Microsoft word - 2-advances orbital handout - laver.doc
ADVANCES IN ORBITAL INFLAMMATION
Nora V. Laver, MD
Ocular Pathology Laboratory
New England Eye Center
Tufts Medical Center
Boston, Massachusetts
Learning objectives
1. To discuss the most important inflammatory orbital lesions and their
clinical frequency.
2. To familiarize the audience with the most prevalent infectious orbital
pathologies.
3. To compare and contrast the most important inflammatory orbital lesions,
including Grave's orbitopathy, inflammatory pseudotumor, infections and
other diseases.
I. INTRODUCTION
The orbit is the bony cavity that contains the eye, eye muscles, lacrimal gland,
and neural and vascular structures that serve eye function. Numerous diseases occur in the orbit that can affect visual function. While the human globe reaches its adult size by about age 3, the full adult orbital size in terms of volume is not attained until about age 16.
A mass lesion of the orbit may cause proptosis, displacement of the eye, lid
asymmetry, conjunctiva and eyelid congestion, changes in ocular motility and even decreased visual acuity. Orbital lesions may be the presenting sign of systemic diseases, such as metastatic cancer. Demographics such as age, sex, and location within the orbit may be helpful in making a specific diagnosis. Treatment of orbital lesions may be medical, such as the use of steroids or radiotherapy for inflammatory disease, and does not always require surgery.
Inflammatory conditions of the orbit, whether they be focally tumefactive or
diffusely infiltrating, are the result of blood-borne inflammatory cells, since there are no
indigenous lymph nodes or lymphoid aggregates in the orbit. Some orbital
inflammations have a known cause (such as fungus or bacterium), and others are
idiopathic (such cases would be Grave's disease, and orbital pseudotumor).
Inflammatory conditions of the orbit include both
infectious and
non-infectious etiologies. Inflammations and tumors comprise about 10-20% of orbital lesions (see
Table 1). Inflammatory and lymphoid lesions of the lacrimal gland are seen at about 5 x
greater frequency than glandular epithelial tumors. The lacrimal gland is a modified
salivary gland, and therefore similar inflammatory processes and tumors occur as in the
major salivary glands (i.e. sarcoid, Sjögren's, viral adenitis, etc.). The lacrimal gland is
the only location in the orbit that under normal circumstances contain lymphoid
inflammatory cells. Inflammatory processes of the deeper orbit are blood-borne, and
lymphoid proliferative diseases (i.e. lymphomas) are by-definition primary extra-nodal.
Table 1. Frequency of Orbital Lesions by Major Diagnostic Group
Diagnostic Group
Frequency (%)
Thyroid orbitopathy
Inflammatory lesions
Vascular neoplasms
Vascular, structural
Lacrimal gland lesions
Lymphoproliferative lesions 5
Secondary tumors
Mesenchymal lesions
Metastatic tumors
Optic nerve tumors
Other and unclassified
Major Causes of Orbital Inflammatory Lesions
•
Infectious Orbital Lesions
a. Orbital cellulitis
b. Fungal infections
c. Parasitic infections
d. Other orbital infections
•
Inflammatory Orbital Lesions
e. Grave's orbitopathy
f. Orbital Inflammatory Pseudotumor
g. Sarcoidosis
h. Amyloid deposition
i. Vasculitis
j. Benign lymphoepithelial lesion
k. Histiocytic disorders
l. Reactive lymphoid hyperplasia
m. Lymphoma
n. Angiolymphoid hyperplasia with eosinophilia
•
Secondary Orbital Inflammations
o. Necrotic orbital tumor
p. Orbital foreign body
q. Orbital metastases
r. Ruptured dermoid cyst
s. Mucocele
t. Orbital blood cyst
II. CASE PRESENTATIONS
CASE NUMBER 1
Clinical Presentation: Painful left eye of 15 hour duration
A 65-year old Asian female presented to ER with acute painful, swollen left eye of 15
hour duration. The patient noticed an insidious onset of discomfort in the left eye (OS)
over 3 days. The patient denied trauma or recent illness. She did not have a significant
past ocular history, and was not taking any medications. She had a clinical history of
hyperthyroidism and hypertension for which she was taking tapazole, rocaltrol, and
atenolol. The patient had emigrated from China 5 years prior to presentation. She did
not suffer from any known allergies, was a febrile and had moderate distress from pain.
Her non-corrected visual acuity was 20/50 in her right eye (OD) and 20/100 in her left
eye. The intraocular pressures were 16 (OD) and 74 (OS). The pupils were reactive in
the right eye and sluggish but reactive in her left eye. The motility was intact OD; there
were no extraocular movements OS, with a color vision of 12/12 OD; 1/12 OS and an
estimated proptosis of 5mm in her left eye. Her anterior segment exam showed an
edematous and ecchymotic left upper eyelid with some conjunctival inflammation
present. The cornea, anterior chamber, and iris were normal. A CBC w/diff lab study
was normal. She was immuno-competent; she did not have diabetes mellitus. Imaging
showed a focal soft tissue lesion involving the orbit with a characteristic and subtle focal
bony destruction.
The differential diagnosis included:
– Secondary (metastatic, contiguous spread) – Primary intracranial
Lacrimal gland tumors
Cavernous hemangioma
Inflammatory/Infectious
– Vasculitis and granulomatous (Wegener's, Sarcoid, Temporal arteritis) – Fungal (Mucormycosis, Aspergillosis) – Bacterial (sinusitis, mucocele, periostitis) – Viral (Herpes) – Acute and subacute idiopathic inflammation
Orbital pseudotumor Tolosa-Hunt syndrome
Lymphoproliferative disorder (lymphoma)
– Carotid cavernous fistula – Cavernous sinus thrombosis
Neuro-ophthalmic disorders
– Cranial nerve palsies
Thyroid eye disease.
The patient underwent an anterior orbitotomy for orbit debulking; a tissue biopsy was obtained and cultures were done.
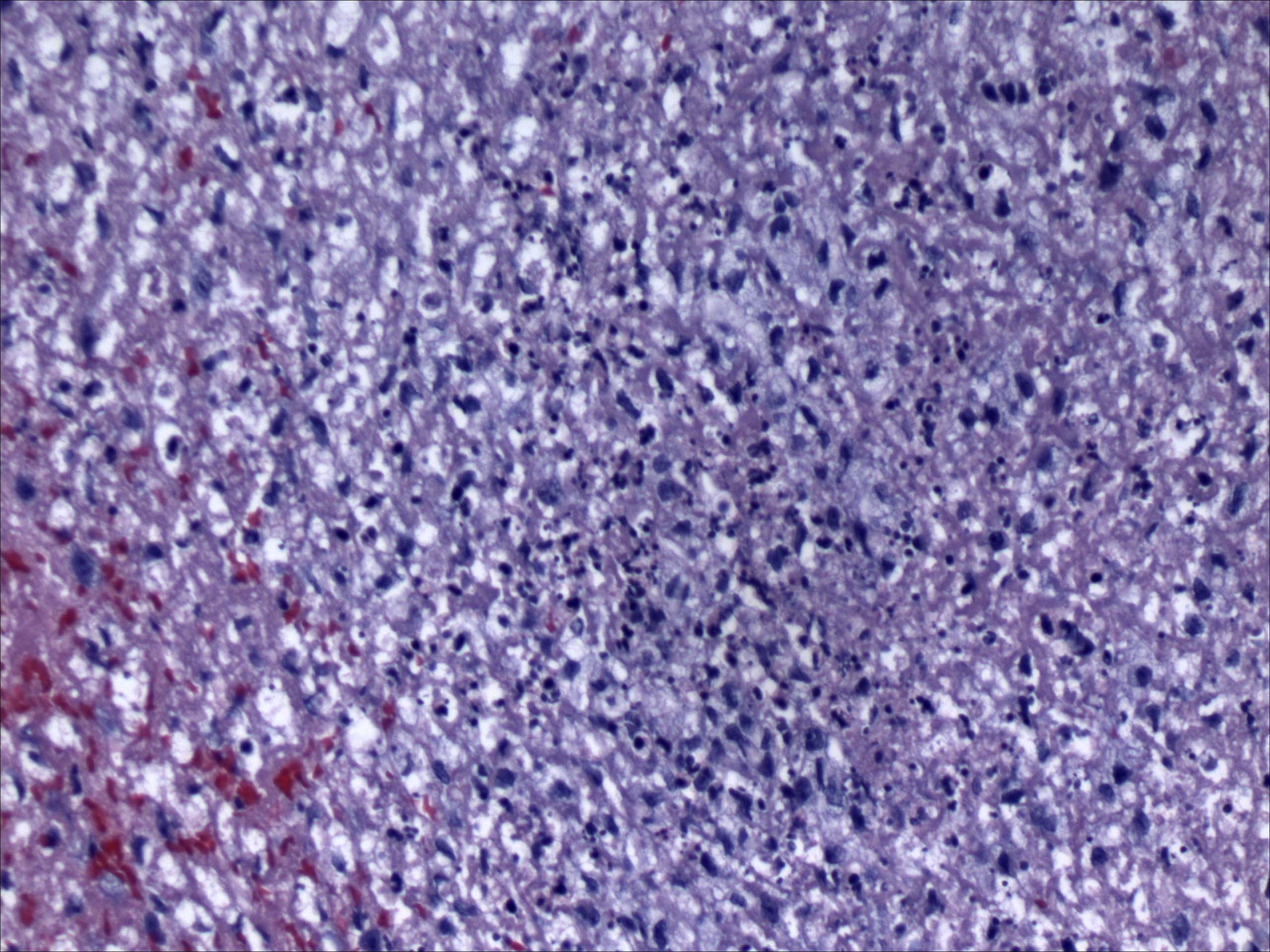
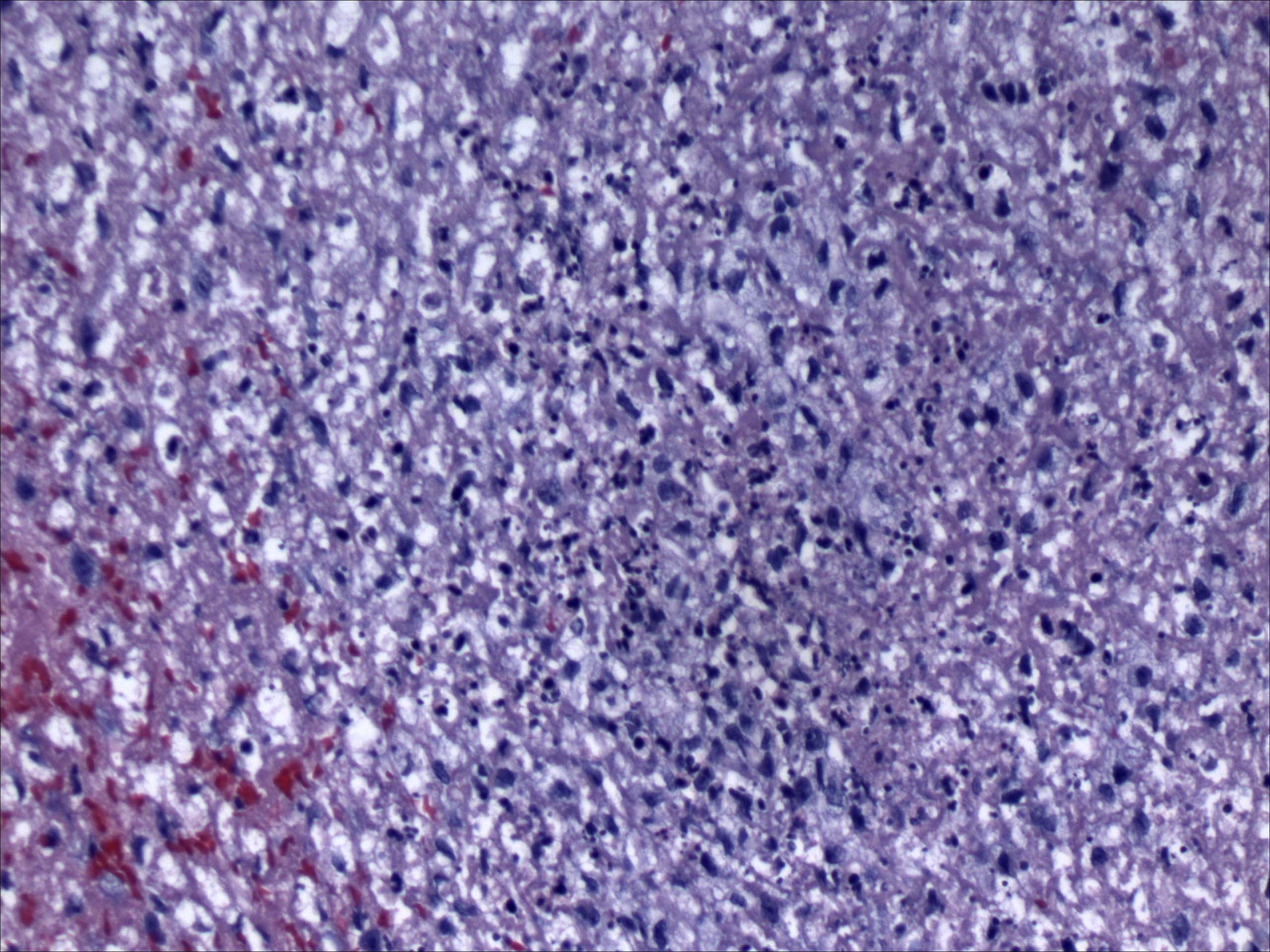
Histopathology of case number 1, H and E stain, 20 X.
CASE NUMBER 2
Clinical presentation: Worsening proptosis of 5 months duration.
A 42-year old man inpatient from the Shattuck Hospital in Boston presented with a left
eye proptosis of 4 to 5 month duration. The patient's clinical history included
schizophrenia. He denied pain. His visual acuity in the left eye was 20/200, color 0/10,
with a positive afferent papillary defect due to a compressive optic neuropathy. He had
6 mm of proptosis with a frozen globe, with no external ocular movement present.
Computed tomographic (CT) scanning showed a diffuse infiltration of the orbit, with
involvement of the optic nerve. The orbital mass showed poorly defined margins.
The differential diagnosis of this lesion included:
Metastasis, lymphoproliferative disorder
Idiopathic orbital pseudotumor
Ruptured dermoid cyst
Systemic vasculitis (Wegener's)
Infections (tuberculosis)
A diagnostic orbital biopsy was performed.
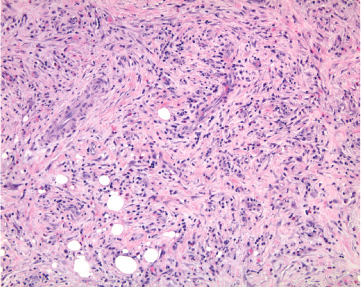
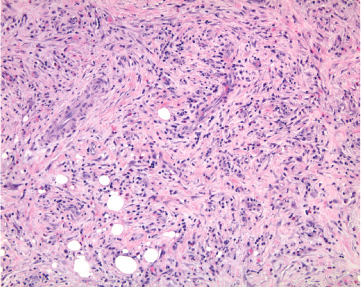
Histopathology of case number 2, H & E, 10 X
III. INFECTIOUS ORBITAL LESIONS
A. Orbital Cellulitis
The major causes of orbital cellulitis are sinusitis (58%), eyelid or face infection
(28%), foreign body (11%), and hematogenous (4%). Staphylococcus and Streptococcus are the most common causative organisms in adults, Haemophilus influenzae in children. Less common organisms are Pseudomonas and Escherichia coli. Children are affected more than adults, and in children the primary focus is generally an ethmoiditis because the ethmoid sinus pneumatizes before all of the other sinuses and has a very large ostium into the nasal cavity.
Orbital symptoms include pain, eyelid edema and erythema, chemosis, and axial
proptosis if diffuse disease occurs or abaxial displacement if an abscess forms. Decreased ocular motility is common, and intraocular pressure may be elevated. A rapid loss of vision from optic nerve compression, optic neuritis, or vasculitis may ensue. Orbital abscess (subperiosteal abscess) may occur, and is an emergency situation. Surgical drainage is often necessary (or CT-guided urgent aspiration may be employed to save vision). With posterior extension, cavernous sinus thrombosis, subdural empyema, and intracranial abscess may develop potentially causing a catastrophic event.
One third of patients with orbital cellulitis will have positive blood cultures.
Systemic symptoms may include malaise and fever. If the cavernous sinus is involved, headache, nausea, vomiting, and decreased consciousness may supervene. The warning signs of orbital cellulitis are a dilated pupil, marked ophthalmoplegia, loss of vision, afferent pupillary defect, papilledema, perivasculitis, and violaceous eyelids.
B. Fungal Infections
Two fungal infections commonly involve the orbit, usually by invasion from the
sinuses. There are the ubiquitous organisms Aspergillus and Mucor (Phycomycosis), which exist in air and soil, on skin, and as common food molds. They produce two clinical syndromes.
The first is a life-threatening infection of the sinuses involving the orbit and brain
in patients with poor controlled diabetes, or in cases of underlying systemic immuno-
compromising conditions such as leukemia, carcinomatosis, or burns. A tissue biopsy is
necessary to establish a diagnosis. Histopathology shows necrotic tissue due to
invasion of vessels by the fungus, causing infarction. The inflammatory infiltrate may be
minimal in pancytopenic patients or may consist of numerous neutrophils. The organism
may be identified by the size of the hyphae, the branching pattern and the presence of
septa. Mucor shows broad, irregularly shaped nonseptate hyphae measuring 30 to 50
um in diameter and branching at right angles. Aspergillus species are narrower,
measuring 5-10 um in diameter, they are septate, are more regular, and branch at acute
angles. Culture of the biopsy material is necessary for exact speciation. Early diagnosis
and aggressive therapy are necessary for survival.
The second infection is limited to the nose, orbit and sometimes brain in
otherwise healthy patients. In these cases, biopsy specimens show well-formed granulomatous inflammation, often with necrotizing centers surrounded by neutrophils, histiocytes, giant cells, lymphocytes and plasma cells. The organisms are usually located in the center of the granulomatous inflammation and may not be easily found requiring fungal stains for easy identification (PAS and GMS stains). Aspergillosis is the most common fungal infection of the paranasal sinuses (causes approximately 90% of the cases). The pathogenesis is related to the fungus ability to binds to laminin and fibrinogen. The treatment depends on the presence of invasion of surrounding structures; if bone or blood vessel invasion is present, the prognosis is poor with high mortality, usually 2-6 months after the initial presentation. Five of 17 reported cases in the literature of sino-orbital aspergillosis occurring in immuno-competent patients survived the infection.
Other fungi may rarely involve the orbit including Sporothrix schenckii and
Blastomyces dermatitidis among others.
C. Orbital Parasites
Many parasites may involve the orbit, but examples in North America are few and
usually occur in individuals who have lived or traveled in the Middle East, Africa, Asia, Central and South America. All of these infections require excision of the affected tissues and histopathological examination for diagnosis. Cysts due to Echinococcus Granulosus (hydatid cyst) are probably the most frequent (up to 30% of patients with proptosis in Iraq have this infection). Other cystic infections are cysticercosis, produced
by the larval stage of the pork tapeworm Taenia solium. Microfilaria of Onchocerca volvulus, Loa Loa and adult worms of Dirofilaria species have been seen in the anterior orbit. Trichinella spiralis may localize in the extraocular muscles. Eggs of Paragonimus and Schistosoma haematobium have been reported.
Histopathological evaluation shows granulomatous inflammation, with numerous
eosinophils, surrounding the residue of parasite. The Splendore-Hoeppli phenomenon
refers to radiating eosinophil deposits around helminths (or fungi), attracted by the Ag-
Ab complexes that form on the cuticular walls of these parasites.
D. Other orbital infections
Tuberculosis may rarely involve the orbit, spreading from the paranasal sinuses
or lacrimal gland or via the blood system. On histopathological examination, typical non-necrotizing granulomatous inflammation is present. A single or few acid fast positive stain bacilli may be found in most cases (if immunosuppression is present, then numerous bacilli are fouind).
Syphilitic orbital involvement is extremely rare. A syphilitic peri-ostitis with
superior orbital fissure inflammation and external ophthalmoplegia has been described.
Dacryo-adenitis are usually infectious and of viral etiology and is seen in
children and adults. The eyelid can present with erythema laterally, and a swollen "S-shaped" deformity, and lacrimal gland enlargement on CT projecting beyond the orbital rim (in contrast to epithelial tumors, which rarely project beyond rim).
Rhinoscleroma is an endemic, chronic, slowly progressive granulomatous
disease caused by Klebsiella rhinoscleromatis. The rate of occurrence is probably associated with poverty, poor hygiene, and prolonged contact with infected individuals. Rhinoscleroma is endemic in some parts of Africa, Asia, eastern Europe, South America, and Central America. The disease most frequently affects persons in the 20- to 40-year age range. The nose is the most common site of infection, although the nasopharynx, paranasal sinuses, pharynx and orbit may be involved as well. On histologic examination these masses are formed of plasma cells cells with Russell bodies and Mikulicz cells (foamy histocytes containing K. rhinoscleromatis as seen on gram stain). Treatment of rhinoscleroma is antibiotic therapy.
IV. INFLAMMATORY ORBITAL LESIONS
A. Grave's Orbitopathy / Thyroid-Related Orbitopathy (TRO)
Thyroid orbitopathy is an immunological disorder that affects the orbital muscles
and fat. Hyperthyroidism is seen with orbitopathy at some point in most patients,
although the two are commonly asynchronous. Thyroid orbitopathy is seen most
frequently in middle-aged adults (30–50 years), more commonly in women than in men
(ratio of 3–4:1); it is always a bilateral process but is often asymmetrical; and multiple
muscles are involved simultaneously, most commonly the inferior and medial rectus.
There are no known endocrinologic or immunologic parameters to predict which patients
will have ocular involvement. The disease has an immune etiology, with an anti-thyroid
immunoglobulin produced called TSI (thyroid-stimulating Ig); this immunoglobulin
interacts with the receptor on the thyroid follicular cell for TSH. The thyroid gland thereby becomes autonomous.
The systemic signs of Grave's disease include diffuse hyperplastic goiter,
tachycardia, sweating, weight loss, and pre-tibial edema. Ocular symptoms and signs include dry eyes, conjunctival injection, eyelid retraction, exophthalmos, diplopia, corneal exposure, and rarely optic nerve compression (see Table 2). Graves' disease usually runs a progressive course for 3–5 years and then stabilizes. Less than 10% of patients have evidence of infiltrative myopathy, where enlargement of the extra-ocular muscles occurs, leading to the more serious ophthalmic signs including proptosis, diplopia with extra-ocular motility imbalances, and optic nerve compression.
Orbital imaging shows increased fat lucency, as well as extraocular muscle
enlargement confined to the bellies, but with sparing of the insertions and origins. On MRI the T1 is isointense and the T2 isointense to slightly hyperintense to muscle. Thickened muscles with medium to high internal reflectivity and an irregular acoustic structure are seen on echography.
Histopathological examination shows the enlarged, rubbery muscles with variable
amounts of edema and infiltration with inflammatory round cells. An increased amount of acid mucopolysaccharides infiltrates the orbital tissue.
Symptomatic therapy is given until the disease stabilizes. Systemic
corticosteroids or radiotherapy may be indicated for acute orbital inflammation and congestion. The orbital disease is usually progressive over 1–5 years, followed by stabilization. Eyelid recession, strabismus surgery, or orbital decompression may be offered after stabilization, as needed, to improve function and cosmesis
Table 2. Werner Classification of eye changes with Grave's disease, based on the
mnemonic "no-specs"
No signs,symptoms
Only signs, no symptoms
Soft tissue involvement
Corneal involvement
B. Orbital Inflammatory Syndrome (OIS) / Idiopathic Orbital Inflammation/
Orbital Pseudotumor
Diffuse orbital pseudotumor is a nongranulomatous acute to subacute onset
inflammatory disease with no systemic manifestations that may affect teenagers to the elderly. Most commonly it occurs in the anterior or mid orbit, and it frequently involves the lacrimal gland. It is typically unilateral but rarely may be bilateral. Uveitis and retinal detachment may be associated with scleritis.
Clinical symptoms include abrupt pain, conjunctival injection, chemosis, eyelid
edema, exophthalmos, and motility restriction. A palpable mass is detected in 50% of
cases. The disease should be distinguished clinically from infectious orbital cellulitis.
In children, bilaterality is present more commonly (40%), with evidence of papillitis or
iritis. In adults, if the presentation is bilateral, a systemic disease such as lymphoma or
Wegener's should be ruled out.
On CT scan, the posterior Tenon's capsule shows thickening and enhancement.
Extra ocular muscle swelling typically extends to involve the tendons, and orbital fat shows increased intensity (either from edema or inflammatory cell infiltration). A shaggy orbital infiltrate or discrete mass is present, which may mold to the globe or optic nerve sheath. The lacrimal gland may be enlarged. On MRI the T1 signal is hypointense and the T2 signal is hyperintense to muscle. Moderate enhancement occurs with gadolinium. On echography, the lesion has a variable shape and borders, with low to medium reflectivity, a regular acoustic structure, and weak sound attenuation. Edema in Tenon's capsule may appear as an area of lucency behind the globe.
Histopathological evaluation shows widespread polymorphic infiltrate of
lymphocytes, eosinophils, plasma cells, and polymorphonuclear leukocytes involving extraocular muscles, fibro-fatty tissues and the lacrimal gland. In the sclerosing type, the dominant feature is scarring and collagen deposition. Eosinophils can be seen (and may be accompanied by peripheral blood eosinophilia, especially in children). Lymphoid follicles and germinal centers are not typically seen (more typical of Grave's Disease). As the disease progresses, there is fibrous replacement of muscles, fat, and lacrimal gland acini. In the sclerosing pseudotumor variant increased fibrosis and wall-to-wall congealing of all orbital contents leads to a "frozen orbit". If the disease is specifically localized to the apex, a Tolosa Hunt syndrome is produced, with complete painful external ophthalmoplegia.
This disease is exquisitely responsive to high dose systemic corticosteroids, and
can show remarkable clinical resolution within 48 hours. Slow taper over 4-6 weeks recommended, because rebound can occur. Intractable cases with progressive fibrosis respond less well to corticosteroids. Radiotherapy has some advocates. Prognosis generally is excellent, with complete resolution of disease.
C. Sarcoidosis
Sarcoidosis is a multi-system disease manifest in ocular adnexa, uvea, lacrimal and
salivary glands, lungs, skin etc. The disease has a predilection to involve lacrimal gland and it is a cause of acute and sub-acute lacrimal gland enlargement or inflammation. Histopathological examination shows characteristic non-necrotizing granulomatous inflammation, giant cells and a lymphoplasmacytic infiltrate. The disease is mostly bilateral, but may be asymmetric.
D. Amyloid Deposition
Amyloid deposition may be related to systemic or localized disease. If systemic, it
may be associated it with a plasma cell dyscrasia, a chronic inflammatory condition or a familiar neuropathy. Localized disease may be due to a local lymphoid proliferation, a chronic inflammatory condition or an organ-limited disease. Histopathological evaluation
of amyloid on H and E stain shows eosinophilic amorphous deposition, often situated around blood vessels. The material stains with Congo Red stain and shows apple-green dichroism under polarized light.
E. Vasculitis
a. Wegener's Granulomatosis
Wegener's granulomatosis is a necrotizing granulomatosis of the upper
respiratory tract, characterized by vasculitic pneumonitis, glomerulonephritis, sinusitis, and mucosal ulcerations of the nasopharynx. A limited form does not involve the kidney. The cause is T-cell immune complex formation secondary to inhaled antigens. The key features of this condition are a) a peak incidence in adults 40–50 years of age; b) men are more commonly affected than women, in a ratio of 2:1; c) the classic antineutrophil cytoplasmic antibody (c-ANCA) is positive in 80% of cases; d) 40–50% of patients may have ocular involvement (mostly contiguous from the sinus or pharynx, but it may be isolated); of those 18–22% of patients demonstrate orbital involvement, usually bilateral as a result of extension of the sinus process through a lytic bony lesion, or as a result of a vasculitis of the orbital vessels.
Symptoms are chemosis, exophthalmos, motility restriction, papilledema, and
decreased vision. Ocular tissue involvement may include scleritis and episcleritis (20–38%), uveitis (10–20%), peripheral corneal guttering (14–28%), and retinal vasculitis (7–18%).
The pathology is a necrotizing granulomatous vasculitis with giant cells.
However, the inflammatory infiltrate may or may not show granulomas, but mononuclear histiocytes seen (along with lymphocytes and plasma cells) with vasculitic involvement of arteries, veins and interstitial connective tissue inflammation.
The treatment consists of administration of systemic corticosteroids plus
cyclophosphamide or azathioprine. Radiotherapy is of doubtful value. Improvement with systemic therapy is usual, with up to 90% remission. Patients who have the more limited form of the disease have a better prognosis.
b. Giant Cell Temporal (Cranial) Arteritis
The clinical presentation may be varied with systemic symptoms (myalgias,
weight loss, jaw claudication, fatigue, headaches) and ophthalmic symptoms (transient
or permanent vision loss, visual field loss – AION, ophthalmoplegia).
This disease usually affects the elderly and presents with elevated ESR. The
ophthalmic artery and posterior ciliary arteries may be involved. Histopathology shows a
mononuclear cellular infiltration of all layers of the blood vessel wall with histiocytes
and/or giant cells seen at the muscularis media and internal elastic lamina. Destruction
and or loss of the internal elastic lamina, and destruction of muscularis media with
fibrosis are findings that are detectable even in healed arteritis. Inflammation in orbital
vessels is not a prominent feature of the disease.
c. Polyarteritis Nodosa
This form of vasculitis affects smaller arteries (orbital as well as other). There is
vessel wall necrosis, with numerous PMN's and eosinophils present. Usually it affects
males more than females (unusual among the auto-immune diseases). Serum p-ANCA is positive in most patients.
d. Orbital Thrombophlebitis
Elderly individuals may be affected by an inflammation centered almost
exclusively around the orbital veins. The inflammation is idiopathic or associated with a visceral malignancy (for example mucinous carcinoma), or and infection of the eyelids. It is considerably painful, with hemorrhage and suffusion of the lids and orbital contents. On histological evaluation PMN's and lymphocytes are localized to the walls of veins, causing thrombosis.
F. Benign Lympho-epithelial Lesion of Lacrimal Gland
Historically, bilateral parotid and lacrimal gland enlargement was characterized
by the term Mikulicz's disease if the enlargement appeared apart from other diseases.
If it was secondary to another disease, such as tuberculosis, sarcoidosis, lymphoma,
and Sjögren's syndrome, the term used was Mikulicz's syndrome.
The lesion occurs mostly in adult (50 years of age) females (60-80% of cases).
The lacrimal gland shows diffuse swelling that can be asymptomatic or with mild pain. Most cases of benign lymphoepithelial lesions appear in conjunction with Sjögren's syndrome. When Sjögren's syndrome is present, the swelling is usually bilateral. In most cases, a biopsy is needed to distinguish benign lymphoepithelial lesions from chronic sialadenitis.
Histopathology shows a marked lymphoplasmacytic infiltration. Lymphoid follicles
surround solid epithelial nests, giving rise to the 'epimyoepithelial islands', that are mainly composed of ductal cells with occasional myoepithelial cells. Excess hyaline basement membrane material is deposited between cells, and there is also acinar atrophy and destruction.
Treatment usually consists of surgical removal of the affected gland. Prognosis is
usually good, however occasionally this condition may evolve into lymphoma, or represent occult lymphoma from the outset.
G. Histiocytic Diseases
G. Eosinophilic Granuloma (Langerhans' Cell Histiocytosis)
Eosinophilic granuloma is the most common and benign form of the histiocytosis
X group. The disease affects primarily children and teenagers (from birth to 20 years of age). It consists of a unifocal, granulomatous proliferation in the bone. Orbital involvement occurs in up to 20% of cases, most commonly in the superotemporal orbit.
Clinically, a rapid onset of displacement of the globe occurs, and painful
superolateral swelling. Erythema and inflammatory signs are seen in the overlying skin. Unifocal disease is termed eosinophilic granuloma. Multifocal disease may present with multiple orbital lytic lesions and diabetese insipidus (Hand-Schuller-Christian disease),
and a multifocal disease with visceral, skin and nodal involvement (Letter-Siwe disease). A spectrum of these diseases used to be termed "Histiocytosis X".
Orbital imaging usually shows a lytic orbital rim lesion (near the superotemporal
bony rim), orbital extension may look pink and inflammatory. Histopathological examination shows numerous binuclear histiocytes, eosinophils, and giant cells with characteristic Langerhans' granules are seen in the cytoplasm. Immunohistochemical stains used to aid the diagnosis include CD1a stain and S100.
Surgical curettage generally is curative, but radiotherapy at 900–1500 cGy also
may be used. The prognosis is very good.
Orbital Xanthogranuloma (Erdheim-Chester Disease)
The disease is characterized by subcutaneous eyelid, anterior or posterior orbital
lesions presenting as indurated, waxy yellow, erythematous nodules. The patients are
usually in the 6th decade of life. The disease is associated with systemic disease
(plasma cell dyscrasias, multiple myeloma). On histopathology, the characteristic
Touton giant cells, and foamy lipid-laden xanthoma cells are present. Necrobiosis
(dissolution of collagen as a central nidus) may be present.
Kimura's Disease
Also called Angiolymphoid Hyperplasia with Eosinophilia is a rare disease
involving primarily the skin of head and neck. The inflammatory lesion is usually present in superior orbit, well-circumscribed but edges "trail off" into surrounding orbital connective tissue. In general blood eosinophilia or asthma is found more frequently in patients with skin involvement than with orbital disease.
H. Benign Reactive Lymphoid Hyperplasia
This disease constitutes a benign proliferation of lymphoid follicles that contain
polymorphic lymphocytes that are immunohistochemically polyclonal. Benign reactive lymphoid hyperplasia (BRLH) occurs most commonly in the anterior superior orbit, with a predilection for the lacrimal gland (15%). The clinical course is indolent, with painless exophthalmos, globe displacement, and typically normal vision. A firm, rubbery mass is often palpable beneath the orbital rim, and there may be a pink subconjunctival "salmon-patch" infiltrate. Imaging shows an infiltrative mass seen in the eyelids or anterior orbit. It typically molds to the globe and other adjacent structures and may extend along the rectus muscles. On MRI the T1 signal is hypointense and the T2 signal hyperintense to muscle. On histopathology there is typically is a polymorphous population of small lymphocytes and plasma cells, with mitotically active germinal centers. Treatment
involves systemic corticosteroids or local radiotherapy at 1500–2000 cGy. Some lesions may require cytotoxic agents (chlorambucil) for control. There is a 15–25% chance of developing systemic lymphoma within 5 years
In contrast, orbital lymphoma is usually a low-grade malignancy characterized by
a proliferation of monoclonal B cells (non-Hodgkin's). Most commonly affected is the older age group (50–70 years). Clinically, a palpable mass may be present in the
anterior orbit. Symptoms include exophthalmos, occasional diplopia, eyelid edema, and
ptosis. In 75% of cases the process is unilateral, and in 25% it is bilateral; 40% of cases
are associated with systemic disease at the time of diagnosis. Imaging shows a well-
defined mass that molds to encompass adjacent structures. Most lesions are located in
the anterior, superior, and lateral orbit and frequently involve the lacrimal gland. A
specific form of lymphoma, the MALT (mucosa-associated lymphoid tissue) lymphoma
or marginal zone lymphoma has the highest frequency of occurrence in the orbit. This
lymphoma is characterized by an extranodal location, a localized disease, and a
distinctive histopathology of lymphoplasmacytic infiltrates, foci of follicle center cell and
lympho-epithelial lesions. Most ocular adnexal lympomas are localized at presentation
and radiation therapy provides excellent local control.
V. DIAGNOSIS
Case number 1 diagnosis: Sino-Orbital Aspergillosis infection in an immuno-
competent patient.
References
Heier JS et al. Proptosis as the initial presentation of fungal sinusitis in
immunocompetent patients. Ophthalmology. 1995: 102: 713-17.
Sivak-Callcott et al. Localised invasive sino-orbital aspergillosis: characteristic features.
British Journal of Ophthalmology. 2004: 88: 681-687.
Hedges TR, Leung LE. Parasellar and orbital apex syndrome caused by aspergillosis.
Neurology. 1976: 26: 117-20.
Lee JH et al. Cavernous sinus syndrome: Clinical features and differential diagnosis with
MR imaging. American Journal of Roengenology 2003: 181: 583-90.
Rootman J. Diseases of the orbit. Lippincott. Philadelphia, 1988.
Case number 2 diagnosis: Inflammatory pseudotumor
Yan J, Wu Z, Li Y. A clinical analysis of idiopathic orbital inflammatory pseudotumor. Yan Ke Xue Bao 2000; 16(3):208-13. Weber AL, Romo LV, Sabates NR. Pseudotumor of the orbit. Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am 1999; 37(1):151-68. Mombaerts I, Goldschmeding R, Schlingemann RO, et al. What is orbital pseudotumor? Surv Ophthalmol 1996; 41(1):66-78. Wasmeier C, Pfadenhauer K, Rosler A. Idiopathic pseudotumor of the orbit and Tolosa-Hunt syndrome--are they the same disease? J Neurol 2002; 249(9):1237-41. Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol 2002; 13:347-51.
Source: http://uscapknowledgehub.org/site~/98th/pdf/companion24h02.pdf
UNIVERSIDAD DE LA REPÚBLICAFACULTAD DE ENFERMERÍA Factores que inciden en el consumo de psicofármacos en el personal de enfermería de una institución médica del interior del Uruguay Br. Alvarez, Catalina Br. Lapido, Soledad Br. Lorduguin, Florencia Br. Mantuani, Flavia M Prof. Agda. Esp. Lic. Enf. Garay, Margarita Prof. Agdo. Mg. Lic. Enf. Díaz, Álvaro
Case 1:10-cv-02902-JEI -AMD Document 50 Filed 08/25/11 Page 1 of 37 PageID: 964 UNITED STATES DISTRICT COURT DISTRICT OF NEW JERSEY TROY D., and O'NEILL S., HONORABLE JOSEPH E. IRENAS CIVIL ACTION NO. 10-2902 Bruce W. Clark, Esq. 902 Carnegie CenterSuite 500Princeton, NJ 08540 Counsel for Plaintiffs OFFICE OF THE NEW JERSEY ATTORNEY GENERALBy: Susan Marie ScottRJ Hughes Justice Complex25 Market StreetP.O. Box 112Trenton, NJ 08625