Microsoft word - titelblad_x.doc
From the Department of Orthopaedics,
Clinical Sciences Lund, Lund University, Sweden
The infected knee arthroplasty
Anna Stefánsdóttir
Anna Stefánsdóttir
List of papers, 2
Results / Summary of papers, 20
Definitions and abbreviations, 3
Introduction, 4
Historical background, 4
The Swedish Knee Arthroplasty Register, 4
Definition of infected knee arthroplasty, 4
Discussion, 25
The size of the problem, 5
Limitations of the study, 25
Classification, 6
Timing and type of infection, 25
Infecting microorganisms, 7
Antibiotic susceptibility, 26
Type of treatment, 27
The results of treatment, 27
Effects on quality of life, 11
Prognostic factors for failure to eradicate infec-
Economic impact, 12
Antibiotic prophylaxis, 12
Timing of antibiotics, 28
Other prophylactic measures, 13
Conclusions, 30
Aims of the study, 14
Populärvetenskaplig sammanfattning, 31
Patients and methods, 15
Yfirlit á íslensku, 32
Papers I–III, 15
References, 34
Original papers I–IV
THE INFECTED KNEE ARTHROPLASTY
The thesis is based on the following papers:
I. Stefánsdóttir A, Knutson K, Lidgren L, and III. Stefánsdóttir A, Knutson K, Lidgren L, and
Robertsson O. The time and type of deep
Robertsson O. 478 primary knee arthroplasties
infection after primary knee arthroplasty.
revised due to infection – a nationwide report.
II. Stefánsdóttir A, Johansson D, Knutson K, IV. Stefánsdóttir A, Robertsson O, W-Dahl A,
Lidgren L, and Robertsson O. Microbiology
Kiernan S, Gustafson P, and Lidgren L. Inad-
of the infected knee arthroplasty: Report from
equate timing of prophylactic antibiotics in
the Swedish Knee Arthroplasty Register on
orthopedic surgery. We can do better.
426 surgically revised cases.
Acta Orthopaedica 2009; 80(6): 633-8.
Scandinavian Journal of Infectious Diseases
2009; 41(11-12): 831-40.
Anna Stefánsdóttir
Definitions and abbreviations
Biofilm Organised communities of aggregated
PMMA Poly(methyl methacrylate): bone cement
bacteria embedded in a hydrated matrix of extracellular polymeric substances
Primary arthroplasty
The first time one or more joint sur-
Coagulase-negative staphylococci
faces are resurfaced with prosthetic implant(s)
Colony-forming unit. A measure of
the number of viable bacteria. In air
RA
Rheumatoid arthritis
expressed as cfu/m3
Revision arthroplasty
Cumulative revision rate
A reoperation during which prosthetic component(s) are either exchanged,
Index operation
removed, or added
First-time revision, due to an infection
Minimum inhibitory concentration: the lowest concentration of an antimi-
The Swedish Knee Arthroplasty Regis-
crobial substance that will inhibit the
visible growth of a microorganism after overnight incubation
Surgical site infection
Methicillin-resistant
Staphylococcus TKA
Tricompartmental knee arthroplasty
Unicompartmental knee arthroplasty
Polymerase chain reaction: a tech-nique for in vitro amplification of spe-cific DNA sequences from organisms, including bacteria.
THE INFECTED KNEE ARTHROPLASTY
tion after a primary knee arthroplasty that involves
addition, exchange, or removal of at least one
The development of modern knee arthroplasty prosthetic component (including arthrodesis and started in the 1940s. In 1953 Walldius, an ortho-
amputation). The reason for revision is recorded
paedic surgeon in Stockholm, described promis-
based on a report from the operating surgeon and
ing results with the use of a hinge prosthesis made information retrieved from hospital records. In a
of acrylate (Walldius 1953). Even though aseptic validity study, it was estimated that 94% of revi-
and antiseptic techniques were well implemented sions were accounted for (Robertsson et al. 1999).
at this time, infection was a significant problem.
In his series of 32 arthroplasties, performed on 26
patients, Walldius reported fatal septicaemia in 1
Definition of infected knee arthroplasty
case, amputation due to infection in 2 cases, and arthrodesis due to infection in 4 cases (Walldius No standardised criteria of infected knee arthro-1957). Sir John Charnley, the great pioneer in hip plasty are available. The finding of a microor-arthroplasty, addressed the infection problem by ganism in cultures from tissue biopsies has been developing an operating theatre with ultra-clean referred to as the gold standard (Banit et al. 2002), air and a body exhaust system. By these measures, but some authors have instead used histological the infection rate after hip arthroplasty was brought criteria of infection (Atkins et al. 1998). It is well down from more than 7% to 0.6% (Charnley 1979). known that in some cases of infected knee arthro-In the early 1970s the principles of low-friction plasty, culture fails to reveal any microorganism – arthroplasty were applied to the knee joint (Insall and the possibility of false-positive cultures must et al. 1976), and with continuing development knee also be considered. In clinical practice, the diag-arthroplasty has become a routine operation that is nosis of infection is made by sound interpretation performed on a large scale throughout the industr-
of medical history, clinical signs, laboratory tests,
diagnostic imaging, microbiology, and macro-scopic findings during surgery.
A clear distinction has to be made between a
superficial infection and an infection located within
The Swedish Knee Arthroplasty Register
the joint capsule, involving the prosthetic implant.
The Swedish Knee Arthroplasty Register (SKAR) An anatomy-based nomenclature scheme of noso-was established in 1975 by the Swedish Ortho-
comial surgical site infections (SSIs) was presented
paedic Society, and it was the first national arthro-
by the Centers for Disease Control (CDC) in 1992
plasty register. The main aims were to give early (Horan et al. 1992), and this is now widely used warning of inferior designs and to present aver-
for surveillance (Morgan et al. 2005, Barnes et al.
age results based on the experience of a whole 2006). According to this scheme, SSIs are divided nation instead of that of highly specialised units into incisional SSIs and organ/space SSIs. Inci- (Robertsson et al. 2000b). Currently there are 76 sional SSIs are further classified as involving only orthopaedics departments in Sweden that perform the skin and subcutaneous tissue (superficial inci-knee arthroplasties, and all report to the register. sional SSIs) or involving deep soft tissues (i.e. fas-In September 2010, the database contained infor-
cial and muscle layers) of the incision (deep inci-
mation on 165,000 primary knee arthroplasties and sional SSIs). To be classified as an organ/space SSI, 12,450 revision knee arthroplasties. The main out-
the infection has to occur within 1 year of implanta-
come variable reported by the register is revision tion and it should appear to be related to the pro-arthroplasty, which is defined as any later opera-
cedure (Horan et al. 1992). In the case of infected
Anna Stefánsdóttir
Yearly number of knee arthroplasties
n = 12,129
n = 20,349
n = 34,224
n = 28,441
ight 2010 SKARyr
ight 2010 SKARyr
Year of operation
Year after index operation
Figure 1. The annual number of arthroplasties for dif-
Figure 2. The CRR because of infection in OA patients
ferent diagnoses registered in the SKAR. From the
undergoing primary TKA during different time periods.
SKAR Annual report 2010, available at www.knee.se.
From the SKAR Annual report 2010, available at www.
knee.se.
knee arthroplasty this nomenclature is confusing, 5 years (Furnes et al. 2002). In Finland data from as the largest part of the incision does not involve the Finnish Hospital Infection Program, the Finn-any muscle layer. In practice, there will be two ish Arthroplasty Register, and the Finnish Patient classes: (1) superficial incisional SSI (involving Insurance Center were cross-matched and the skin and subcutaneous tissue), and (2) organ/space infection rate for 5,921 cases of TKA performed SSI (involving the joint, with the joint capsule as a during 1999–2004 was estimated to be 1.3% (Huo-natural boundary). In this work the organ/space SSI tari et al. 2010). In the USA, the risk of infection is termed infected knee arthroplasty.
after TKA was reported to be 1.55% within 2 years in 69,663 patients in the Medicare population, the infections being identified by ICD-9 codes (Kurtz et al. 2010). In that study, patients undergoing
The size of the problem
TKA because of a bone cancer, a fracture, or joint
Despite the large number of operations performed infection were excluded, as were patients younger each year, it is difficult to obtain reliable informa-
tion on the incidence of infected knee arthroplasty.
With the increasing number of primary knee
The national arthroplasty registers provide some arthroplasties (Figure 1), the number of infected information, but it must be remembered that there cases will increase. It has been predicted that can be methodological differences between reg-
infection will become the most frequent mode of
isters. Of the 34,701 primary knee arthroplasties failure of total knee arthroplasty, with great eco-(both total knee arthroplasty (TKA) and unicom-
nomic consequences (Kurtz et al. 2007). In Den-
partmental knee arthroplasty (UKA)) reported to mark in 2008, infection was reported to be the the SKAR during 1999–2003, 0.65% were revised most common reason for revision (32.1%) (DKR due to infection within 5 years. 29,928 were pri-
2009), and in Australia in 17.1% of cases (AOAN-
mary TKAs and 0.70% of them were revised JRR 2009). In Sweden and in England, in 2009, because of infection within 5 years (personal infection was reported to be the cause of revision in information from the SKAR, September 2010). 23% of cases (NJR 2010, SKAR 2010).
Of 6,133 cemented TKAs reported to the Nor-
Data from the SKAR has been used to calculate
wegian arthroplasty register during 1994–2000, the cumulative revision rate (CRR) due to infection 0.44% were revised because of infection within in OA patients undergoing TKA (Figure 2). The
THE INFECTED KNEE ARTHROPLASTY
CRR due to infection decreased during the first time periods studied, but there was a slight increase in CRR in patients operated during the years 2006–2008, compared to those operated during the years 2001–2005.
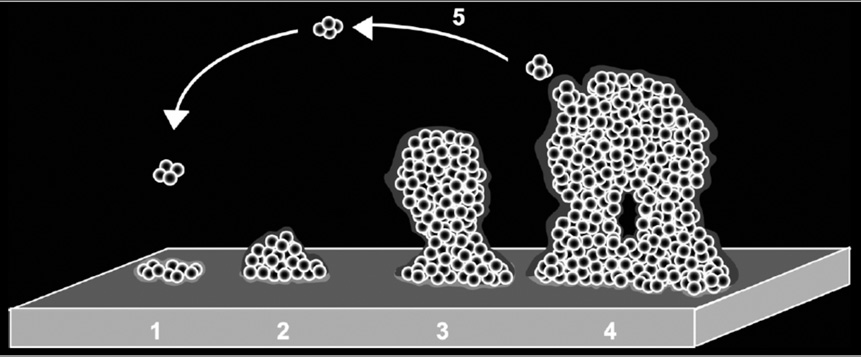
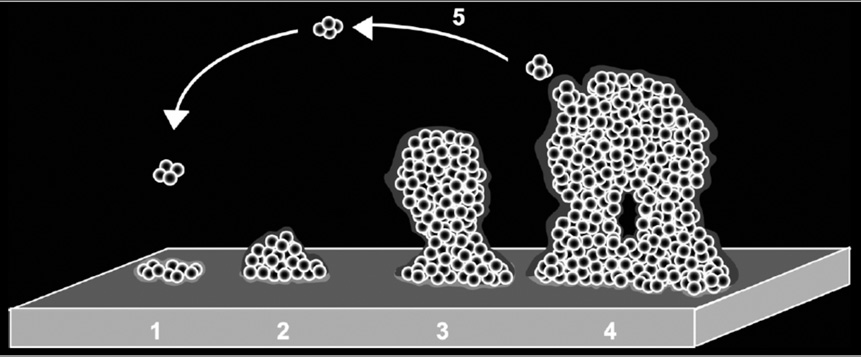
Figure 3. The development of a biofilm, depicted as a five-stage process. Stage 1: initial attachment of cells to
There is no consensus on a classification system
the surface; stage 2: production of extracellular poly-
for infected arthroplasties.
meric substances; stage 3: early development of biofilm architecture; stage 4: maturation of biofilm architec-
Zimmerli and co-workers have suggested that
ture; stage 5: dispersion of bacterial cells from the bio-
prosthetic joint infections should be classified
film. From: Lasa I. International Microbiology 2006; 9:
as three types: early, delayed, and late infections
21–28. Published with permission.
depending on the time of appearance of the first
signs and symptoms of infection (Zimmerli and (chronic) infections. This classification has been
Ochsner 2003). According to this scheme, early used in a staging system that has been shown to be
infections present during the first 3 months after predictive of outcome when treating infected knee
surgery, delayed infections present between 3 arthroplasties (McPherson et al. 1999, Cierny and
months and 2 years, and late infections present 2 DiPasquale 2002).
years or more after the arthroplasty. The late infec-
tions may appear either with a sudden systemic
inflammatory response syndrome or without initial Pathogenesis
signs of sepsis, with a delayed course after a clini-cally unrecognised bacteraemia. This classification How do bacteria aggregate in a biofilm and how do scheme highlights the pathogenesis and the pre-
they live in it? The answers to these questions are
sumed fact that most infections diagnosed within central to our understanding of the pathogenesis 2 years after primary arthroplasty are acquired of infected knee arthroplasty. A biofilm is defined during the perioperative period.
as an organised community of aggregated bacte-
A classification system meant to be of assistance ria embedded in a hydrated matrix of extracellular
when selecting treatment was presented by Segawa polymeric substances (Hall-Stoodley and Stoodley and co-workers (Segawa et al. 1999), who defined 2009). Biofilms can be formed by most, if not all, an early postoperative infection as a wound infec-
microorganisms and today the biofilm mode of life
tion (superficial or deep) that develops less than is regarded as the rule rather than the exception four weeks after the index operation. They defined (Jefferson 2004, Lewis 2007, Coenye and Nelis a late chronic infection as one that develops four 2010).
weeks or more after the index operation and has
Biofilm formation is a multi-stage process (von
an insidious clinical presentation. They defined an Eiff et al. 2002) that starts with attachment of bac-acute haematogenous infection as one that is asso-
teria to the implant surface. At the same time, the
ciated with a documented or suspected anteced-
implant is coated with proteins from the host, with
ent bactaeremia and that is characterised by acute which the bacteria can attach by specific surface onset of symptoms. In addition, they defined a sep-
proteins. The next step is proliferation and accu-
arate group of infections: those that are clinically mulation in multi-layered cell clusters, which are inapparent but where there are at least 2 positive embedded in extracellular polymeric substances cultures from specimens obtained at the time of a (containing polysaccharides, proteins, and DNA). presumed aseptic revision (Segawa et al. 1999). An As the biofilm matures, focal areas may dissolve attempt at debridement with salvage of the pros-
and the liberated bacterial cells can spread to
thesis was recommended in early postoperative another location where new biofilms can be formed infections, and removal of the prosthesis in late (Lasa 2006, Hoiby et al. 2010) (Figure 3). Bacte-
Anna Stefánsdóttir
had on the rate of infection emphasises the impor-tance of intra-operative contamination (Lidwell et al. 1987).
Bacteria are responsible for the vast majority of knee arthroplasty infections, with occasional infec-
Figure 4. Model of biofilm resistance. An initial treat-
tions caused by fungi – most commonly a member
ment with antibiotic kills planktonic bacterial cells
of the genus Candida (Hennessy 1996). The bacte-
and the majority of bacterial cells in the biofilm. The immune system kills planktonic persisters but the bio-
ria most commonly found in infected knee arthro-
film persister cells are protected from the host defenses
plasties are Staphylococcus aureus (S. aureus) and
by the exoplysaccharide matrix. After the antibiotic
coagulase-negative staphylococci (CNS), of which
concentration drops, persisters resurrect the biofilm and the infection relapses. From: Lewis. Antimicrobial
Staphylococcus epidermidis in this context is the
Agents and Chemotherapy 2001; 45(4): 999–1007. Pub-
most important species.
lished with permission.
It has been stated that early infections are caused
by virulent microorganisms such as S. aureus and
rial cells embedded in the biofilm communicate Gram-negative bacteria, whereas delayed (low-with each other and show a coordinated group grade) infections are caused by less virulent micro-behaviour mediated by a process called quorum organisms such as CNS and Propionibacterium sensing (Coenye and Nelis 2010).
acnes (Kamme et al. 1974, Zimmerli et al. 2004).
The extracellular polymeric substances protect
the bacteria from the host's immune cells and
restrict the diffusion of antimicrobials into the Risk factors
biofilm. Bacteria in the deeper layers of a thick biofilm have less access to nutrients and will grow Men have a higher risk of revision because of more slowly, which reduces the effect of antibi-
infection than women (Figure 5a) (Robertsson et
otics active against proliferating bacteria. A sub-
al. 2001, Furnes et al. 2002, Jämsen et al. 2009a),
population of the bacteria in the biofilm is named but the reason for this is unknown.
persisters, which are bacteria that are highly toler-
Rheumatoid patients have a higher risk of revi-
ant to antibiotics – even those active against slowly sion because of infection than OA patients (Figure growing bacteria – and when the antibiotic concen-
5b) (Robertsson et al. 2001, Schrama et al. 2010).
tration drops, the persisters resurrect the biofilm The reason for this may be related to the disease and there is relapse of infection (Figure 4) (Lewis and to the anti-rheumatic treatment. Glucocorti-2001, Lewis 2007).
coid agents are known to increase the risk of infec-
To start biofilm formation, bacteria must have tion (Bernatsky et al. 2007) whereas the effect of
access to the joint and there are several possible the new biological anti-rheumatic drugs on the routes of entry. Bacteria, either from the patient's incidence of infection following orthopaedic sur-skin or from the surroundings, can contaminate the gery has not been clarified (Giles et al. 2006, den joint at the time of surgery. Bacteria can also gain Broeder et al. 2007). access to the joint from an adjacent infection, either
Primary UKAs have a lower risk of revision
a postoperative superficial SSI or a later abscess because of infection than TKA (Figure 5c). around the knee joint. They can spread haematog-
Obesity is a growing problem in many parts of
enously from a distant focus, and finally, they can the world, and at least in the USA the mean BMI spread as an iatrogenic infection in conjunction of patients undergoing knee arthroplasty is rising with arthrocentesis, arthroscopy, or surgical inter-
(Fehring et al. 2007). In a study in which more
vention in the joint. The effect that the introduction than half of the patients had a BMI of ≥ 30 kg/of ultra-clean air and prophylactic antibiotics has m2, obesity was a risk factor for infection (Namba
THE INFECTED KNEE ARTHROPLASTY
n = 27,435
n = 43,742
ight 2010 SKAR
ight 2010 SKAR
ight 2010 SKAR
Year after index operation
Year after index operation
Year after index operation
Figure 5. Using the endpoint "revision for infection", the CRR (1999–2008) shows in TKA for OA that men are more affected than women (RR = 2.0). The same tendency is true for RA, although not statistically significant. UKA with its smaller implant size does better than the larger TKA, but even in UKA men have 2.9 times the risk of women of becoming revised for infection. In TKA, patients with RA are more affected than those with OA (RR = 1.7). From the SKAR Annual report 2010, available at www.knee.se.
et al. 2005). Obese patients often have other co-morbidities such as diabetes, which increases the risk of infection (Dowsey and Choong 2009). Pre-operative hyperglycaemia has recently been shown to be predictive of infection after a primary knee arthroplasty (Jämsen et al. 2010).
Smoking may increase the risk of SSI (Mangram
et al. 1999). In an interventional study, wound-related complications were found to be less fre-quent in the group of patients who had smoking intervention 6–8 weeks before scheduled hip or knee arthroplasty (Møller et al. 2002).
The risk of infection is increased in revision sur-
gery, when constrained or hinged prostheses are used, and when there is a history of earlier fracture in the joint (Jämsen et al. 2009a).
Figure 6. A 59-year-old man with OA attended hospi-
Post-operative wound complications are a strong tal with fever (38°C) and a painful knee 14 days after
predictor of later diagnosis of infected arthro-
undergoing primary knee arthroplasty. Open debride-
plasty (Wymenga et al. 1992b, Berbari et al. 1998, ment was performed, and methicillin sensitive S. aureus
was cultured from 5 out of 5 tissue biopsies. Antibiotic
Jämsen et al. 2009a). It appears likely that many of treatment started with i.v. cloxacillin, followed by p.o. these presumed superficial SSIs and wound com-
ciprofloxacin and rifampicin. The infection could be
plications were actually deep infections.
eradicated and the implant retained. Published with permission from Bertil Christenson.
the degree of suspicion. In delayed and late infec-
tions, pain and/or stiffness may be the predominant
There is a large variation in the symptoms and complaint, often in conjunction with mild to mod-signs of infected knee arthroplasty, depending on erate effusion in the joint. the type of infection, the infecting microorganism,
The laboratory tests found to be of value are
and the immunological status of the patient (Fig-
C-reactive protein (CRP) and erythrocyte sedi-
ures 6 and 7). The presence of – or a history of mentation rate (ESR) (Sanzén and Carlsson 1989, – post-operative wound complication should raise Parvizi et al. 2008a). There is a normal rise in CRP
Anna Stefánsdóttir
Figure 7. A 66-year-old woman with RA was treated with glucocorticoid, metho-trexate, and remicade, and on the third day after undergoing primary knee arthroplasty she received p.o. flucloxacillin due to discharge from the wound. She attended hospital at day 16 (picture) because of continued discharge. Open debridement was performed, and methicillin resistant CNS was cultured in 5 out of 5 tissue biopsies. Antibiotic treatment started with i.v. vancomycin, followed by p.o. clindamycin and rifampicin. The infection could be eradicated and the implant retained.
in conjunction with surgery, with a peak on the prosthetic joint infection were found to be 1.1 × second day (White et al. 1998), and near normali-
109/L for fluid leukocyte count and 64% for neu-
sation at the end of the second week (Niskanen et trophil differential; when combined with CRP and al. 1996). The level of synovial fluid IL-1 and IL-6 ESR, infection could safely be excluded or con-has recently been shown to differentiate patients firmed (Parvizi et al. 2008a).
with periprosthetic infection from patients with
The sensitivity of synovial fluid culture has
aseptic diagnosis (Deirmengian et al. 2010).
varied between 50% and 100% in different studies
Plain radiographs are necessary to visualise (Meermans and Haddad 2010). Blood culture bot-
the state of the implant, and to look for signs of tles are recommended (Font-Vizcarra et al. 2010), periprosthetic bone destruction and loosening. and in the case of small amounts of fluid gained, a Radionuclide imaging has been found to be help-
paediatric bottle can be used (Hughes et al. 2001).
ful when differentiating between delayed or late
In 1981, Kamme and Lindberg reported their
infection and aseptic loosening, the combined leu-
experience with culture of biopsy samples, col-
kocyte/marrow imaging being the recommended lected during revision hip arthroplasty, and rec-procedure (Love et al. 2009). The role of CT and ommended that five separate biopsy samples be MRI has been limited due to metal artefacts, but taken (Kamme and Lindberg 1981). Other authors with technological advances these techniques may have come to the same conclusion (Atkins et al. become useful (Sofka et al. 2006).
Analysis of synovial fluid is an essential part of
With the polymerase chain reaction (PCR) tech-
investigation, and leukocyte differential of > 65% nique, bacteria can be identified by amplification neutrophils (or a leukocyte count of > 1.7 × 109/L) of bacterial DNA containing the 16S rRNA gene. has been found to be a sensitive and specific test Despite interesting reports during the 1990s (Mari-for the diagnosis of prosthetic knee infection in ani et al. 1996, Tunney et al. 1999), the technique patients without underlying inflammatory joint still has a limited role in diagnosing infected knee disease (Trampuz et al. 2004). In another study, the arthroplasty (De Man et al. 2009, Del Pozo and cut-off values for optimal accuracy in diagnosis of Patel 2009) .
THE INFECTED KNEE ARTHROPLASTY
Intraoperative gram staining has repeatedly been treatment failure compared to debridement within
shown to lack sensitivity and is not recommended 2 days of onset (Brandt et al. 1997). Better results (Morgan et al. 2009).
have been reported when rifampcicin (which inhib-
Histology has been considered to be the most its bacterial RNA polymerase) has been included
reliable method in diagnosing arthroplasty infec-
in the antibiotic treatment used in conjunction
tion (Atkins et al. 1998), but it is not standardised with debridment of a stable implant (Zimmerli et and the inter-observer variability is high (Zimmerli al. 1998, Berdal et al. 2005, Soriano et al. 2006, et al. 2004).
Aboltins et al. 2007), but it is still not clear for
The American Academy of Orthopaedic Sur-
how long after surgery this strategy can be used.
geons has recently published extensive guidelines In the study by Zimmerli and co-workers, the long-for the diagnosis of periprosthetic joint infections est duration of symptoms was 21 days whereas in of the hip and knee (AAOS 2010).
the other studies the protocol allowed inclusion of infections diagnosed within 3 months.
Revision arthroplasty can be performed in one
or two stages. In a review paper published in 2009,
Treatment
Jämsen and co-workers summarised the results
Successful treatment of infected knee arthroplasty of one- and two-stage revision arthroplasties and involves eradication of the infection along with found that the overall success rate in eradication preservation of function in a pain-free knee joint. of infection was 73–100% after one-stage revision This may be achieved by early debridement with and 82–100% after two-stage revision (Jämsen retention of the implant or revision arthroplasty et al. 2009b). Comparison of the two methods is, in one or two stages. In certain circumstances, the however, difficult due to differences in selection.
treatment is limited to limb saving, with an arthro-
Two-stage revision arthroplasty may also be per-
desis or extraction of the implant as options, and formed in different ways. Initially, the joint was under exceptional circumstances the only alterna-
left empty during the interval between stage one
tive is above-the-knee amputation. There are cases and stage two (Insall et al. 1983). Beads made of in which suppressive antibiotic treatment is used to antibiotic-loaded bone cement were then intro-maintain function in a chronically infected joint.
duced, which allowed local administration of
Algorithms have been developed to be of help antibiotics in the joint (Borden and Gearen 1987).
when choosing treatment (Zimmerli et al. 2004), With the use of a spacer block, made of antibiotic-and favourable outcome has been coupled to adher-
loaded bone cement, it was possible to preserve the
ence to the algorithm (Laffer et al. 2006).
length of the leg, prevent adhesion of the patella
Debridement involves arthrotomy, removal of all to the femur, and thereby make stage two easier to
debris and inflamed synovial membranes, if pos-
perform (Cohen et al. 1988). An articulating spacer
sible exchange of the tibial insert (which makes (Figure 8), with separate tibial and femoral com-access to the posterior part of the joint possible) ponents, probably gives better patient comfort and and lavage with a large amount of fluid. The prob-
the range of motion after stage two may become
ability of eradicating the infection is related to better (Hofmann et al. 1995, Fehring et al. 2000, the time the biofilm has had to establish itself and Jämsen et al. 2009b). mature. It is still not clear what cases it would be
Arthrodesis can be performed in one or two
reasonable to try to treat with debridement. A dura-
stages. During the time of healing, it can be fix-
tion of less than 4 weeks has been recommended ated using either external or internal fixation, an as a time limit (Schoifet and Morrey 1990, Segawa intramedullary rod being the most common type et al. 1999), whereas in other studies the limit has of internal fixation (Knutson et al. 1984, Conway been set at 2 weeks (Borden and Gearen 1987, et al. 2004). Better results, with respect to eradica-Teeny et al. 1990, Burger et al. 1991, Wasielewski tion of infection, have been reported with the use et al. 1996). It has even been reported that debride-
of external fixation (Figure 9) whereas the rate of
ment more than 2 days after the onset of symptoms healing of the arthrodesis is higher with the use of may be associated with a higher probability of an intramedullary rod (Mabry et al. 2007).





Anna Stefánsdóttir
Figure 8. A 77-year-old man with OA who had an early infection with methicillin-resis-tant CNS after a primary knee arthroplasty. Open debridement failed, and radiographs at 7 weeks after primary surgery revealed periprosthetic bone destruction (see above). He went through a two-stage revision with the use of an articulating spacer made of vancomycin- and gentamicin-loaded bone cement. During the interval between stage 1 and 2, the antibiotic treatment consisted of i.v. vancomycin, followed by p.o. line-zolid. The infection was eradicated.
Above-the-knee amputation may be the only
alternative in the case of life-threatening sepsis or uncontrollable infection. Vascular disease in con-junction with infection may also lead to amputa-tion. High mortality and poor functional result have been reported (Fedorka et al. 2010).
Suppressive antibiotic is an alternative for patients
with chronic infection caused by a micro organism that can be suppressed with oral antibiotic(s), which can be given for long time without severe adverse effects (Segreti et al. 1998).
Effects on quality of life
Figure 9. An 86 year-old-man with RA who fell and sus-tained a rupture of the patellar ligament twelve days
Surprisingly little information is available on the
after a primary knee arthroplasty. The joint became
effect that infected knee arthroplasty has on qual-
infected with 3 kinds of bacteria (S. aureus, Proteus vul-garis, and a Haemophilus species). Due to lack of a func-
ity of life. When compared with patients with
tioning extensor mechanism, arthrodesis was chosen as
uncomplicated total joint arthroplasty, patients with
treatment with double Orthofix instruments used for
infection scored significantly lower in satisfaction
external fixation. The patient died of cerebrovascular disease, before healing of the arthrodesis.
(visual analogue scale), WOMAC, AQoL, and all aspects of SF-36 other than general health and role limitations–emotional (Cahill et al. 2008). In a
Extraction, or excision arthroplasty, can be con-
study in which 26 cases that were revised because
sidered in exceptional cases but it leaves the joint of infection were compared with 92 cases that were unstable and it is not certain that infection can be revised for reasons other than infection, the objec-eradicated by extraction of the prosthesis.
tive results after septic revision were inferior to the
THE INFECTED KNEE ARTHROPLASTY
Distribution of satisfaction, percent
are in line with an earlier study from the US where
surgical treatment of the infected total knee implant
required 3–4 times the resources of the hospital
and the surgeon compared to a primary TKA, and
approximately twice the resources of a non-septic
revision arthroplasty (Hebert et al. 1996).
Apart from the direct costs related to hospitalisa-
tion, there are considerable indirect costs related to
home care, nursing facilities, and antibiotics.
Figure 10. Results from a postal survey in 1997,
The goal of antimicrobial prophylaxis is to achieve
answered by patients who had undergone primary knee arthroplasty in the period 1981–1995 (Roberts-
serum and tissue drug levels that exceed – for the
son et al. 2000a). Of the revised cases, 47% of 232
duration of the operation – the minimum inhibitory
patients who had revision for infection and 61% of
concentrations (MICs) for the organisms likely to
1,865 patients who had revision for other reasons were satisfied or very satisfied.
be encountered during the operation (Bratzler and Houck 2004).
results after aseptic revision in terms of Knee Soci-
The first study published on prophylactic anti-
ety clinical score, function score, range of motion, biotics in joint replacements came from Sweden and return to activities of daily living (Barrack et (Ericson et al. 1973). The effect of cloxacillin as al. 2000). In a study from the SKAR, 47% of those prophylactic antibiotic in hip surgery was com-revised because of infection were satisfied or very pared with a placebo, and in the treatment group satisfied, compared to 61% of those revised for there were no infections in 83 patients after 6 other reasons (Figure 10) (Robertsson et al. 2000a).
months of follow-up whereas there were 12 infec-tions in the placebo group (8 superficial and 4 deep infections) (p < 0.001). A larger study with a longer follow-up confirmed the results and showed
a lower rate of infection in the treatment group,
In the USA the costs of prosthetic joint infections even after a follow-up of more than 2 years (Carls-during the years 1997–2004 have been analysed, son et al. 1977). The effect of the first-generation based on information from the National Hospital cephalosporin cefazolin was proven in a multi-Discharge Survey. The annual adjusted diagnos-
centre study performed in France during the period
tic-related group (DRG) cost for such infection 1975–1978 (Hill et al. 1981).
increased from $195 million to $283 million during
In a comparison between beta-lactam penicillin
these years, whereas the mean DRG reimburse-
and a first-generation cephalosporin as a prophy-
ment per hospitalisation of $9,034 did not change laxis in hip arthroplasty, there was no difference (Hellmann et al. 2010).
found between the groups (Pollard et al. 1979).
In another study from the USA, based on the In this study, flucloxacillin was given intrave-
Nationwide Inpatient Sample (NIS) database, the nously for 24 hours followed by oral medication average total charge for those having a primary for 14 days, whereas cephaloridine was given as knee arthroplasty without an infection was $35,320 3 intravenous doses over the first 12 hours, and whereas the average total charge for those with the authors concluded that the simplicity of the infection was $63,705 (Kurtz et al. 2008). In a 3-g cephaloridine regime was an advantage. Beta-single-centre study, also from the USA, the mean lactam penicillin and a first-generation cepha-charge for infected revision TKA was $109,805 losporin were compared in another study using the whereas the mean charges for aseptic revision TKA same dosage scheme for both types of antibiotics was $55,911 (Lavernia et al. 2006). These figures (1 g × 3) (Van Meirhaeghe et al. 1989). There was
Anna Stefánsdóttir
no significant difference in infection rate between effect of antibiotic-loaded cement has been stud-the study groups, but the groups were heterogene-
ied more thoroughly in primary hip replacement,
ous and the study lacked power.
where there has been convincing evidence of a
There is now a general consensus that the length reduced number of infections from using antibi-
of antibiotic prophylaxis should not exceed 24 otic-loaded bone cement (Engesaeter et al. 2003,
hours, but how many doses should be given has not Parvizi et al. 2008b).
been clarified. In a multi-centre study in the Neth-
erlands, a one-dose regime with the second-gen-
eration cephalosporin cefuroxime was compared Other prophylactic measures
to 3 separate doses in patients undergoing a total hip replacement, hemiarthroplasty of the hip, or In the 1960s and early 1970s antibiotics were total knee replacement (Wymenga et al. 1992a). In seen as an alternative to ultra-clean air as opera-the one-dose group, the infection rate was 0.83% tion boxes were not widely available. By combin-(11/1,324) and in the 3-dose group it was 0.45% ing ultra-clean air and antibiotics the incidence of (6/1,327), but the difference was not statistically sepsis after surgery was much less than that when significant (p = 0.17). The authors concluded that either was used alone (Lidwell et al. 1987). With a 3-dose regimen of cefuroxime was to be recom-
the low infection rates of today, it is extremely dif-
mended until further data became available.
ficult to prove (or disprove) the effect of a single
In a study from the Norwegian Arthroplasty Reg-
specific change in prophylactic measures by meas-
ister, it was shown that the risk of revision for any uring infection rate. In the operating theatre, cfu/reason was higher when one dose of antibiotic (as m3 is used as a measure of the quality of the air, compared to 4 doses) was given within 24 hours, and this value should be less than 10. whereas there was no significant difference in the
A shower with chlorhexidine solution has been
risk of revision between administration of 3 and shown to effectively decrease bacterial counts on 4 doses within 24 hours. When the endpoint was the skin (Byrne et al. 1991), and in Sweden at revision due to infection, no statistically significant least two preoperative chlorhexidine showers are difference was found (Engesaeter et al. 2003).
routine before knee arthroplasty surgery. It has,
The timing of the pre-operative antibiotic proph-
however, not been proven that this routine reduces
ylaxis is important (van Kasteren et al. 2007), the number of infections. In a recent study, pre-especially when a tourniquet is used (Tomita and operative screening to identify nasal carriers of S. Motokawa 2007).
aureus and subsequent treatment with nasal mupi-
The risk of haematogenous infection in conjunc-
rocin and chlorhexidine soap reduced the number
tion with dental procedures has been debated, but of infections (Bode et al. 2010). Other studies have it is now clearly understood that antibiotic prophy-
shown that in people who are nasal carriers of S.
laxis is not needed for all patients with total joint aureus, the use of mupirocin ointment results in a replacement prior to dental procedure (Berbari et statistically significant reduction in S. aureus infec-al. 2010, Zimmerli and Sendi 2010).
tions (van Rijen et al. 2008), but possible resist-ance to mupirocin has to be monitored (Caffrey et al. 2010).
Other prophylactic measures include optimisa-
Bone cement
tion of the patient's condition prior to operation,
The Australian arthroplasty register reported a minimising the length of stay at the hospital prior lower rate of revision due to infection when anti-
to operation, and strict addiction to hygiene rou-
biotic cement was used (0.67%) than when plain tines.
cement was used (0.91%) (AOANJRR 2009). The
THE INFECTED KNEE ARTHROPLASTY
Aims of the study
The aims of the study were:
1. to determine the timing and type of deep infec-
4. to evaluate the results of surgical treatment of
tion after a primary knee arthroplasty, and to
infected knee arthroplasty, and identify possi-
evaluate the most commonly used classifica-
ble factors that may be predictive of the out-
2. to determine the microbiology of surgically 5. to study the timing of administration of the first
revised infected primary knee arthroplasty
dose of prophylactic antibiotics in orthopaedic
and the antibiotic susceptibility patterns of the
pathogens isolated;
3. to determine what type of surgical treatment
Swedish orthopedic surgeons have used for infected knee arthroplasty;
Anna Stefánsdóttir
Patients and methods
primary knee arthroplasties
revised due to infection
281 knees/279 patients
Paper I and III
197 knees/193 patients
n = 478 (472 patients)
mean age at primary op. 68 (14–88)mean age at index op.
244 knees/242 patients
182 knees/179 patients
n = 426 (421 patients)
mean age at primary op. 68 (14–88)mean age at index op.
176 knees/patients
115 knees/patients
mean age at primary op. 70 (43–90)
74 operations/patients
40 operations/patients
mean age at primary op. 77 (26–96)
Figure 11. An overview of patient allocation.
and the results of treatment was gathered retro-
spectively from patient records, operation reports,
Patients who were included. Patients who had and culture reports which were requested from the
their primary knee arthroplasty revised for the involved orthopaedics departments and microbiol-
first time during the years 1986–2000, due to deep ogy laboratories involved.
infection, were included in the studies. No criteria
Patients who were excluded. Of the 526 revi-
had to be fulfilled other than that the treating sur-
sions, 48 knees (9.1%) were excluded. In 22 cases,
geon had diagnosed the knee as being infected at the operating surgeon at the time of surgery sus-the time of revision. This first revision was defined pected infection and, based on this report, the as the index operation. In December, 2003, the reason for revision was registered to be infection. SKAR was searched for cases fulfilling this crite-
A review of the medical records showed that infec-
rion and 526 cases were identified. During the study tion could not be verified. Seven cases of debride-period, the national patient administrative system ment, which included exchange of the tibial poly-(PAS) was used to search for unreported revisions ethylene insert, were excluded since in the context – minimising the risk of unreported revisions, in of the study these operations were considered to be particular arthrodesis, extraction of the prosthesis, soft tissue operations and not true revisions. In 19 and amputation. Information on sex, age, primary cases, aseptic revisions were wrongly recorded as diagnosis, primary operation, and revisions was infected revisions.
gathered from the database of the registry. Infor-
Patients. 478 first-time revisions of primary
mation on co-morbidities, wound complications knee arthroplasties due to infection remained for after the primary operation, type of infection, the study. An overview of patient allocation is given infecting pathogen, its antimicrobial susceptibil-
in Figure 11. Six patients had both knees revised
ity pattern, surgical and antimicrobial treatment, because of infection and each knee was regarded
THE INFECTED KNEE ARTHROPLASTY
as a separate case. Osteoarthritis (OA) was the pri-
of deep infection. In 11 cases, it was not possible
mary diagnosis in 299 patients (302 cases), rheu-
to determine the exact date of diagnosis from the
matoid arthritis (RA) was the primary diagnosis hospital records. in 140 patients (143 cases), and other disease was
The type of infection was determined based on
the primary diagnosis in 33 patients (33 cases). both clinical appearance and timing. An acute hae-Regarding gender, 54.6% of the OA cases and matogenous infection was defined as an infection 67.8% of the RA cases were females. Today, OA is occurring acutely around a formerly uninfected the predominant indication for knee arthroplasty; knee arthroplasty, irrespective of the time from pri-however, during the time of the study, patients with mary arthroplasty until diagnosis of infection. To RA made up a larger proportion of those being be classified as an acute haematogenous infection, operated (Figure 1). A modified Charnley's classi-
it had to be clear that there was an interval without
fication for the knee (Charnley 1979, Dunbar et al. signs of infection between the primary arthroplasty 2004) was used as an estimate of co-morbidity and and the occurrence of infection. Deep infections the patients were classified as group A (disease in that occurred after surgical intervention other than the index knee only), group B (bilateral knee dis-
revision or through direct spreading from an adja-
ease), or group C (remote arthritis and/or a medical cent traumatic wound into the joint, or after an condition that affected their ability to ambulate). arthrocentesis, were classified separately as sec-14% of the patients were noted to have diabetes.
ondary infections. The remaining infections were
The primary operations were performed at classified according to the time of diagnosis into
75 orthopaedics departments, the first in 1976 early infections (≤ 3 months from primary arthro-(4 cases) and the most recent in 2000 (11 cases). plasty), delayed infections (between 3 months and There were 389 TKAs (81.4%), 65 UKAs (13.6%), 2 years), and late infections (more than 2 years). In 4 combined medial and lateral UKAs (0.8%), 17 paper I, these remaining infections were even clas-hinged prostheses (3.6%), and 3 femuro-patellar sified as early post-operative infections (≤ 4 weeks) prostheses (0.6%).
and late infections (> 4 weeks), after those infec-
Bone cement was used for fixation in 96% of tions diagnosed at a presumed aseptic revision had
cases, but information about the type of cement been classified separately. In 9 cases, based on the used was available in only 45% of cases; of these, existing information, it was not possible to deter-90% contained antibiotic. Information on the type mine the type of infection.
of systemic antibiotic prophylaxis used could not
Re-operation prior to the index operation was
be extracted from the hospital records, but the most defined as any operation at the knee joint that did not commonly used antibiotic prophylaxis in Sweden involve exchange, addition, or removal of a pros-has been cloxacillin (SHPR 2009).
thetic component, with the exception of exchange
Information about wound complications was of the tibial insert in conjunction with debride-
gathered from the hospital records, and it was ment. In 220 cases (46.0%), re-operations were available in 444 cases (92.9%). To be recorded as a performed after the diagnosis of a deep infection wound complication, the wound disturbance had to and before the index operation. Continuous lavage have occurred during the first 30 days after primary was most common (116 cases), followed by deb-operation and had to have been noted before deep ridement (43 cases, 4 of which included exchange infection was diagnosed. The wound complica-
of the tibial insert), arthroscopy (31), wound revi-
tions were classified as culture-positive incisional sion (16), lavage (13), extirpation of a sinus tract SSI, prolonged wound drainage, skin necrosis, (8), and incision and drainage (4). The time from wound rupture, prolonged wound healing, bleed-
the diagnosis of infection until the re-operation was
ing, and inflammation.
less than 4 weeks in 205 cases (93.2%).
The time of infection was defined as the date on
The index operations were performed at 59
which the treating surgeon considered the knee to orthopaedics departments throughout Sweden be deeply infected. This date did not always coin-
(approximately 1 operation every other year), the
cide with the time of appearance, as there could first in 1986 (n = 24), and the most recent in 2000 be a reluctance to correctly interpret obvious signs (n = 41). The index operations were categorised
Anna Stefánsdóttir
as either one-stage revisions, two-stage revisions, how many patients received antibiotics before arthrodeses, extractions, above-the-knee amputa-
sampling for culture.
tions, or other operations. Unconventional surgical
For species identification we relied on the cul-
treatments, such as partial revision or the use of ture reports from the microbiology departments the same components after re-sterilisation, were and statements in the medical records. In some grouped as other operations.
cases, only the type of bacterium (for example
Antibiotics were widely used, both before and "anaerobic Gram-positive coccus") or the genus
after the diagnosis of a deep infection, but the (for example, Enterococcus sp. or Staphylococ-information in the hospital records was unreliable. cus sp.) was given. The antibiotic susceptibility Better information was available on the use of anti-
reported by the microbiological laboratories as S
biotics after the index operation, and in 17 cases a (sensitive), I (intermediate), or R (resistant) was combination including rifampicin was used.
noted. Isolates of the same bacterial species were
Microbiology. 52 cases were excluded from not tested against the same antimicrobial agent in
the study on microbiology (paper II). In 41 cases, all the microbiological laboratories, or throughout no information on microbiological findings was the study period. Reported susceptibility to PcV available and in 4 the information was based on and PcG is reported together as susceptibility to culture from a sinus tract, which is regarded as an Pc. Staphylococcal isolates were variously tested unreliable type of culture. In 7 cases, the patient for susceptibility to oxacillin, dicloxacillin, cloxa-record included information on microbiology but cillin, or simply isoxazolylpenicillins. An isolate the treating doctor had judged that the findings tested against one of these agents was considered reported had no clinical relevance.
to be S, I, or R to isoxazolylpenicillins and those S.
Culture reports were available for study in 288 aureus that were R were called methicillin-resist-
of the 426 cases. Six were excluded, as the micro-
biological findings in the culture report had been
When performing statistical analysis, the patho-
judged by the treating doctor to be without any gens were divided into 9 groups: S. aureus, CNS, clinical relevance and these findings were not in streptococci, other aerobic Gram-positive bacteria, agreement with other information on microbiol-
Gram-negative bacteria, anaerobes, other patho-
ogy reported in the medical record. In 19 cases, gens, polymicrobial infections, and negative cul-the culture was reported negative. Of the 263 cases tures.
remaining, 21 had a polymicrobial infection (18
Result of treatment. To evaluate the results of
with 2 pathogens and 3 with 3). In one case, two treatment, 2 end-points were determined. Firstly, S. aureus isolates with different susceptibility pat-
the re-revision rate due to infection was gathered
terns each grew in 4 of 5 tissue samples collected from SKAR. All cases could be followed concern-during surgery, and in 8 cases two or more strains ing further revision from the date of index opera-of CNS were cultured from at least 2 tissue sam-
tion – or in the case of a two-stage revision arthro-
ples each. Of the 296 isolates no susceptibility pat-
plasty or arthrodesis from the date of stage 2 – until
tern was reported for 11, leaving 285 isolates for the date of death or until closure of study at the end study on antimicrobial susceptibility pattern.
of 2006. The median follow-up time with respect
The microbiological findings were based on to re-revision was 7.9 years, with a range from 17
tissue cultures in 221 cases, on synovial fluid cul-
days (due to death early after index operation) to
ture (gained either from knee aspiration or during 21.4 years. Re-arthrodesis of an infected arthrod-surgical revision) in 165 cases, and on wound cul-
esis and above the knee amputation after an extrac-
ture in 21 cases; in 19 cases, the type of culture was tion was considered as re-revision, despite that the unknown. The decision to include wound cultures operation did not include removal of a prosthetic was based on the findings of Cuñé and co-workers component.
(Cuñé et al. 2009). Most of the wound cultures
Secondly, the rate of failure to eradicate infec-
were from early infections, and excluding these tion was determined by adding information from cases would have led to a bias because of miss-
the hospital records on failed but not re-revised
ing information on early infections. It is not known cases to the re-revision rate. It is difficult to dif-
THE INFECTED KNEE ARTHROPLASTY
ferentiate between persistent infection and new interval between stage 1 and 2 and the state of the infection, especially retrospectively. Furthermore, joint during the interval was analysed. Those cases it can be argued that for the individual patient it is with failure to eradicate infection were compared of no importance whether the infection is a persist-
with cases without failure to eradicate infection.
ent or a recurrent one. Thus, all infections diag-
Time trends were studied by dividing the study
nosed after the index operation were regarded as a period into three 5-year periods, with the index failure to eradicate infection. In some cases, life-
operation performed 1986–1990, 1991–1995, or
long antibiotics were prescribed, but if no clinical 1996–2000. In paper II, the period was divided
signs of infections were detected these cases were depending on the date of culture.
not regarded as failures. The follow-up time with
respect to failure to eradicate the infection was
calculated as the time from the date of the index Paper IV
operation – or in the case of a two-stage revision arthroplasty or arthrodesis from the date of stage In 114 consecutive cases treated at the department 2 – until date of revision, death, or the latest avail-
of Orthopaedics, at Lund University Hospital,
able information in the medical records. Optimally, during 2008 the time of administration of preoper-the follow-up time should be at least 1 year after ative prophylactic antibiotic in relation to the start conclusion of antibiotic treatment but due to the of surgery was recorded from the operation report. retrospective nature of this part of the study, this The information was collected without the involve-could not always be accomplished. The median ment or knowledge of the staff who administered follow-up time regarding failure to eradicate the the prophylactic antibiotic. According to local infection was 2.1 years, with a range from 0 to 16.9 guidelines, patients should have the preoperative years. 80% of the one-stage revisions and 74.7% prophylactic antibiotic 30 minutes before the start of the two-stage revisions were followed in this of surgery but administration within a time interval respect for more than a year whereas only 54.9% from 45 minutes to 15 minutes before start of sur-of the arthrodesis patients and 27.6% and 16.7% gery was regarded as adequate.
of those with extractions and amputations, respec-
The timing of prophylactic antibiotics was not
tively, could be followed for more than a year. It is registered in the SKAR before 2009. To search possible that patients with persistent infection (that for this information, 300 cases were randomly was not revised) were treated at a department other selected from the 9,238 primary TKAs registered than the one that performed the index operation, in the SKAR as having been performed during and were thereby missed.
2007 because of osteoarthritis. The anaesthetic
Mortality. The 1-year mortality was determined record was requested from the operating unit and
based on information from the Swedish Cause of 291 reports were received. Four patients had both Death Register (Statistics Sweden).
knees operated on the same day; in 3 cases, the
Prognostic factors. When searching for factors knee selected for study was the first one and in 1
that affected outcome, the analysis was restricted to case it was the second. Information on the type and those cases that were treated with revision arthro-
dose of prophylactic antibiotic, as well as the time
plasty in one or two stages. The variables that were of administration in relation to the inflation of a tested were: sex, primary diagnosis, age at index tourniquet and to the start of surgery, was searched operation, Charnley group, the presence of diabe-
for in the anaesthetic record. Administration of
tes, the presence of wound complication(s) after prophylactic antibiotic more than 45 minutes primary operation, type of infection, type of patho-
before the start of surgery was regarded as inad-
gen, occurrence of re-operation before the index equate because of the short half-life of the most operation, time from diagnosis to index operation, commonly used antibiotics. Administration later one- or two-stage revision, year of index operation, than 15 min before the start of surgery was also the region in which the index operation was per-
regarded as inadequate, as in most cases the infu-
formed, and use of rifampicin in antibiotic treat-
sion would not have entered the circulation at the
ment. For two-stage revision, even the length of the time of incision or inflation of a tourniquet.
Anna Stefánsdóttir
It was assumed that censored cases had the same
risk of re-revision or failure to eradicate infection
Paper I. The Chi-square test was used to compare as those that were not censored. This assumption proportions.
might be untrue, as it is possible that dying and
Paper II. The Chi-square test was used to evalu-
failure to eradicate infection were competing risks.
ate the distribution of microbiological findings.
For statistical evaluation of categorical factors
Cuzick's test for trend (a Wilcoxon-type test for that could be prognostic of outcome, Kaplan-Meier trend across a group of three or more independent curves were calculated separately for each group random samples (Cuzick 1985)) was used to evalu-
and the log rank test used to evaluate whether there
ate changes over time in antibiotic susceptibility were differences in survival. For continuous vari-pattern.
ables, Cox regression analysis was used.
Paper III. The Chi-square test was used to com-
Paper IV. The 95% confidence interval for pro-
pare proportions. The Kaplan-Meier method was portions was calculated as ± 1.96 standard errors.
used to calculate the cumulative re-revision rate for
For all statistical evaluations, the significance
infection and the cumulative rate of failure to eradi-
level was set at p < 0.05.
cate infection for those treated with two-stage revi-
The statistical analyses were performed using
sion. Censoring events were death and re-revision the software packages PASW Statistics 18 (SPSS, for reasons other than infection (aseptic revision or Chicago, IL) and STATA version 11.1 (Stata Corp above-the-knee amputation due to atherosclerosis). LP, College Station, TX).
THE INFECTED KNEE ARTHROPLASTY
Results / Summary of papers
of infection (30.3%), followed by delayed infec-
Paper I: The time and type of deep
tion (between 3 months and 2 years, 28.4%) and
infection after primary knee arthroplasty
acute haematogenous infection (22.0%). Using
In 478 cases of first-time revisions due to infection, the classification system proposed by Segawa and during the years 1986–2000 the time from primary co-workers, late (chronic) infection was the most knee arthroplasty until the diagnosis of deep infec-
common type of infection (59.9%), followed by
tion was found to range from 3 days to 21.3 years. acute haematogenous infection (22.0%), and only Two-thirds of the infections (317 cases) were 52 cases (11.1%) were diagnosed as early postop-diagnosed within 2 years of primary arthroplasty erative infections; that is, ≤ 4 weeks after primary (Figure 12). Of those that were diagnosed within knee arthroplasty. 2 years, almost half of the cases (143 of 317) were
In 186 cases, a wound problem was noted during
diagnosed within 3 months (Figure 13).
the first 30 postoperative days, before deep infec-
Acute haematogenous infections were found to tion was diagnosed. The incidence of wound com-
occur at all times after primary arthroplasty, and plications varied depending on the type of infec-could not be classified as a subgroup of late infec-
tion. When using Zimmerli's classification, this
tion. Infections occurring after surgical interven-
varied from 7.4% and 8.7% in those with second-
tion other than revision or through direct spread ary and acute haematogenous infection, respec-from an adjacent traumatic wound into the joint, tively, to 17.2% in those with late infection, and or after an arthrocentesis, did not fit in to the exist-
57.1% and 61.3% in those with delayed and early
ing classification systems and were classified sepa-
infection. The most common type of wound com-
rately as secondary infections. Using the classifica-
plication was wound drainage (n = 74), followed
tion system proposed by Zimmerli and co-workers, by culture-positive superficial surgical site infec-with the modification that acute haematogenous tion (44), skin necrosis (25), wound rupture (21), infections could occur at all times and that sec-
inflammation (15), prolonged wound healing (5),
ondary infections were classified separately, early and bleeding (2). infection (≤ 3 months) was the most common type
positive culture at revision
positive culture at revision
acute haematogenous
acute haematogenous
other (early, delayed, late)
other (early, delayed, late)
Years since primary arthroplasty
Months since primary arthroplasty
Figure 12. The number of deep infections diagnosed
Figure 13. The number of deep infections diagnosed
each year after primary knee arthroplasty, shown
each month during the first 2 years after primary knee
according to type of infection, in 467 cases that were
arthroplasty, shown according to type of infection, in
revised due to infection in Sweden, 1986–2000.
317 cases that were revised due to infection in Sweden, 1986–2000.
Anna Stefánsdóttir
Negative culture
Polymicrobial Other
Gram-negative bacteria Other aerobic Gram-positive bacteria
Streptococcus spp.
Coagulase-negative staphylococci
Staphylococcus aureus
Figure. 14 The microbiological spectrum of infected primary knee arthroplasties surgi-cally revised in Sweden during 1986–2000, divided into 3 periods based on the date of culture.
lowed by streptococci (19/99, 19.2%) and Gram-
Paper II: Microbiology of the infected
negative bacteria (8/99, 8.1%). The most common
knee arthroplasty: Report from the
pathogens in polymicrobial infections were CNS,
Swedish Knee Arthroplasty Register on
Gram-negative bacteria and Enterococcus spp.
426 surgically revised cases
Only 1 of 84 S. aureus isolates (1.2%) tested
The microorganism most commonly found in against isoxazolyl penicillins was resistant 426 cases of infected primary knee arthroplasties (MRSA). Sixty-two of 100 CNS isolates (62%) revised due to infection, during 1986–2000, was tested against isoxazolyl penicillins were resistant. Staphylococcus aureus, which was the sole causa-
Gentamicin resistance was found in 1 of 28 tested
tive pathogen in 30.5% of cases, followed by coag-
isolates of S. aureus (4%) and 19/29 tested isolates
ulase-negative staphylococcus (CNS), which was of CNS (66%).
the sole pathogen in 27.5% of cases. Streptococcus
The microbiology was found to change signifi-
accounted for 8.4% of the infections, Enterococcus cantly during the period studied (p = 0.019) (Figure spp. for 7.7%, Gram-negative bacteria for 6%, and 14). The proportion of infections caused by S. anaerobic bacteria for 2.7%. In 6.3% of cases more aureus decreased from 46.3% during 1986–1990 than one pathogen was cultured (polymicrobial to 27.6% during 1996–2000. At the same time, infections), and in 9.2% the cultures were negative. the proportion of infections caused by enterococci
The microbiological spectrum varied considera-
increased. No enterococcal strains were cultured
bly depending on the type of infection (p < 0.001). before 1991 and of the 33 strains cultured, 21 were CNS was the most common pathogen in early, isolated in 1996 or later.
delayed, and late infections (105/229, 35.1%), fol-
The reported methicillin resistance among CNS
lowed by S. aureus (55/299, 18.4%), whereas S. increased during the period studied (p = 0.002), aureus was the most common pathogen in acute with 0/6 reported resistant in 1990 or earlier, 18/31 haematogenous infections (67/99, 67.7%), fol-
during 1991–1995, and 45/63 during 1996–2000.
THE INFECTED KNEE ARTHROPLASTY
Two-stage, 12 (3)
Aseptic revision, 2
Arthrodesis, 16 (3)
Re-arthrodesis, 2 (1)
Two-stage, 281 (22)
Extraction, 5 (1)
aseptic causes, 3
Aseptic revision, 13 (1)
Partial one-stage, 1 (1)
Planned two-stage
Extraction only, 8
Infected primary
Re-arthrodesis, 1
knee arthroplasties
One-stage, 45 (1)
Extraction, 1 (1)
Aseptic revision, 3
Arthrodesis, 103 (7)
Re-arthrodesis, 3
Planned arthrodesis
Extraction only, 2
Figure 15. Flow chart showing revisions per-
Extraction, 19 (1)
formed in 478 cases of infected primary knee arthroplasty. The numbers of cases in which
infection was not eradicated but further sur-gery was not performed are given in paren-
Aseptic revision, 1
Cumulative rates (Kaplan-Meier)
Paper III: 478 primary knee arthroplasties
revised due to infection – a nationwide
failure to eradicate infection rate
During the period 1986–2000, two-stage revision
arthroplasty was the most commonly used surgical
treatment for infected primary knee arthroplasty
in Sweden (289/478, 60.5%) (Figure 15). There
were regional differences in type of treatment. The highest proportion of patients treated with revision
arthroplasty (one- or two-stage) was in the western
region (78%), and the lowest in the northern region
(61%). The highest proportion of patients treated
Years after index operation
with an arthrodesis was in the northern region (33%), and the lowest was in the western region Figure 16. The cumulative re-revision rate and rate of
failure to eradicate infection after 281 two-stage revi-
(12%). 40% of the one-stage revisions were per-
sion arthroplasties performed in Sweden, 1986–2000.
formed in the southern region. The proportion of patients undergoing revision arthroplasty increased was 9.4% (95% CI 6.5–13.5) at 2 years and 12.7% from 59.6% in the period 1986–1990 to 75.3% (95% CI 9.2–17.8) at 5 years. The cumulative rate during 1995–2000, and the proportion of patients of failure to eradicate infection was 17.8% (95% having an arthrodesis decreased from 27.3% in CI 13.3–24.0) at 2 years and 27.5% (95% CI 1986–1990 to 19.5% in 1995–2000.
21.3–38.3) at 5 years (Figure 16). Arthrodesis was
After a two-stage revision arthroplasty, the the most common surgical method used when re-
cumulative re-revision rate because of infection revising an infected knee arthroplasty (Figure 15).
Anna Stefánsdóttir
The only factor that was found to be predic-
Number of cases
tive of failure to eradicate infection after a revi-sion arthroplasty (one- or two-stage) was a his-
tory of wound complication after the primary operation and before deep infection was diagnosed (p = 0.005). The risk of failure to eradicate infec-
tion was doubled for those with a history of wound complication after primary arthroplasty compared
to those who did not have a history of wound com-plication (RR = 2.04, 95% CI 1.23–3.39). Of the 34
cases with wound complication and where there was a failure to eradicate infection, 31 were early or delayed infections.
-150 -120 -90 -60 -30
In 59 of the 281 two-stage revisions that were
Minutes before/after inflation of tourniquet
completed, and in 5 of the 45 one-stage revisions, Figure 17. The timing of administration of prophylactic infection was not eradicated. The difference was antibiotic in relation to the inflation of a tourniquet not significant (p = 0.150), but it is questionable in 176 cases of primary TKA. Zero represents the start
of surgery. The green bars correspond to acceptable
whether comparison should be made because of timing.
differences in selection.
A spacer block made of antibiotic-loaded
PMMA was the most commonly used method for pital, initiated by a local strategic program against local antibiotic treatment and stabilisation of the antibiotic resistance, signalled that the timing of joint during the interval between stage 1 and stage administration was inadequate. To verify these 2. Using both PMMA beads and a spacer gave results and to test the hypothesis that the timing a lower rate of failure to eradicate infection, but was inadequate even at other departments, a larger compared to spacer the difference was not statisti-
study was conducted in Lund, and 291 cases ran-
cally significant (p = 0.123).
domly selected from the SKAR – from the 9,238
The most commonly used technique to accom-
primary TKAs reported to have been performed
plish an arthrodesis was external fixation, which because of OA during 2007 – were studied .
was used in 79 cases, 38 of which were done in a
Of the 114 patients studied in Lund, only 51
two-stage manner. An intramedullary rod was used (45%, 95% CI: 36–54%) received the first antibi-in 21 cases, 17 of which were done in 2 stages. otic dose of antibiotic between 45 and 15 minutes In 2 cases, the joint was stabilised with pins (one-
before the start of surgery. In 22 cases (19%), sur-
stage), and in 1 case it was stabilised with a plate gery was started at the same time or before admin-and screws (two-stage).
istration of prophylactic antibiotic. In the material
The 1-year mortality for those patients treated from the SKAR, the time of administration of the
with extraction of the implant or above-the-knee first doses of antibiotic prophylaxis could be ascer-amputation was high.
tained from the anaesthetic record in 198 cases. Only 113 patients (57%, CI: 50–64%) received the antibiotic between 45 and 15 minutes before the start of surgery. The mean time was 41 min-
Paper IV: Inadequate timing of prophy
utes, with a range from 105 minutes before the
lactic antibiotics in orthopedic surgery.
start of operation to 120 minutes after the start. In
We can do better
176 cases, it was possible to read the time from
As the effect of prophylactic antibiotics is related administration of prophylactic antibiotic until the to the timing of administration, it is important to time of inflation of a tourniquet. Only 94 (53%, CI: follow how the routines with preoperative prophy-
46–61%) received antibiotics between 45 and 15
lactic antibiotics are working. A small study at the minutes before the tourniquet was applied (Figure Department of Orthopaedics, Lund University Hos-
17). The mean time was 40 minutes, with a range
THE INFECTED KNEE ARTHROPLASTY
from 153 minutes before the inflation of a tourni-
Information on type of antibiotic used was avail-
quet to 120 minutes after inflation.
able in 247 cases (85%), and of these 89% had
In 2 of the 4 bilaterally operated patients, no received cloxacillin, 9% clindamycin, and 2%
additional antibiotic was given before the start of cefuroxime. The most common dose of cloxacillin surgery on the second knee.
was 2 g (158/212 patients, 75%).
Anna Stefánsdóttir
Deep infection after a knee arthroplasty is a Timing and type of infection
demanding and growing problem (Kurtz et al. 2007). In papers I–III, a large number of primary There have been relatively few reports involv-knee arthroplasties that were surgically revised due ing all infected knee arthroplasties, and not only a to an infection, during the years 1986–2000, were subgroup of patients (Walker and Schurman 1984, identified by searching the Swedish Knee Arthro-
Grogan et al. 1986, Bengtson et al. 1989, Bengtson
plasty Register (SKAR). The information was used and Knutson 1991, Rasul et al. 1991, McPherson et to determine the timing and type of infection, the al. 1999, Segawa et al. 1999, Peersman et al. 2001, microbiology and antimicrobial resistance pattern, Husted and Toftgaard Jensen 2002, Laffer et al. and the type of treatment and results thereof. The 2006, Pulido et al. 2008). In these studies, the onset strength of the study is that it covered all revisions of infection was reported to be within 3 months of performed, irrespective of type of hospital, type of surgery in 29–46% of cases and within 4 weeks in infection, or type of treatment. In paper IV, a spe-
3–48% of cases. The proportion of haematogenous
cific and important part of the preventive measures infections varied from 6% to 49%. There are sev-was studied – i.e. the timing of administration of eral methodological differences between the stud-the first dose of prophylactic antibiotic.
ies, which is why comparisons should be done with caution. The largest study, involving 357 cases oper-ated during 1975–1985, was an earlier study from the SKAR where 46.5% of the infections were diag-
Limitations of the study
nosed within 3 months of primary arthroplasty; 25%
The major drawback of the study is that not all were reported to be of haematogenous origin, and in infected knee arthroplasties were included. An 40% of cases the primary diagnosis was RA (Bengt-unknown number of patients were treated with-
son and Knutson 1991). Today, the overwhelming
out revision of the prosthetic components, and majority of patients who undergo knee arthroplasty were thereby not reported to the register. Those have OA (Figure 1), and as the most common type who were not included may have been the frail or of infection in OA patients was early infection, this elderly patients, those who refused surgery, those type of infection is probably even more common who were treated with suppressive antibiotics, now than during the study period.
or those with soft tissue operation only. It is not
As there is no clear evidence for the statement
possible to predict the effect of these cases on the that infections with a duration of less than 4 weeks overall result. In addition, it is probable that infec-
can be treated with debridement, there is no reason
tions caused by low-virulence organisms were (to to classify the infections as early postoperative (≤ an unknown extent) not diagnosed as being septic 4 weeks) and late (> 4 weeks). Classification of during revision and were therefore not reported. infections as early (≤ 3 months after the primary Data on some of the variables were collected retro-
arthroplasty) and delayed (3 months to 2 years)
spectively, which could have affected the reliabil-
highlights the pathogenesis and the general belief
ity. The information gathered was not complete in that most infections are acquired during or shortly all cases, and some data were less available during after surgery, but may not be detected until later. the first years of the study. In addition, no infor-
The high incidence of wound problems in those
mation was available on several factors that may with delayed infection supports this view. Wound have affected the outcome, with the state of the soft complication is a well known risk factor for later tissues around the knee, complete information on diagnosis of deep infection (Berbari et al. 1998, co-morbidities, and smoking habits probably being Abudu et al. 2002, Saleh et al. 2002, Phillips et the most important ones.
al. 2006, Galat et al. 2009), but surprisingly little
THE INFECTED KNEE ARTHROPLASTY
guidance can be found in the literature regarding aureus was the infecting pathogen in 6/15 (40%) optimal treatment (Vince and Abdeen 2006) and (Fulkerson et al. 2006).
the results of treatment (Galat et al. 2009).
The proportion of polymicrobial infections was
Acute haematogenous infections should be clas-
in accordance with that in other studies (Peersman
sified separately, irrespective of the length of time G 2001, Pulido et al. 2008), and as described ear-from primary operation. Furthermore, we defined a lier, polymicrobial infections were most common group of secondary infections that should be clas-
in early infections (Marculescu and Cantey 2008).
sified separately.
The testing of anti-microbial susceptibility was not
CNS was the most prevalent pathogen in the early standardised, and during the study period, mini-and delayed infections. Infections caused by CNS mum inhibitory concentration (MIC) breakpoints often present with subtle clinical signs and can for several species and antibiotics were changed. often be suppressed easily, but not eradicated, with As a result of this, caution is required when inter-antibiotics. A high level of awareness is needed for preting the results of antibiotic susceptibility.
identification and for timely, resolute treatment.
The prevalence of methicillin-resistant S. aureus
The number of studies that have described the (MRSA) was very low but consistent with the gen-
microbiology in infected knee arthroplasties is lim-
erally low prevalence of MRSA in Sweden (Sten-
ited. In a study of 121 patients who were revised hem et al. 2006).
because of an infected knee arthroplasty at an Eng-
Only 9 of 29 CNS isolates tested were sensitive
lish hospital during the period 1994–2008, CNS to gentamicin, which is in accordance with what caused 49% of the infections, S. aureus 13%, E. has previously been reported in infected hip arthro-coli 7%, Enterococcus faecalis 6%, and other bac-
plasty (Hope et al. 1989). The gentamicin resist-
teria 25% (Nickinson et al. 2010). Information on ance among CNS strains must be considered in type of infection was not provided in the paper. In a revision of an infected knee arthroplasty, and other study on 84 cases of knee arthroplasty, re-operated antibiotic(s) added to the bone cement used in con-at either of two hospitals in the USA during 1991–
temporary spacers and at re-arthroplasty.
2003, S. epidermidis caused 36% of the infections,
The microbiological spectrum changed over
S. aureus 32%, Streptococcus spp. 11%, Entero-
time, with a decrease in the proportion of infections
coccus spp. 7%, E. coli 2%, Pseudomonas aeru-
caused by S. aureus after 1990. There was also a
ginosa 2%, Corynebacterium spp. 7%, and other change in primary diagnosis, with an increase in bacteria 7% (Fulkerson et al. 2006). Of those 8 OA and decrease of RA. Even though the immune infections that occurred within 4 weeks of surgery, system in rheumatoid patients is affected in a com-4 were caused by S. aureus.
plicated manner, both by the disease and its treat-
The microbiological findings in acute haema-
ment, the decrease in infections caused by S. aureus
togenous infections differed significantly from the cannot, with our current knowledge, be explained findings in early, delayed, and late infections, S. by the changes in primary diagnosis. Another aureus being the dominating pathogen. Identify-
factor, that unfortunately could not be studied, is
ing the source of an acute haematogenous infec-
the use of antibiotic-impregnated bone cement.
tion is in many cases a difficult task and in a ret-
Data from the Swedish Hip Arthroplasty Register
rospective study even more difficult. In the few show that the use of antibiotic-impregnated bone cases in which origin could be identified, leg or cement became widespread in hip arthroplasty at foot ulcer was the most common source. There the beginning of the 1990s (SHPR 2003), and it is is little information on haematogenous infections likely that the same applies to knee arthroplasty. It in the literature, but Fulkerson and co-workers could be hypothesised that the use of antibiotics in report that haematogenous infections accounted bone cement had greater effect on S. aureus than on for 17.8% of infected knee arthroplasties and S. CNS, but it is very difficult to evaluate separately
Anna Stefánsdóttir
the effects of the various prophylactic measures revision arthroplasty was 45.5% and the proportion that have been introduced in orthopaedic surgery. treated with an arthrodesis was 38.6% (Bengtson et The microbiology in infected knee arthroplasties al. 1989). In more recent studies, the proportion of has to be examined in the context of the overall surgically revised patients treated with a revision incidence. In previous reports from the SKAR, the arthroplasty has been reported to be in the 68–90% cumulative revision rate (CRR) due to infection has range, and the proportion treated with an arthro-been shown to have decreased from 2.7% during desis to be in the 10–16% range (Segawa et al. 1976–1985 to 1.1% during 1986–2000 (Figure 2). 1999, Husted and Toftgaard Jensen 2002, Laffer et With the described decrease in infections caused al. 2006, Kosters et al. 2009). There appear to have by S. aureus, CNS is now the most important path-
been many arthrodeses in the present study, but it
ogen in infected knee arthroplasty. The methicillin must be kept in mind that there were more rheuma-resistance among CNS strains found in infected toid patients during the earlier years of the study; cases increased. Further studies are required to they may have had poorer bone stock and inferior determine the present status as well as the preva-
quality of the soft tissues. We plan to analyse the
lence of methicillin-resistant CNS in patients at results of arthrodeses in a future study.
admission and in the hospital environment. Beta-
There are many unanswered questions with
lactams continue to be the best choice of systemic regard to the best possible treatment, and good antibiotic prophylaxis, but there is good reason to results have been reported with the use of treat-remind all the personnel involved about preven-
ment strategies that divide considerably from
tive measures other than antibiotics that have been those in the present algorithms. For example, shown to be effective – and are especially impor-
two-stage revisions have been performed without
tant in the case of CNS. The observed increase in the use of prolonged antibiotic treatment and the infections caused by enterococci, especially during infection reported to be successfully eradicated in the first post-operative period, is a matter of con-
34/38 cases (89%) (Hoad-Reddick et al. 2005). In
cern and requires further study.
another study, 18 patients with MRSA infected knee arthroplasties were treated with a one-stage uncemented revision, followed by intra-articular administration of vancomycin for 6 weeks and
Type of treatment
only 24 hours of intravenous antibiotics. At a
The existing guidelines for choice of surgical mean follow-up of 62 months the infection was treatment in infected knee arthroplasty are largely controlled in all but one patient (Whiteside et al. based on empirical findings. The factors to be con-
sidered when choosing the type of treatment for the
individual patient are: the duration of symptoms,
the general health of the patient, the condition of The results of treatment
the soft tissues and the implant, and bacteriology (Zimmerli et al. 2004, Leone and Hanssen 2005). The crude rate of failure to eradicate infection of In practice, even other factors such as local tradi-
21% found in our study after a two-stage revision
tion, the skill and experience of the orthopaedic arthroplasty is in line with publications reporting surgeon, and the availability of expert knowledge in the poorest results (Jämsen et al. 2009b). Survival microbiology and infectious diseases can affect the analysis, which takes into account that during fol-choice of treatment, and these factors may explain low-up some patients die or are revised for reasons the regional differences found in the choice of other than infection, revealed still higher failure treatment. It is difficult to compare the distribution rates (27.5% at 5 years). It can be questioned, how-between different treatment alternatives found in ever, whether the patients reported in published our study with that in other studies, due to the lim-
studies are representative of the whole group of
ited number of reports on all infected knee arthro-
patients treated for infected knee arthroplasty.
plasties treated. In a previous Swedish study from Probably our results better reflect the everyday 1973–1986, the proportion of patients treated with reality that most patients and orthopaedic surgeons
THE INFECTED KNEE ARTHROPLASTY
are faced with. To improve the results, it appears in cases of failed open debridement and irrigation reasonable to suggest centralisation of treatment (Sherrell et al. 2010, Gardner et al. 2010). to fewer centres. The failure rate after one-stage
It was a disappointment not be able to reveal
revision arthroplasty is in accordance with earlier any other prognostic factors, but even though reports, but differences in selection make compari-
the present cohort included a large number of
sons with previous studies or with two-stage revi-
patients, it was heterogeneous and many orthopae-
sion meaningless.
dic surgeons with varying degrees of experience
The best results were obtained with two-stage were involved. Furthermore, there was variability
revision arthroplasty when an antibiotic-loaded regarding the possibility of consulting infectious PMMA spacer and antibiotic-loaded PMMA beads disease and microbiology specialists. Prospective were left in the joint during the interval between collection of data, including better estimation of stages one and two, even though the difference co-morbidities, is needed.
was not statistically significant. Beads have elution characteristics that differ from those of spacers, which may be beneficial (Walenkamp 2001, Anag-
Timing of antibiotics
nostakos et al. 2009).
The number of patients in our study who received the first dose of antibiotic at a suboptimal time was alarming, and raises concerns about other aspects
of prophylactic measures. It was recently shown in
According to data from the SKAR, the 1-year mor-
a non-randomised study that the use of a simple
tality after a primary knee arthroplasty performed surgical safety check-list reduced morbidity and during 1989–2008 was 1.4%. The substantially mortality. The administration of antibiotics within higher mortality found after arthrodesis, extrac-
60 min before incision improved from 56% to 83%
tion, and amputation probably reflects the poorer by use of the safety list, and the surgical site infec-medical condition of the patients treated by these tion rate was reduced by almost 50% (p < 0.001) methods.
(Haynes et al. 2009). The use of a check-list is recommended.
The half-life of cloxacillin is relatively short (30
minutes), with cefuroxim and clindamycin having
Prognostic factors for failure to
somewhat longer half-lives (66 and 155 minutes,
respectively). If the antibiotic is given too early
A history of wound complication after the primary before the start of surgery, it is not certain that the knee arthroplasty and before the diagnosis of deep concentration of antibiotic in the tissue will be high infection was the only factor that was found to be enough throughout the whole operation. Thus, one predictive of failure to eradicate infection after a could consider whether or not all patients for whom revision arthroplasty. It is not clear how a delay the actual surgical procedure takes more than 1 hour in correct diagnosis can affect the result of treat-
should have a new infusion, starting just before the
ment. The use of antibiotics in patients who had tourniquet is released. This is also what the AAOS wound complications was extensive, but the exact has recommended in its recent document on infec-magnitude was unfortunately impossible to meas-
tion prophylaxis (Prokuski 2008). The document
ure accurately retrospectively. It is possible that states that at twice the half-life of the selected anti-prolonged antibiotic treatment, with retained and biotic (counting from the first injection), a repeat undebrided implant, enhances the development of dose should be given. In knee arthroplasty surgery, antibiotic resistance and thereby makes the infec-
this very often coincides with the release of the
tion more difficult to treat when revised. To our tourniquet. If antibiotic is given too late, the antibi-knowledge, this has not been described before and otic may not reach the tissue at the time of surgery. further studies are needed. Recently, poorer out-
This is especially important when a tourniquet is
come has been reported after revision arthroplasty used during the operation.
Anna Stefánsdóttir
been reported (Bode et al. 2010, Johnson et al.
The future
2010). It is likely that increased attention will be
Antimicrobial resistance is a growing problem. The paid to the quality of air in the operation theatre result of treatment appears to be poorer when the as well as to strict adhesion to hygiene routines in infection is caused by methicillin resistant bacte-
ria (Kilgus et al. 2002, Bradbury et al. 2009, Kurd
There is ongoing experimental work on coating
et al. 2010) and in areas with high prevalence of of implants with antibiotics (Lawson et al. 2010, methicillin resistant bacteria vancomycin has been Smith et al. 2010). With better understanding of recommended as a prophylactic antibiotic (Meehan the mechanism controlling the formation of a bio-et al. 2009). Prophylactic methods other than anti-
film it may become possible to disturb the biofilm
biotics, which can reduce the number of infections, formation and thereby reduce the risk of infection will probably become increasingly important. and improve the results of treatment of a manifest Good effect of decolonisation with chlorhexidine, infection (Hoiby et al. 2010). either as soap or impregnated clothes, has recently
THE INFECTED KNEE ARTHROPLASTY
• Of the 478 first-time revisions performed due
9% had a one-stage revision. Almost 30% were
to infection after a primary knee arthroplasty in
treated with the poorer functional alternatives:
Sweden 1986–2000, 30% were diagnosed within
arthrodesis, extraction of the implant, or above-
3 months from primary operation and two-thirds
the-knee amputation. There were regional differ-
were diagnosed within 2 years. In these cases, a
ences in the type of surgical treatment chosen,
wound complication was frequently noted after
and the average number of cases treated at each
the primary arthroplasty but before the diagnosis
orthopaedics department was 1 every other year.
of deep infection. Acute haematogenous infec-
By centralising the treatment to units with spe-
tions, which accounted for 22% of cases, were
cialists in orthopaedics and infectious diseases
found to occur at all times after primary arthro-
working in a team, every patient could be offered
plasty and to be more common in patients with
the most optimal treatment available.
RA than in those with OA. Awareness of the fact • After a two-stage revision arthroplasty, only that most infections arise early and are associ-
half of those with failure to eradicate infection
ated with wound complications should encour-
were re-revised, the cumulative re-revision rate
age use of judicious postoperative care and could
at 2 years being 9.4% and the cumulative rate
lead to earlier diagnosis and treatment.
of failure to eradicate infection being 17.8%.
• S. aureus was the most commonly found micro-
These figures are in line with the poorest results
organism in the 426 cases that were available
reported in other studies, which indicates that
for microbiological analysis. During the study
there is room for improvement. The only factor
period, the proportion of infections caused by
that was found to be predictive of failure to
S. aureus decreased however, and during the
eradicate the infection was a history of wound
last 5-year period CNS was the most commonly
complication(s) after the primary operation,
found microorganism. CNS was even the most
before the diagnosis of infection. This implies
commonly found microorganism in early and
that every surgeon performing knee arthroplast-
delayed infections. MRSA was found in only
ies has to be capable of taking adequate care of
1 case, whereas increasing methicillin resist-
wound complications.
ance was noted in the CNS isolates. Gentamicin • The time of administration of the first dose of resistance was common in CNS, which has to be
prophylactic antibiotic was suboptimal in 55%
considered in revision surgery – at least when
of the cases studied at Lund University Hospi-
the revision is performed due to infection – as
tal, and in 47% of the cases randomly selected
antibiotic other than gentamicin should be added
from the SKAR. To bring about a change for the
to the bone cement.
better, it is suggested that the WHO's checklist
• A two-stage revision knee arthroplasty was the
should be used at all operations, and that the
surgical method chosen in 60% of the 478 cases
timing of antibiotic administration be reviewed
that were revised for the first time due to an
regularly at all departments.
infection during the years 1986–1990. Another
Anna Stefánsdóttir
Vid en knäprotesoperation ersätts ledytorna i knäet aureus (MRSA). Resistens bland KNS mot meticil-med en protes gjord av metall och plast. Den vanli-
lin ökade under studietiden och närmare undersök-
gaste orsaken till denna operation är artros (ledsvikt). ningar behövs för att ta reda på hur vanligt det är Antalet knäprotesoperationer ökar stadigt och 2009 att patienter inför knäprotesoperation bär på meti-utfördes 12,700 förstagångsoperationer i Sverige. cillinresistenta KNS. Bland KNS var resistens mot Resultaten är överlag goda men en allvarlig kom-
gentamicin, vilket är det antibiotikum som blandas
plikation som drabbar mellan 1 och 2% av patien-
i bencement för att minska risken för infektion,
terna är bakterieinfektion i leden. Om infektionen också vanlig och det måste ortopeder ta hänsyn till upptäcks tidigt kan den behandlas med upprensning vid revisioner utförda på grund av infektion.
i leden och antibiotika men annars måste protesen
Den vanligaste behandlingsmetoden var två-stegs-
avlägsnas. En ny protes kan sedan sättas in, antingen revision (60%) och ytterligare 9% fick en ny knäled vid samma operation (en-stegsrevision) eller efter en genom en-stegsrevision. Nästan 30% behandlades protesfri period då patienten behandlats med antibio-
med steloperation, slinkled eller amputation. Det
tika (två-stegsrevision). I vissa fall leder behandling var regionala skillnader i val av behandling och de av infektionen till stel operation och enstaka gånger flesta ortopedkliniker behandlade mycket få fall. till slinkled (led utan protes) eller amputation. Sedan Det föreslås att knäprotesrevisioner på grund av 1975 har Svenska Knäprotesregistret (SKAR) infektion centraliseras till enheter där ortopeder och samlat information om knäprotesoperationer utförda infektionsläkare tillsammans styr behandlingen.
i Sverige och denna databas har använts för att i
Två år efter två-stegsrevisionen hade 17.8%
detalj granska 478 fall som under åren 1986 till 2000 misslyckats med att bli av med infektionen. Vid genomgick en knäprotesrevision på grund av infek-
denna tidpunkt hade 9.4% reviderats ytterligare en
tion. En revision är en omoperation där protesdelar gång på grund av infektion (räknat med Kaplan-insättes, bytes eller borttages.
Meiers metod). Dessa resultat motsvarar de sämsta
Studien visade att i 30% av fallen hade infek-
resultaten som har presenterats tidigare, men jäm-
tionen bekräftats inom 3 månader från primär-
förelse försvåras av att tidigare studier ofta kommer
operationen och att två tredjedelar av infektionerna från högspecialiserade enheter. Den enda faktorn hade bekräftats inom 2 år. Sårproblem efter primär som uppvisade ett samband med senare misslyck-operationen var vanligt förekommande bland dessa ande i att bota infektion var förekomsten av sårpro-patienter. För att upptäcka infektioner tidigt är blem efter primäroperationen. Detta understryker noggrann uppföljning under den första tiden efter ytterligare vikten av ett adekvat omhändertagande operation viktig och infektion måste misstänkas av patienter med sårproblem.
i de fall där sårproblem föreligger. Drygt 20% av
I en separat studie granskades vid vilken tidpunkt
infektionerna uppstod efter att bakterier tagit sig den första dosen av förebyggande antibiotikum via blodbanan till leden. Denna typ av infektion gavs. För att uppnå den bästa effekten av antibio-(hematogen infektion) var vanligare hos patienter tika rekommenderas att första dosen ges inom 45 med ledgångsreumatism än hos de med ledsvikt.
till 15 minuter före operationsstart. Bland patienter
Infektionerna orsakades oftast av stafylokocker, opererade på Universitetssjukhuset i Lund fick 55%
som är bakterier som normalt finns på huden. den första dosen utanför denna tidsrymd. Bland ett Under de första åren som studerades var Stafylo-
slumpmässigt urval patienter som registrerats i
coccus aureus (den gula stafylokocken) vanligast, SKAR i samband med en knäprotesoperation fick medan koagulas-negativa stafylokocker (KNS, 47% den första dosen antibiotikum utanför denna den vita stafylokocken) orsakade flest infektio-
tidsrymd. Användning av en checklista, framtagen
ner under de senare åren. I enbart 1 fall orsakades av världshälsoorganisationen WHO, kan medföra infektionen av meticillinresistent stafylococcus en förbättring och rekommenderas.
THE INFECTED KNEE ARTHROPLASTY
Yfirlit á íslensku
Við liðskiptaaðgerð á hné er liðflötum hnésins gir methisillín-ónæmir KNS eru á húð þeirra sem skipt út fyrir gervilið úr málmi og plasti. Slitgigt gangast undir liðskiptaaðagerð. Ónæmi gegn gen-er algengasta orsök aðgerðar. Liðskiptaaðgerðum tamicin var einnig útbreytt meðal KNS, en genta-á hné fjölgar stöðugt og í Svíþjóð nam fjöldi micin er það sýklalyf sem blandað er í beinsement aðgerða 12,700 árið 2009. Árangur aðgerðar er til að minnka líkur á sýkingu, og þurfa læknar almennt góður, en þó verða 1-2% sjúklinga fyrir að taka tillit til þessa við enduraðgerðir vegna því að fá bakteríusýkingu í liðinn. Sýkingu sem sýkingar.
greinist snemma má lækna með því að hreinsa og
Algengasta skurðmeðferðin var tveggja-þrepa
skola liðinn og gefa sýklalyf, en að öðrum kosti enduraðgerð (60%) og 9% til viðbótar fengu nýjan þarf að fjarlægja gerviliðinn. Hægt er að setja gervilið við eins-þreps aðgerð. Tæplega 30% inn nýjan gervilið, annað hvort við sömu aðgerð sjúklinga voru meðhöndlaðir með staurliðsaðgerð, (eins-þreps enduraðgerð) eða eftir að hnéð hefur varanlegri fjarlægingu gerviliðs eða aflimun. Flest verið án gerviliðar um tíma og sjúklingurinn sjúkrahús meðhöndluðu fáa sjúklinga og svæðis-fengið sýklalyf (tveggja-þrepa aðgerð). Í vissum bundinn munur var á hvaða meðferð var valin. Lagt tilvikum leiðir sýkingin til staurliðsaðgerðar, var-
er til að enduraðgerðir vegna sýkinga í hnégervi-
anlegrar fjarlægingar gerviliðsins eða aflimunar. liðum fari fram á sjúkrahúsum þar sem bæklunar-Sænska hnégerviliðaskráin (Svenska knäprotes-
læknir og smitsjúkdómasérfræðingur starfa náið
registret) hefur frá 1975 safnað upplýsingum um saman.
liðskiptaaðgerðir á hné sem framkvæmdar eru í
Tveimur árum eftir tveggja-þrepa enduraðgerð
Svíþjóð. Úr skránni voru fengin 478 tilfelli sem á höfðu 17.8% sýnt merki þess að sýking væri í árunum 1986–2000 höfðu gengist undir aðgerð þar liðnum. Önnur enduraðgerð vegna sýkingar hafði sem gerviliður var fjarlægður eða skipt út vegna verið framkvæmd hjá 9.4%. Þessi árangur er með sýkingar og þau rannsökuð ítarlega.
þeim lakari sem kynntur hefur verið, en saman-
Í 30% tilvika greindist sýkingin innan þriggja burður er erfiður þar sem fyrri rannsóknir hafa
mánaða frá fyrstu aðgerð og tveir þriðju hlutar flestar verið gerðar við sérhæfðar stofnanir. Eina sýkinganna höfðu greinst innan tveggja ára. Í breytan sem reyndist hafa forspárgildi fyrir áfram-þessum hópi voru vandamál tengd skurðsári mjög haldandi sýkingu í liðnum eftir enduraðgerð var algeng. Mælt er með góðu eftirliti með sjúklingum vandamál tengt skurðsári eftir fyrstu aðgerð. Þetta fyrst eftir aðgerð og að tekið sé á vandamálum undirstrikar enn frekar mikilvægi þess að sinna tengdum skurðsári af ákveðni. Rúmlega 20% þessum vandamálum vel.
sýkinganna voru blóðbornar, það er að bakteríur
Í sérstakri rannsókn var skoðað hversu mörgum
dreifðust með blóði í liðinn. Þessi tegund sýkingar mínútum áður en aðgerð hófst sjúklingar fengu var algengari hjá liðagigtarsjúklingum en slitgig-
fyrsta skammt fyrirbyggjandi sýklalyfjagjafar, en
mælt er með að fyrsti skammtur sé gefinn 45 til
Sýkingin var oftast af völdum stafýlókokka, 15 mínútum fyrir aðgerð. Meðal sjúklinga sem
sem eru bakteríur sem tilheyra eðlilegri húðflóru. gengust undir aðgerð við Háskólasjúkrahúsið í Fyrstu ár rannsóknarinnar var Stafýlókokkus Lundi reyndist tímasetning fyrstu sýklalyfjag-aureus (guli stafýlókokkurinn) algengastur en jafar vera utan réttra tímamarka í 55% tilvika. Í þau síðustu kóagúlasaneikvæðir stafýlókokkar tilviljunarkenndu úrtaki sjúklinga úr sænsku hné-(KNS, hvíti stafýlókokkurinn). Í einungis einu til-
gerviliðaskránni reyndust 47% hafa fengið fyrsta
felli orsakaði methisillín-ónæmur Stafýlokokkus skammtin utan réttra tímamarka. Til úrbóta er mælt aureus (MÓSA) sýkingu. Ónæmi meðal KNS gegn með notkun gátlista, sem gefinn hefur verið út af methisillíni jókst á tímabilinu og nánari rannsókna Alþjóðaheilbrigðismálastofnuninni (WHO).
er þörf til að ganga úr skugga um hversu algen-
Anna Stefánsdóttir
I would like to express my sincere gratitude to the Johan Lindahl and Birger Bylander for shouldering following people:
my clinical work while I was busy writing.
Kaj Knutson, my supervisor, for being so generous Gun-Britt Nyberg for her encouragement and guid-
with his wide knowledge of orthopaedic infec-
ance through the formalities.
tions, and for his guidance in constructive think-ing. I am also extremely grateful for his help All my colleagues at the orthopaedic department with the layout of this thesis.
in Lund for inspiring discussions and compan-ionship.
Lars Lidgren, my co-supervisor, for his never-end-
ing enthusiasm and willingness to share one of The secretaries at orthopaedic departments through-his favourite subjects, and for his patience while
out Sweden who provided me with copies of hos-
I was busy with other important work.
pital records, and the personnel of the microbiol-ogy departments who provided me with culture
Otto Robertsson, my co-supervisor, for teaching
me the importance of preciseness in scientific work, for extracting whatever I needed from the My mother, Kristjana, my sisters and brother, and database, and for his unstinting support.
my extended family for always believing in me and giving me the sense that I belong, despite so
Daniel Johansson for his excellent work on the
many years abroad.
microbiology paper.
My family – my dear husband Jón Erlingur and our
Annette W-Dahl, Pelle Gustafson, and Sverrir
wonderful children Stefán Erlingur, Sigtryggur,
Kiernan for our enjoyable collaboration on the
Hildur Ylfa and Katrín Una – for your love.
antibiotic paper.
Jonas Ranstam for his invaluable advice on statis-
The studies in this thesis were supported by grants
from: the Swedish Association of Local Authori-ties and Regions (SALAR); the Faculty of Medi-
Urban Rydholm for his support, and for an instruc-
cine, Lund University; Region Skåne; the Swedish
tive and enjoyable decade at the rheumatology Research Council – Medicine (09509); and Stif-surgery unit in Lund.
telsen för bistånd åt rörelsehindrade i Skåne.
THE INFECTED KNEE ARTHROPLASTY
AAOS work group. Guidelines for the diagnosis of peripros-
Berdal JE, Skramm I, Mowinckel P, Gulbrandsen P, Bjorn-
thetic joint infections of the hip and knee. Guideline and
holt JV. Use of rifampicin and ciprofloxacin combina-
evidence report. American Academy of Orthopaedic
tion therapy after surgical debridement in the treatment
Surgeons, 2010. Available at www.aaos.org/research/
of early manifestation prosthetic joint infections. Clin
guidelines/guide.asp. Accessed October 28, 2010.
Microbiol Infect 2005; 11(10): 843-5.
Aboltins CA, Page MA, Buising KL, Jenney AW, Daffy JR,
Bernatsky S, Hudson M, Suissa S. Anti-rheumatic drug use
Choong PF, Stanley PA. Treatment of staphylococcal
and risk of serious infections in rheumatoid arthritis.
prosthetic joint infections with debridement, prosthe-
Rheumatology (Oxford) 2007; 46(7): 1157-60.
sis retention and oral rifampicin and fusidic acid. Clin
Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vanden-
Microbiol Infect 2007; 13(6): 586-91.
broucke-Grauls CM, Roosendaal R, Troelstra A, Box
Abudu A, Sivardeen KA, Grimer RJ, Pynsent PB, Noy M.
AT, Voss A, van der Tweel I, van Belkum A, Verbrugh
The outcome of perioperative wound infection after total
HA, Vos MC. Preventing surgical-site infections in nasal
hip and knee arthroplasty. Int Orthop 2002; 26(1): 40-3.
carriers of Staphylococcus aureus. N Engl J Med 2010;
Anagnostakos K, Wilmes P, Schmitt E, Kelm J. Elution of
362(1): 9-17.
gentamicin and vancomycin from polymethylmethacr-
Borden LS, Gearen PF. Infected total knee arthroplasty. A
ylate beads and hip spacers in vivo. Acta Orthop 2009;
protocol for management. J Arthroplasty 1987; 2(1):
80(2): 193-7.
AOANJRR. Australien Orthopedic Association National
Bradbury T, Fehring TK, Taunton M, Hanssen A, Azzam K,
Joint Replacement Registry. Hip and knee arthroplasty.
Parvizi J, Odum SM. The fate of acute methicillin-
Annual report 2009. Available at www.aoa.org.au.
resistant Staphylococcus aureus periprosthetic knee
Accessed October 28, 2010.
infections treated by open debridement and retention of
Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson
components. J Arthroplasty 2009; 24(6 Suppl): 101-4.
H, Peto TE, McLardy-Smith P, Berendt AR. Prospec-
Brandt CM, Sistrunk WW, Duffy MC, Hanssen AD, Steckel-
tive evaluation of criteria for microbiological diagnosis
berg JM, Ilstrup DM, Osmon DR. Staphylococcus aureus
of prosthetic-joint infection at revision arthroplasty. The
prosthetic joint infection treated with debridement and
OSIRIS Collaborative Study Group. J Clin Microbiol
prosthesis retention. Clin Infect Dis 1997; 24(5): 914-9.
1998; 36(10): 2932-9.
Bratzler DW, Houck PM. Antimicrobial prophylaxis for
Banit DM, Kaufer H, Hartford JM. Intraoperative frozen
surgery: an advisory statement from the National Surgi-
section analysis in revision total joint arthroplasty. Clin
cal Infection Prevention Project. Clin Infect Dis 2004;
Orthop 2002; (401): 230-8.
38(12): 1706-15.
Barnes S, Salemi C, Fithian D, Akiyama L, Barron D, Eck
Burger RR, Basch T, Hopson CN. Implant salvage in infected
E, Hoare K. An enhanced benchmark for prosthetic joint
total knee arthroplasty. Clin Orthop 1991; (273): 105-12.
replacement infection rates. Am J Infect Control 2006;
Byrne DJ, Napier A, Phillips G, Cuschieri A. Effects of
34(10): 669-72.
whole body disinfection on skin flora in patients under-
Barrack RL, Engh G, Rorabeck C, Sawhney J, Woolfrey M.
going elective surgery. J Hosp Infect 1991; 17(3): 217-
Patient satisfaction and outcome after septic versus asep-
tic revision total knee arthroplasty. J Arthroplasty 2000;
Caffrey AR, Quilliam BJ, LaPlante KL. Risk factors associ-
15(8): 990-3.
ated with mupirocin resistance in meticillin-resistant Sta-
Bengtson S, Knutson K, Lidgren L. Treatment of infected
phylococcus aureus. J Hosp Infect 2010; 76(3): 206-10.
knee arthroplasty. Clin Orthop 1989; (245): 173-8.
Cahill JL, Shadbolt B, Scarvell JM, Smith PN. Quality of
Bengtson S, Knutson K. The infected knee arthroplasty. A
life after infection in total joint replacement. J Orthop
6-year follow-up of 357 cases. Acta Orthop Scand 1991;
Surg (Hong Kong) 2008; 16(1): 58-65.
62(4): 301-11.
Carlsson AK, Lidgren L, Lindberg L. Prophylactic antibiot-
Berbari EF, Hanssen AD, Duffy MC, Steckelberg JM, Ilstrup
ics against early and late deep infections after total hip
DM, Harmsen WS, Osmon DR. Risk factors for pros-
replacements. Acta Orthop Scand 1977; 48(4): 405-10.
thetic joint infection: case-control study. Clin Infect Dis
Charnley J. Low Friction Arthroplasty of the Hip. Springer-
1998; 27(5): 1247-54.
Verlag: Berlin Heidelberg New York 1979.
Berbari EF, Osmon DR, Carr A, Hanssen AD, Baddour
Cierny G, 3rd, DiPasquale D. Periprosthetic total joint infec-
LM, Greene D, Kupp LI, Baughan LW, Harmsen WS,
tions: staging, treatment, and outcomes. Clin Orthop
Mandrekar JN, Therneau TM, Steckelberg JM, Virk A,
2002; (403): 23-8.
Wilson WR. Dental procedures as risk factors for pros-thetic hip or knee infection: a hospital-based prospective
Coenye T, Nelis HJ. In vitro and in vivo model systems to
case-control study. Clin Infect Dis 2010; 50(1): 8-16.
study microbial biofilm formation. J Microbiol Methods 2010.
Anna Stefánsdóttir
Cohen JC, Hozack WJ, Cuckler JM, Booth RE, Jr. Two-
Font-Vizcarra L, Garcia S, Martinez-Pastor JC, Sierra JM,
stage reimplantation of septic total knee arthroplasty.
Soriano A. Blood culture flasks for culturing synovial
Report of three cases using an antibiotic-PMMA spacer
fluid in prosthetic joint infections. Clin Orthop 2010;
block. J Arthroplasty 1988; 3(4): 369-77.
(468): 2238-43.
Conway JD, Mont MA, Bezwada HP. Arthrodesis of the
Fulkerson E, Valle CJ, Wise B, Walsh M, Preston C, Di
knee. J Bone Joint Surg Am 2004; 86-A(4): 835-48.
Cesare PE. Antibiotic susceptibility of bacteria infecting
Cuñé J, Soriano A, Martinez JC, Garcia S, Mensa J. A super-
total joint arthroplasty sites. J Bone Joint Surg Am 2006;
ficial swab culture is useful for microbiologic diagnosis
88(6): 1231-7.
in acute prosthetic joint infections. Clin Orthop 2009;
Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB,
(467): 531-5.
Havelin LI. Early failures among 7,174 primary total
Cuzick J. A Wilcoxon-type test for trend. Stat Med 1985;
knee replacements: a follow-up study from the Nor-
wegian Arthroplasty Register 1994-2000. Acta Orthop Scand 2002; 73(2): 117-29.
DKR. Dansk Knæalloplastikregister Årsrapport 2009. Avail-
able at www.dkar.dk. Accessed October 28, 2010.
Galat DD, McGovern SC, Larson DR, Harrington JR, Hans-
sen AD, Clarke HD. Surgical treatment of early wound
De Man FH, Graber P, Luem M, Zimmerli W, Ochsner PE,
complications following primary total knee arthroplasty.
Sendi P. Broad-range PCR in selected episodes of pros-
J Bone Joint Surg Am 2009; 91(1): 48-54.
thetic joint infection. Infection 2009; 37(3): 292-4.
Gardner J, Gioe TJ, Tatman P. Can This prosthesis be saved?:
Deirmengian C, Hallab N, Tarabishy A, Della Valle C,
Implant salvage attempts in infected primary TKA. Clin
Jacobs JJ, Lonner J, Booth RE, Jr. Synovial fluid biomar-
Orthop 2010 Jun 11. [Epub ahead of print].
kers for periprosthetic infection. Clin Orthop 2010; (468): 2017-23.
Giles JT, Bartlett SJ, Gelber AC, Nanda S, Fontaine K,
Ruffing V, Bathon JM. Tumor necrosis factor inhibi-
Del Pozo JL, Patel R. Clinical practice. Infection associated
tor therapy and risk of serious postoperative orthopedic
with prosthetic joints. N Engl J Med 2009; 361(8): 787-
infection in rheumatoid arthritis. Arthritis Rheum 2006;
55(2): 333-7.
den Broeder AA, Creemers MC, Fransen J, de Jong E, de
Grogan TJ, Dorey F, Rollins J, Amstutz HC. Deep sepsis fol-
Rooij DJ, Wymenga A, de Waal-Malefijt M, van den
lowing total knee arthroplasty. Ten-year experience at the
Hoogen FH. Risk factors for surgical site infections and
University of California at Los Angeles Medical Center.
other complications in elective surgery in patients with
J Bone Joint Surg Am 1986; 68(2): 226-34.
rheumatoid arthritis with special attention for anti-tumor necrosis factor: a large retrospective study. J Rheumatol
Hall-Stoodley L, Stoodley P. Evolving concepts in biofilm
2007; 34(4): 689-95.
infections. Cell Microbiol 2009; 11(7): 1034-43.
Dowsey MM, Choong PF. Obese diabetic patients are at sub-
Hebert CK, Williams RE, Levy RS, Barrack RL. Cost of
stantial risk for deep infection after primary TKA. Clin
treating an infected total knee replacement. Clin Orthop
Orthop 2009; (467): 1577-81.
1996; (331): 140-5.
Dunbar MJ, Robertsson O, Ryd L. What's all that noise? The
Hellmann M, Mehta SD, Bishai DM, Mears SC, Zenilman
effect of co-morbidity on health outcome questionnaire
JM. The estimated magnitude and direct hospital costs of
results after knee arthroplasty. Acta Orthop Scand 2004;
prosthetic joint infections in the United States, 1997 to
75(2): 119-26.
2004. J Arthroplasty 2010; 25(5): 766-71.
Engesaeter LB, Lie SA, Espehaug B, Furnes O, Vollset SE,
Hennessy MJ. Infection of a total knee arthroplasty by Cand-
Havelin LI. Antibiotic prophylaxis in total hip arthro-
ida parapsilosis. A case report of successful treatment by
plasty: effects of antibiotic prophylaxis systemically and
joint reimplantation with a literature review. Am J Knee
in bone cement on the revision rate of 22,170 primary
Surg 1996; 9(3): 133-6.
hip replacements followed 0-14 years in the Norwegian
Hill C, Flamant R, Mazas F, Evrard J. Prophylactic cefazo-
Arthroplasty Register. Acta Orthop Scand 2003; 74(6):
lin versus placebo in total hip replacement. Report of a
multicentre double-blind randomised trial. Lancet 1981;
Ericson C, Lidgren L, Lindberg L. Cloxacillin in the prophy-
1(8224): 795-6.
laxis of postoperative infections of the hip. J Bone Joint
Hoad-Reddick DA, Evans CR, Norman P, Stockley I. Is
Surg Am 1973; 55(4): 808-13, 43.
there a role for extended antibiotic therapy in a two-stage
Fedorka CJ, Chen AF, McGarry WM, Parvizi J, Klatt BA.
revision of the infected knee arthroplasty? J Bone Joint
Functional Ability After Above-the-knee Amputation for
Surg Br 2005; 87(2): 171-4.
Infected Total Knee Arthroplasty. Clin Orthop 2010 Oct
Hofmann AA, Kane KR, Tkach TK, Plaster RL, Camargo
1. [Epub ahead of print].
MP. Treatment of infected total knee arthroplasty using
Fehring TK, Odum S, Calton TF, Mason JB. Articulating
an articulating spacer. Clin Orthop 1995; (321): 45-54.
versus static spacers in revision total knee arthroplasty
Hoiby N, Bjarnsholt T, Givskov M, Molin S, Ciofu O. Anti-
for sepsis. The Ranawat Award. Clin Orthop 2000; (380):
biotic resistance of bacterial biofilms. Int J Antimicrob
Agents 2010; 35(4): 322-32.
Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy
Hope PG, Kristinsson KG, Norman P, Elson RA. Deep
TH. The obesity epidemic: its effect on total joint arthro-
infection of cemented total hip arthroplasties caused by
plasty. J Arthroplasty 2007; 22(6 Suppl 2): 71-6.
coagulase-negative staphylococci. J Bone Joint Surg Br 1989; 71(5): 851-5.
THE INFECTED KNEE ARTHROPLASTY
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG.
Kurd MF, Ghanem E, Steinbrecher J, Parvizi J. Two-stage
CDC definitions of nosocomial surgical site infections,
exchange knee arthroplasty: does resistance of the infect-
1992: a modification of CDC definitions of surgical
ing organism influence the outcome? Clin Orthop 2010;
wound infections. Infect Control Hosp Epidemiol 1992;
468(8): 2060-6.
13(10): 606-8.
Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E,
Hughes JG, Vetter EA, Patel R, Schleck CD, Harmsen S,
Karrholm J, Garellick G, Havelin LI, Furnes O, Malchau
Turgeant LT, Cockerill FR, 3rd. Culture with BACTEC
H, Lau E. Future clinical and economic impact of revi-
Peds Plus/F bottle compared with conventional methods
sion total hip and knee arthroplasty. J Bone Joint Surg
for detection of bacteria in synovial fluid. J Clin Micro-
Am 2007; 89 Suppl 3: 144-51.
biol 2001; 39(12): 4468-71.
Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J.
Huotari K, Lyytikainen O, Ollgren J, Virtanen MJ, Seitsalo
Infection burden for hip and knee arthroplasty in the
S, Palonen R, Rantanen P. Disease burden of prosthetic
United States. J Arthroplasty 2008; 23(7): 984-91.
joint infections after hip and knee joint replacement in
Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J.
Finland during 1999-2004: capture-recapture estimation.
Prosthetic joint infection risk after TKA in the Medicare
J Hosp Infect 2010; 75(3): 205-8.
population. Clin Orthop 2010; 468(1): 52-6.
Husted H, Toftgaard Jensen T. Clinical outcome after treat-
Laffer RR, Graber P, Ochsner PE, Zimmerli W. Outcome
ment of infected primary total knee arthroplasty. Acta
of prosthetic knee-associated infection: evaluation of 40
Orthop Belg 2002; 68(5): 500-7.
consecutive episodes at a single centre. Clin Microbiol
Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison
Infect 2006; 12(5): 433-9.
of four models of total knee-replacement prostheses. J
Lasa I. Towards the identification of the common features of
Bone Joint Surg Am 1976; 58(6): 754-65.
bacterial biofilm development. Int Microbiol 2006; 9(1):
Insall JN, Thompson FM, Brause BD. Two-stage reimplan-
tation for the salvage of infected total knee arthroplasty.
Lavernia C, Lee DJ, Hernandez VH. The increasing financial
J Bone Joint Surg Am 1983; 65(8): 1087-98.
burden of knee revision surgery in the United States. Clin
Jefferson KK. What drives bacteria to produce a biofilm?
Orthop 2006; (446): 221-6.
FEMS Microbiol Lett 2004; 236(2): 163-73.
Lawson MC, Hoth KC, Deforest CA, Bowman CN, Anseth
Johnson AJ, Daley JA, Zywiel MG, Delanois RE, Mont MA.
KS. Inhibition of Staphylococcus epidermidis biofilms
Preoperative chlorhexidine preparation and the incidence
using polymerizable vancomycin derivatives. Clin
of surgical site infections after hip arthroplasty. J Arthro-
Orthop 2010; 468(8): 2081-91.
plasty 2010; 25(6 Suppl): 98-102.
Leone JM, Hanssen AD. Management of infection at the site
Jämsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors
of a total knee arthroplasty. J Bone Joint Surg Am 2005;
for infection after knee arthroplasty. A register-based
87(10): 2335-48.
analysis of 43,149 cases. J Bone Joint Surg Am 2009a;
Lewis K. Riddle of biofilm resistance. Antimicrob Agents
91(1): 38-47.
Chemother 2001; 45(4): 999-1007.
Jämsen E, Stogiannidis I, Malmivaara A, Pajamaki J,
Lewis K. Persister cells, dormancy and infectious disease.
Puolakka T, Konttinen YT. Outcome of prosthesis
Nat Rev Microbiol 2007; 5(1): 48-56.
exchange for infected knee arthroplasty: the effect of treatment approach. Acta Orthop 2009b; 80(1): 67-77.
Lidwell OM, Elson RA, Lowbury EJ, Whyte W, Blowers
R, Stanley SJ, Lowe D. Ultraclean air and antibiotics
Jämsen E, Nevalainen P, Kalliovalkama J, Moilanen T.
for prevention of postoperative infection. A multicenter
Preoperative hyperglycemia predicts infected total knee
study of 8,052 joint replacement operations. Acta Orthop
replacement. Eur J Intern Med 2010; 21(3): 196-201.
Scand 1987; 58(1): 4-13.
Kamme C, Lidgren L, Lindberg L, Mardh PA. Anaerobic
Love C, Marwin SE, Palestro CJ. Nuclear medicine and
bacteria in late infections after total hip arthroplasty.
the infected joint replacement. Semin Nucl Med 2009;
Scand J Infect Dis 1974; 6(2): 161-5.
39(1): 66-78.
Kamme C, Lindberg L. Aerobic and anaerobic bacteria in
Mabry TM, Jacofsky DJ, Haidukewych GJ, Hanssen AD.
deep infections after total hip arthroplasty: differential
Comparison of intramedullary nailing and external fixa-
diagnosis between infectious and non-infectious loosen-
tion knee arthrodesis for the infected knee replacement.
ing. Clin Orthop 1981; (154): 201-7.
Clin Orthop 2007; (464): 11-5.
Kilgus DJ, Howe DJ, Strang A. Results of periprosthetic hip
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR.
and knee infections caused by resistant bacteria. Clin
Guideline for prevention of surgical site infection, 1999.
Orthop 2002; (404): 116-24.
Hospital Infection Control Practices Advisory Commit-
Knutson K, Hovelius L, Lindstrand A, Lidgren L. Arthro-
tee. Infect Control Hosp Epidemiol 1999; 20(4): 250-78;
desis after failed knee arthroplasty. A nationwide mul-
ticenter investigation of 91 cases. Clin Orthop 1984;
Marculescu CE, Cantey JR. Polymicrobial prosthetic joint
(191): 202-11.
infections: risk factors and outcome. Clin Orthop 2008;
Kosters K, van Crevel R, Sturm PD, Willem Schreurs B, de
(466): 1397-404.
Waal Malefijt MC, van Kampen A, Kullberg BJ. Treat-
Mariani BD, Martin DS, Levine MJ, Booth RE, Jr., Tuan RS.
ment of knee prosthesis infections: evaluation of 15
The Coventry Award. Polymerase chain reaction detec-
patients over a 5-year period. Int Orthop 2009; 33(5):
tion of bacterial infection in total knee arthroplasty. Clin
Orthop 1996; (331): 11-22.
Anna Stefánsdóttir
McPherson EJ, Tontz W, Jr., Patzakis M, Woodsome C,
Rasul AT, Jr., Tsukayama D, Gustilo RB. Effect of time of
Holtom P, Norris L, Shufelt C. Outcome of infected total
onset and depth of infection on the outcome of total knee
knee utilizing a staging system for prosthetic joint infec-
arthroplasty infections. Clin Orthop 1991; (273): 98-104.
tion. Am J Orthop (Belle Mead NJ) 1999; 28(3): 161-5.
Robertsson O, Dunbar M, Knutson K, Lewold S, Lidgren
Meehan J, Jamali AA, Nguyen H. Prophylactic antibiotics in
L. Validation of the Swedish Knee Arthroplasty Regis-
hip and knee arthroplasty. J Bone Joint Surg Am 2009;
ter: a postal survey regarding 30,376 knees operated on
91(10): 2480-90.
between 1975 and 1995. Acta Orthop Scand 1999; 70(5):
Meermans G, Haddad FS. Is there a role for tissue biopsy
in the diagnosis of periprosthetic infection? Clin Orthop
Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren
2010; (468): 1410-7.
L. Patient satisfaction after knee arthroplasty: a report
Morgan M, Black J, Bone F, Fry C, Harris S, Hogg S,
on 27,372 knees operated on between 1981 and 1995 in
Holmes A, Hughes S, Looker N, McIlvenny G, Nixon
Sweden. Acta Orthop Scand 2000a; 71(3): 262-7.
J, Nolan J, Noone A, Reilly J, Richards J, Smyth E,
Robertsson O, Lewold S, Knutson K, Lidgren L. The Swed-
Howard A. Clinician-led surgical site infection surveil-
ish Knee Arthroplasty Project. Acta Orthop Scand
lance of orthopaedic procedures: a UK multi-centre pilot
2000b; 71(1): 7-18.
study. J Hosp Infect 2005; 60(3): 201-12.
Robertsson O, Knutson K, Lewold S, Lidgren L. The Swed-
Morgan PM, Sharkey P, Ghanem E, Parvizi J, Clohisy JC,
ish Knee Arthroplasty Register 1975-1997: an update
Burnett RS, Barrack RL. The value of intraoperative
with special emphasis on 41,223 knees operated on in
Gram stain in revision total knee arthroplasty. J Bone
1988-1997. Acta Orthop Scand 2001; 72(5): 503-13.
Joint Surg Am 2009; 91(9): 2124-9.
Saleh K, Olson M, Resig S, Bershadsky B, Kuskowski M,
Møller AM, Villebro N, Pedersen T, Tonnesen H. Effect
Gioe T, Robinson H, Schmidt R, McElfresh E. Predictors
of preoperative smoking intervention on postoperative
of wound infection in hip and knee joint replacement:
complications: a randomised clinical trial. Lancet 2002;
results from a 20 year surveillance program. J Orthop
359(9301): 114-7.
Res 2002; 20(3): 506-15.
Namba RS, Paxton L, Fithian DC, Stone ML. Obesity
Sanzén L, Walder M. Antibiotic resistance of coagulase-
and perioperative morbidity in total hip and total knee
negative staphylococci in an orthopaedic department. J
arthroplasty patients. J Arthroplasty 2005; 20(7 Suppl 3):
Hosp Infect 1988; 12(2): 103-8.
Schoifet SD, Morrey BF. Treatment of infection after total
Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR.
knee arthroplasty by debridement with retention of the
The microbiology of the infected knee arthroplasty. Int
components. J Bone Joint Surg Am 1990; 72(9): 1383-
Orthop 2010; 34(4): 505-10.
Niskanen RO, Korkala O, Pammo H. Serum C-reactive pro-
Schrama JC, Espehaug B, Hallan G, Engesaeter LB, Furnes
tein levels after total hip and knee arthroplasty. J Bone
O, Havelin LI, Fevang BT. Risk of revision for infec-
Joint Surg Br 1996; 78(3): 431-3.
tion in primary total hip and knee arthroplasty in patients
NJR. National Joint Registry for England and Wales. 7th
with rheumatoid arthritis compared with osteoarthritis:
Annual report 2010. Available at www.njrcentre.org.uk.
a prospective, population-based study on 108,786 hip
Accessed October 28, 2010.
and knee joint arthroplasties from the Norwegian Arthro-plasty Register. Arthritis Care Res (Hoboken) 2010;
Parvizi J, Ghanem E, Sharkey P, Aggarwal A, Burnett RS,
62(4): 473-9.
Barrack RL. Diagnosis of infected total knee: findings of a multicenter database. Clin Orthop 2008a; 466(11):
Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo
RB. Infection after total knee arthroplasty. A retrospec-tive study of the treatment of eighty-one infections. J
Parvizi J, Saleh KJ, Ragland PS, Pour AE, Mont MA.
Bone Joint Surg Am 1999; 81(10): 1434-45.
Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop 2008b; 79(3): 335-41.
Segreti J, Nelson JA, Trenholme GM. Prolonged suppres-
sive antibiotic therapy for infected orthopedic prosthe-
Peersman G, Laskin R, Davis J, Peterson M. Infection in
ses. Clin Infect Dis 1998; 27(4): 711-3.
total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop 2001; (392): 15-23.
Sherrell JC, Fehring TK, Odum S, Hansen E, Zmistowski
B, Dennos A, Kalore N. The Chitranjan Ranawat Award:
Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The
Fate of Two-stage Reimplantation After Failed Irrigation
incidence of deep prosthetic infections in a specialist
and Debridement for Periprosthetic Knee Infection. Clin
orthopaedic hospital: a 15-year prospective survey. J
Orthop 2010 Jun 26. [Epub ahead of print]
Bone Joint Surg Br 2006; 88(7): 943-8.
SHPR. The Swedish National Hip Arthroplasty Register.
Pollard JP, Hughes SP, Scott JE, Evans MJ, Benson MK.
Annual report 2002. Available at www.jru.orthop.gu.se.
Antibiotic prophylaxis in total hip replacement. Br Med
Accessed October 28, 2010.
J 1979; 1(6165): 707-9.
SHPR. The Swedish National Hip Arthroplasty Register.
Prokuski L. Prophylactic antibiotics in orthopaedic surgery.
Annual report 2008. Available at www.jru.orthop.gu.se.
J Am Acad Orthop Surg 2008; 16(5): 283-93.
Accessed October 28, 2010.
Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Peripros-
SKAR. The Swedish Knee Arthroplasty Register, Annual
thetic joint infection: the incidence, timing, and predis-
report 2010. Available at www.knee.se. Accessed
posing factors. Clin Orthop 2008; (466): 1710-5.
November 2, 2010.
THE INFECTED KNEE ARTHROPLASTY
Smith JK, Bumgardner JD, Courtney HS, Smeltzer MS,
Van Meirhaeghe J, Verdonk R, Verschraegen G, Myny P,
Haggard WO. Antibiotic-loaded chitosan film for infec-
Paeme G, Claessens H. Flucloxacillin compared with
tion prevention: A preliminary in vitro characterization.
cefazolin in short-term prophylaxis for clean orthopedic
J Biomed Mater Res B Appl Biomater 2010; 94(1): 203-
surgery. Arch Orthop Trauma Surg 1989; 108(5): 308-13.
van Rijen MM, Bonten M, Wenzel RP, Kluytmans JA. Intra-
Sofka CM, Potter HG, Adler RS, Pavlov H. Musculoskel-
nasal mupirocin for reduction of Staphylococcus aureus
etal imaging update: current applications of advanced
infections in surgical patients with nasal carriage: a sys-
imaging techniques to evaluate the early and long-term
tematic review. J Antimicrob Chemother 2008; 61(2):
complications of patients with orthopedic implants. HSS
J 2006; 2(1): 73-7.
Wasielewski RC, Barden RM, Rosenberg AG. Results of
Soriano A, Garcia S, Bori G, Almela M, Gallart X, Macule
different surgical procedures on total knee arthroplasty
F, Sierra J, Martinez JA, Suso S, Mensa J. Treatment of
infections. J Arthroplasty 1996; 11(8): 931-8.
acute post-surgical infection of joint arthroplasty. Clin
White J, Kelly M, Dunsmuir R. C-reactive protein level after
Microbiol Infect 2006; 12(9): 930-3.
total hip and total knee replacement. J Bone Joint Surg
Stenhem M, Ortqvist A, Ringberg H, Larsson L, Olsson-
Br 1998; 80(5): 909-11.
Liljequist B, Haeggman S, Ekdahl K. Epidemiology of
Whiteside LA, Peppers M, Nayfeh TA, Roy ME. Methicil-
methicillin-resistant Staphylococcus aureus (MRSA) in
lin-resistant Staphylococcus aureus in TKA treated with
Sweden 2000-2003, increasing incidence and regional
revision and direct intraarticular antibiotic infusion. Clin
differences. BMC Infect Dis 2006; 6: 30.
Orthop 2010 Apr 14. [Epub ahead of print].
Teeny SM, Dorr L, Murata G, Conaty P. Treatment of
Vince KG, Abdeen A. Wound problems in total knee arthro-
infected total knee arthroplasty. Irrigation and debride-
plasty. Clin Orthop 2006; (452): 88-90.
ment versus two-stage reimplantation. J Arthroplasty 1990; 5(1): 35-9.
von Eiff C, Peters G, Heilmann C. Pathogenesis of infections
due to coagulase-negative staphylococci. Lancet Infect
Tomita M, Motokawa S. Effects of air tourniquet on the
Dis 2002; 2(11): 677-85.
antibiotics concentration, in bone marrow, injected just before the start of operation. Mod Rheumatol 2007;
Wymenga A, van Horn J, Theeuwes A, Muytjens H, Slooff
17(5): 409-12.
T. Cefuroxime for prevention of postoperative coxitis. One versus three doses tested in a randomized multi-
Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steck-
center study of 2,651 arthroplasties. Acta Orthop Scand
elberg JM, Patel R. Synovial fluid leukocyte count and
1992a; 63(1): 19-24.
differential for the diagnosis of prosthetic knee infection. Am J Med 2004; 117(8): 556-62.
Wymenga AB, van Horn JR, Theeuwes A, Muytjens HL,
Slooff TJ. Perioperative factors associated with septic
Tunney MM, Patrick S, Curran MD, Ramage G, Hanna D,
arthritis after arthroplasty. Prospective multicenter study
Nixon JR, Gorman SP, Davis RI, Anderson N. Detection
of 362 knee and 2,651 hip operations. Acta Orthop Scand
of prosthetic hip infection at revision arthroplasty by
1992b; 63(6): 665-71.
immunofluorescence microscopy and PCR amplification of the bacterial 16S rRNA gene. J Clin Microbiol 1999;
Zimmerli W, Ochsner PE. Management of infection associ-
37(10): 3281-90.
ated with prosthetic joints. Infection 2003; 31(2): 99-108.
Walenkamp G. Gentamicin PMMA beads and other ocal
Zimmerli W, Sendi P. Antibiotics for prevention of peripros-
antibiotic carriers in two-stage revision of total knee
thetic joint infection following dentistry: time to focus on
infection: a review. J Chemother 2001; 13(1): 66-72.
data. Clin Infect Dis 2010; 50(1): 17-9.
Walker RH, Schurman DJ. Management of infected total
Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE.
knee arthroplasties. Clin Orthop 1984; (186): 81-9.
Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: a randomized control-
Walldius B. Arthroplasty of the knee joint employing an
led trial. Foreign-Body Infection (FBI) Study Group.
acrylic prosthesis. Acta Orthop Scand 1953; 23(2): 121-
JAMA 1998; 279(19): 1537-41.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infec-
Walldius B. Arthroplasty of the knee using an endoprosthe-
tions. N Engl J Med 2004; 351(16): 1645-54.
sis. Acta Orthop Scand Suppl 1957; 24: 1-112.
van Kasteren ME, Mannien J, Ott A, Kullberg BJ, de Boer
AS, Gyssens IC. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clin Infect Dis 2007; 44(7): 921-7.
Source: http://www.myknee.se/pdf/article186.pdf
The Brotherhood Synagogue 28 Gramercy Park South new york, ny 10003 Phone (212) 674-5750 Fax (212) 505-6707 Volume XXXiV number Xi Av / Elul 5776 September 2016 Elie Wieselzt"l: Words and Memories by rabbi daniel Alder FridAy, SEPTEMBEr 2, 7:30 pm SATurdAy, SEPTEMBEr 3, 9:30 am Among the more poignant remembrances "Sir," I said, "you speak of Christ, Christians
International Journal of Applied Research in Natural Products Vol. 7 (4), pp. 11-25. Directory of Open Access Journals ©2008-2014. IJARNP-HS Publication Original Research Extraction and characterization of candidate bioactive compounds in different tissues from salmon (Salmo salar) Falkenberg SS*1, Mikalsen S-O2, Joensen H2, Stagsted J3, Nielsen HH1 1Technical University of Denmark, National Food Institute, Søltofts Plads bldg. 221, 2800 Kgs. Lyngby, Denmark 2University of the Faroe Islands, Department of Science and Technology, Nóatún 3 FO-100 Tórshavn, the Faroe Islands 3Department of Food Science, Aarhus University, Blichers Allé 20, 8830 Tjele, Denmark Summary. There is an interest in bioprospecting organisms from the aquatic environment to find novel bioactive compounds with health promoting or other functional properties. The aim of this study was to evaluate extracts from untreated and heat-treated salmon tissues for their radical scavenging activities and for their ability to inhibit activity of the proteases angiotensin I-converting enzyme (ACE) and dipeptidyl peptidase 4 (DPP-4). In vitro assays were used to detect these activities and the corresponding candidate bioactive compounds were characterized by LC-MS/MS. Radical scavenging activity was detected in <10kDa extracts of gills, belly flap muscle and skin with EC50 values of 39, 82 and 100 µg/mL,