, an open
diabetes may suggest impending DKA, and monitoring of ketones should
foot lesion, or a history of such a lesion should be referred for evalua-
therefore be performed.
tion by an appropriate licensed health professional (e.g., podiatrist or
Glycated hemoglobin (A1C) is a measure of long-term (2- to 3-month)
vascular surgeon). Special shoes should be provided as recommended
glycemic control. Perform the A1C test at least two times a year in patients
by licensed health professionals to aid healing of foot lesions and to
who are meeting treatment goals (and who have stable glycemic control)
prevent development of new lesions.
and quarterly in patients whose therapy has changed or who are not meet-
• Retinopathy: Annual retinal examinations by a licensed eye care pro-
ing glycemic goals.
fessional should be performed for all patients with diabetes, as recom-
Discrepancies between CBG monitoring results and A1C may indicate
mended in the ADA Standards of Care. Visual changes that cannot be
a hemoglobinopathy, hemolysis, or need for evaluation of CBG monitoring
accounted for by acute changes in glycemic control require prompt
technique and equipment or initiation of more frequent CBG monitoring
evaluation by an eye care professional.
to identify when glycemic excursions are occurring and which facet of the
• Nephropathy: An annual spot urine test for determination of micro-
diabetes regimen is changing.
albumin-to-creatinine ratio should be performed. The use of ACE
In the correctional setting, policies and procedures need to be developed
inhibitors or angiotensin receptor blockers is recommended for all
and implemented regarding CBG monitoring that address the following.
patients with albuminuria. Blood pressure should be controlled to
<130/80 mmHg.
• Infection control
• Cardiac: People with type 2 diabetes are at a particularly high risk of
• Education of staff and patients
coronary artery disease. Cardiovascular disease risk factor management
• Proper choice of meter
is of demonstrated benefit in reducing this complication in patients
• Disposal of testing lancets
with diabetes. Blood pressure should be measured at every routine
• Quality control programs
diabetes visit. In adult patients, test for lipid disorders at least annually
• Access to health services
and as needed to achieve goals with treatment. Use aspirin therapy
• Size of the blood sample
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
• Patient performance skills
Table 2—Major components of diabetes self-management education
• Documentation and interpretation of test results • Availability of test results for the health care provider (10)
Survival skills
Daily management issues
• Hypo-/hyperglycemia
• Disease process
• In the correctional setting, policies and procedures need to be de-
• Sick day management
• Nutritional management
veloped and implemented to enable CBG monitoring to occur at the
• Physical activity
frequency necessitated by the individual patient's glycemic control and diabetes regimen. (E)
• A1C should be checked every 3–6 months. (E)
• Monitoring • Acute complications
SELF-MANAGEMENT EDUCATION
• Risk reduction
Self-management education is the cornerstone of treatment for all people
• Goal setting/problem solving
with diabetes. The health staff must advocate for patients to participate
• Psychosocial adjustment
in self-management as much as possible. Individuals with diabetes who
• Preconception care/pregnancy/
learn self-management skills and make lifestyle changes can more effec-
gestational diabetes management
tively manage their diabetes and avoid or delay complications associated with diabetes. In the development of diabetes self-management education
• What is diabetes
program in the correctional environment, the unique circumstances of the
• Signs and symptoms of diabetes
patient should be considered while still providing, to the greatest extent
• Risk factors
possible, the elements of the "National Standards for Diabetes Self-Man-
• Signs and symptoms of, and emergency response to, hypo- and
agement Education" (11). A staged approach may be used depending on
the needs assessment and the length of incarceration. Table 2 sets out the
• Glucose monitoring
major components of diabetes self-management education. Survival skills
should be addressed as soon as possible; other aspects of education may be
provided as part of an ongoing education program.
• Nutrition issues including timing of meals and access to snacks
Ideally, self-management education is coordinated by a certified diabe-
tes educator who works with the facility to develop polices, procedures,
and protocols to ensure that nationally recognized education guidelines
• Include diabetes in correctional staff education programs. (E)
are implemented. The educator is also able to identify patients who need diabetes self-management education, including an assessment of the pa-
ALCOHOL AND DRUGS
tients' medical, social, and diabetes histories; diabetes knowledge, skills, and behaviors; and readiness to change.
Patients with diabetes who are withdrawing from drugs and alcohol need special consideration. This issue particularly affects initial police custody and jails. At an intake facility, proper initial identification and assessment
STAFF EDUCATION
of these patients are critical. The presence of diabetes may complicate
Policies and procedures should be implemented to ensure that the health
detoxification. Patients in need of complicated detoxification should be
care staff has adequate knowledge and skills to direct the management and
referred to a facility equipped to deal with high-risk detoxification. Patients
education of persons with diabetes. The health care staff needs to be involved
with diabetes should be educated in the risks involved with smoking. All
in the development of the correctional officers' training program. The staff
inmates should be advised not to smoke. Assistance in smoking cessation
education program should be at a lay level. Training should be offered at
should be provided as practical.
least biannually, and the curriculum should cover the following.
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
TRANSFER AND DISCHARGE
The sending facility must be mindful of the transfer time in order to
provide the patient with medication and food if needed. The transfer sum-
Patients in jails may be housed for a short period of time before being
mary or medical record should be reviewed by a health care provider upon
transferred or released, and it is not unusual for patients in prison to be
arrival at the receiving institution.
transferred within the system several times during their incarceration.
Planning for patients' discharge from prisons should include instruction
One of the many challenges that health care providers face working in the
in the long-term complications of diabetes, the necessary lifestyle changes
correctional system is how to best collect and communicate important
and examinations required to prevent these complications, and, if possible,
health care information in a timely manner when a patient is in initial police
where patients may obtain regular follow-up medical care. A quarterly
custody, is jailed short term, or is transferred from facility to facility. The
meeting to educate patients with up coming discharges about community
importance of this communication becomes critical when the patient has
resources can be valuable. Inviting community agencies to speak at these
a chronic illness such as diabetes.
meetings and/or provide written materials can help strengthen the com-
Transferring a patient with diabetes from one correctional facility to
munity link for patients discharging from correctional facilities.
another requires a coordinated effort. To facilitate a thorough review of
Discharge planning for the patients with diabetes should begin 1 month
medical information and completion of a transfer summary, it is critical for
before discharge. During this time, application for appropriate entitlements
custody personnel to provide medical staff with sufficient notice before
should be initiated. Any gaps in the patient's knowledge of diabetes care
movement of the patient.
need to be identified and addressed. It is helpful if the patient is given a
Before the transfer, the health care staff should review the patient's
directory or list of community resources and if an appointment for follow-up
medical record and complete a medical transfer summary that includes the
care with a community provider is made. A supply of medication adequate
patient's current health care issues. At a minimum, the summary should
to last until the first postrelease medical appointment should be provided
include the following.
to the patient upon release. The patient should be provided with a written summary of his/her current heath care issues, including medications and
• The patient's current medication schedule and dosages
doses, recent A1C values, etc.
• The date and time of the last medication administration • Any recent monitoring results (e.g., CBG and A1C)
• Other factors that indicate a need for immediate treatment or manage-
• For all interinstitutional transfers, complete a medical transfer sum-
ment at the receiving facility (e.g., recent episodes of hypoglycemia,
mary to be transferred with the patient. (E)
history of severe hypoglycemia or frequent DKA, concurrent illnesses,
• Diabetes supplies and medication should accompany the patient dur-
presence of diabetes complications)
ing transfer. (E)
• Information on scheduled treatment/appointments if the receiving fa-
• Begin discharge planning with adequate lead time to insure continuity
cility is responsible for transporting the patient to that appointment
of care and facilitate entry into community diabetes care. (E)
• Name and telephone/fax number of a contact person at the transferring
facility who can provide additional information, if needed
SHARING OF MEDICAL INFORMATION AND RECORDS
The medical transfer summary, which acts as a quick medical reference
Practical considerations may prohibit obtaining medical records from
for the receiving facility, should be transferred along with the patient. To
providers who treated the patient before arrest. Intake facilities should
supplement the flow of information and to increase the probability that
implement policies that 1) define the circumstances under which prior
medications are correctly identified at the receiving institution, sending
medical records are obtained (e.g., for patients who have an extensive
institutions are encouraged to provide each patient with a medication card
history of treatment for complications); 2) identify person(s) responsible
to be carried by the patient that contains information concerning diagnoses,
for contacting the prior provider; and 3) establish procedures for tracking
medication names, dosages, and frequency. Diabetes supplies, including
diabetes medication, should accompany the patient.
Facilities that use outside medical providers should implement policies
and procedures for ensuring that key information (e.g., test results, diagnoses,
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
physicians' orders, appointment dates) is received from the provider and
PREGNANCY
incorporated into the patient's medical chart after each outside appoint-
Pregnancy in a woman with diabetes is by definition a high-risk pregnancy.
ment. The procedure should include, at a minimum, a means to highlight
Every effort should be made to ensure that treatment of the pregnant
when key information has not been received and designation of a person
woman with diabetes meets accepted standards (14,15). It should be noted
responsible for contacting the outside provider for this information.
that glycemic standards are more stringent, the details of dietary manage-
All medical charts should contain CBG test results in a specified, readily
ment are more complex and exacting, insulin is the only antidiabetic agent
accessible section and should be reviewed on a regular basis.
approved for use in pregnancy, and a number of medications used in the management of diabetic comorbidities are known to be teratogenic and
CHILDREN AND ADOLESCENTS WITH DIABETES
must be discontinued in the setting of pregnancy.
Children and adolescents with diabetes present special problems in disease management, even outside the setting of a correctional institution. Chil-
SUMMARY AND KEY POINTS
dren and adolescents with diabetes should have initial and follow-up care
People with diabetes should receive care that meets national standards.
with physicians who are experienced in their care. Confinement increases
Being incarcerated does not change these standards. Patients must have
the difficulty in managing diabetes in children and adolescents, as it does
access to medication and nutrition needed to manage their disease. In
in adults with diabetes. Correctional authorities also have different legal
patients who do not meet treatment targets, medical and behavioral plans
obligations for children and adolescents.
should be adjusted by health care professionals in collaboration with the
Nutrition and activity
prison staff. It is critical for correctional institutions to identify particularly
Growing children and adolescents have greater caloric/nutritional needs
high-risk patients in need of more intensive evaluation and therapy, includ-
than adults. The provision of an adequate amount of calories and nutrients
ing pregnant women, patients with advanced complications, a history of
for adolescents is critical to maintaining good nutritional status. Physical
repeated severe hypoglycemia, or recurrent DKA.
activity should be provided at the same time each day. If increased physi-
A comprehensive, multidisciplinary approach to the care of people with
cal activity occurs, additional CBG monitoring is necessary and additional
diabetes can be an effective mechanism to improve overall health and delay
carbohydrate snacks may be required.
or prevent the acute and chronic complications of this disease.
Medical management and follow-up
Children and adolescents who are incarcerated for extended periods should
have follow-up visits at least every 3 months with individuals who are ex-
perienced in the care of children and adolescents with diabetes. Thyroid
function tests and fasting lipid and microalbumin measurements should be
performed according to recognized standards for children and adolescents
(12) in order to monitor for autoimmune thyroid disease and complications
and comorbidities of diabetes.
Children and adolescents with diabetes exhibiting unusual behavior
should have their CBG checked at that time. Because children and ado-
The following members of the American Diabetes Association/ National Commis-
lescents are reported to have higher rates of nocturnal hypoglycemia (13),
sion on Correctional Health Care Joint Working Group on Diabetes Guidelines
consideration should be given regarding the use of episodic overnight blood
for Correctional Institutions contributed to the revision of this document: Daniel
glucose monitoring in these patients. In particular, this should be consid-
L. Lorber, MD, FACP, CDE (chair); R. Scott Chavez, MPA, PA-C; Joanne Dorman,
ered in children and adolescents who have recently had their overnight
RN, CDE, CCHP-A; Lynda K. Fisher, MD; Stephanie Guerken, RD, CDE; Linda B.
insulin dose changed.
Haas, CDE, RN; Joan V. Hill, CDE, RD; David Kendall, MD; Michael Puisis, DO; Kathy Salomone, CDE, MSW, APRN; Ronald M. Shansky, MD, MPH; and Barbara Wakeen, RD, LD.
Diabetes Care, volume 30, Supplement 1, January 2007
Diabetes Care, volume 30, Supplement 1, January 2007
References
1. National Commission on Correctional Health Care: The Health Status of Soon-
to-Be Released Inmates: A Report to Congress. Vol. 1. Chicago, NCCHC, 2002
2. Hornung CA, Greifinger RB, Gadre S: A Projection Model of the Prevalence of
Selected Chronic Diseases in the Inmate Population. Vol. 2. Chicago, NCCHC, 2002, p. 39–56
3. Puisis M: Challenges of improving quality in the correctional setting. In Clini-
cal Practice in Correctional Medicine. St. Louis, MO, Mosby-Yearbook, 1998, p. 16–18
4. American Diabetes Association: Standards of medical care in diabetes—2007
(Position Statement). Diabetes Care 30 (Suppl. 1):S4–S41, 2007
5. American Diabetes Association: Screening for type 2 diabetes (Position State-
ment). Diabetes Care 27 (Suppl. 1):S11–S14, 2004
6. Krauss RM, Eckel RH, Howard B, Appel LJ, Daniels SR, Deckelbaum RJ,
Erdman JW Jr, Kris-Etherton P, Goldberg IJ, Kotchen TA, Lichtenstein AH, Mitch WE, Mullis R, Robinson K, Wylie-Rosett J, St Jeor S, Suttie J, Tribble DL, Bazzarre TL: American Heart Association Dietary Guidelines: revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Stroke 31:2751–2766, 2000
7. American Diabetes Association: Nutrition recommendations and interventions
for diabetes (Position Statement). Diabetes Care 30 (Suppl. 1):S48–S65, 2007
8. American Diabetes Association: Hyperglycemic crisis in diabetes (Position
Statement). Diabetes Care 27 (Suppl. 1):S94– S102, 2004
9. American Diabetes Association: Continuous subcutaneous insulin infusion
(Position Statement). Diabetes Care 27 (Suppl. 1):S110, 2004
10. American Diabetes Association: Tests of glycemia in diabetes (Position State-
ment). Diabetes Care 27 (Suppl. 1):S91–S93, 2004
11. American Diabetes Association: National standards for diabetes self-manage-
ment education (Standards and Review Criteria). Diabetes Care 30 (Suppl. 1):S96-S103, 2007
12. International Society for Pediatric and Adolescent Diabetes: Consensus Guide-
lines 2000: ISPAD Consensus Guidelines for the Management of Type 1 Diabe-tes Mellitus in Children and Adolescents. Zeist, Netherlands, Medical Forum International, 2000, p. 116, 118
Edited by
13. Kaufman FR, Austin J, Neinstein A, Jeng L, Halyorson M, Devoe DJ, Pituk-
Michael D. Cohen, MD
cheewanont P: Nocturnal hypoglycemia detected with the continuous glu-
Kathryn Godley, MS, RN, CDE
cose monitoring system in pediatric patients with type 1 diabetes. J Pediatr
141:625–630, 2002
Rhonda Brownstein
14. American Diabetes Association: Gestational diabetes mellitus (Position State-
ment). Diabetes Care 27 (Suppl. 1):S88-S90, 2004
15. Jovanovic L (Ed. ): Medical Management of Pregnancy Complicated by Diabetes.
3rd ed. Alexandria, VA, American Diabetes Association, 2000
Created by the Diabetes support group at
Great Meadow Correctional Facility
Comstock, New York
Diabetes Care, volume 30, Supplement 1, January 2007
Source: https://www.splcenter.org/sites/default/files/d6_legacy_files/downloads/publication/splc_prisoner_diabetes_handbook_1.pdf
Heft Nutztierhaltung 2/01 Abdruck in Absprache mit der Redaktion und unter Quellenangabe gestattet Inhaltsverzeichnis: • Veranstaltungen . 1 • Von Borell, E.: Editorial: 15. IGN-Tagung "Tierschutz und Nutztierhaltung" (2001) . 3 • EKAH und EKTV (Hrsg.): Die Würde des Tieres (2001) . 4 • Brilling, W.: Rinderzucht im Wandel (2001) . 4
MINISTERE DE L'EDUCATION NATIONALE REPUBLIQUE DE COTE D'IVOIRE ET DE L'ENSEIGNEMENT TECHNIQUE ********* INSPECTION GENERALE ******** DIRECTION DE LA PEDAGOGIE ET DE LA FORMATION CONTINUE Mot de Madame la Ministre de l'Education Nationale et de l'Enseignement