Assets.prod.vetlearn.com.s3.amazonaws.com

In collaboration with the American College of Veterinary Surgeons
Treating Navicular Syndrome in
Equine Patients*
R. Wayne Waguespack, DVM, MS, DACVS
R. Reid Hanson, DVM, DACVS, DACVECC
Auburn University
Abstract: Navicular syndrome is a chronic, progressive condition affecting the navicular bone and bursa, deep digital flexor tendon
(DDFT), and associated soft tissue structures composing the navicular apparatus. The treatment options for navicular syndrome are
as varied as the proposed causes of the condition. The severity of clinical signs, intended use and workload of the horse, and owner compliance with therapy are important considerations in developing a treatment plan. Nonsurgical treatment of navicular syndrome consists of rest, hoof balance and corrective trimming/shoeing, and medical therapy, including administration of systemic antiinflam-matories, hemorheologic medications, and intraarticular medications. While surgical therapy can include desmotomy of the col ateral
(suspensory) ligaments of the navicular bone, palmar digital neurectomy is more commonly performed when medical therapy is inef-
fective. Recently, adjunct therapies, such as acupuncture and extracorporeal shock wave therapy, have also been used to treat horses with navicular syndrome. Because of the wide range of pathologic changes and the lack of a definitive cure associated with navicular syndrome, treatment is directed toward the individual horse, focusing on the management of clinical signs to al eviate stress and retard degenerative changes of the navicular bursal and navicular regions.
Navicular syndrome is a chronic progressive condi- the surrounding soft tissues have been reported, primarily
tion affecting the navicular bone and bursa as well involving the palmar fibrocartilage of the navicular bone,
as the associated soft tissue structures1 (FIGURE 1). its underlying subchondral and trabecular bone, and the
This article discusses treatment options and future research apposing DDFT. In addition, erosions and fibrillation of the
involving navicular syndrome.
fibrocartilage, remodeling of the underlying subchondral
The treatment options for navicular syndrome are as var- and trabecular bone, palmar cortical bone erosion, DDFT
ied as the proposed causes of the condition. As new ideas fibrillation, core lesions, and adhesions have been recog-regarding the etiology have been proposed, new treatment nized.3–5 These changes are remarkably similar to those seen regimens have followed. Recently, with the use of computed in osteoarthritis; however, in navicular syndrome, the pal-
tomography (CT) and magnetic resonance imaging (MRI), mar fibrocartilage of the navicular bone and the apposing
it appears that the deep digital flexor tendon (DDFT) at DDFT are involved instead of two apposing hyaline carti-
the level of the navicular bone may play a more significant lage surfaces.
role than previously understood1,2 (FIGURE 2). Despite new Knowledge of these changes may eventually help clarify
information regarding navicular syndrome, many treatments why some treatment regimens produce clinical improve-remain based on modification of pain rather than elimina- ment and allow development of more specific therapeutic
tion or reduction of pathologic processes. In patients with alternatives. In lieu of this, treatment options are focused navicular syndrome, changes in the navicular bone and on management of clinical signs and should be designed to
alleviate stress on the navicular region and prevent or retard
*A companion article, "Navicular Syndrome in Equine Patients:
degenerative changes within the navicular bone and bursal
Anatomy, Causes, and Diagnosis," appeared in the December 2010
Vetlearn.com January 2011 Compendium: Continuing Education for Veterinarians® E1
Copyright 2011 MediMedia Animal Health. This document is for internal purposes only. Reprinting or posting on an external website without written permission from MMAH is a violation of copyright laws.

The severity of clinical signs, the horse's intended use and workload, and the owner's compliance with therapy are
important considerations in developing a treatment plan.
Young horses and horses with less severe clinical signs
are often candidates for conservative therapy. Nonsurgical treatment of navicular syndrome consists of rest, hoof bal-ance and corrective trimming/shoeing, and medical therapy, including systemic antiinflammatories, hemorheologic med-ications, and intraarticular medications.6–8
RestOne of the most overlooked components of treatment is rest.
Continued stress on the navicular region leads to structural
failure and eventual breakdown. Time is necessary to allow soft tissue inflammation to subside and bone remodeling to take place. The time necessary to reduce inflammation var-ies on an individual basis. Absolute confinement is contrain-dicated; pasture or paddock turnout is sufficient.
Corrective Shoeing and Hoof Balance Careful evaluation of foot conformation and balance is the
focal point in nonsurgical treatment of navicular syndrome. Many horses respond to correction of hoof abnormalities.9
The goal is to reduce forces on the navicular region by (1) cor-
recting hoof balance and the hoof–pastern axis, (2) allowing the use of all weightbearing structures of the hoof by main-taining the heel mass and protecting the palmar aspect of
The navicular bursa (black arrow), distal interphalangeal
the foot from concussion, and (3) decreasing the work of the
joint (blue arrow), deep digital flexor tendon, impar liga-
moving foot by either shortening the toe length of the foot to
ment, and collateral sesmoidean ligament. (NB = navicular
permit an easier breakover or rolling the toe of the shoe.
bone; PII = second phalanx; PIII = third phalanx)
Horses with navicular syndrome often have unbalanced
hooves consisting of long toes with low, underrun, and
contracted heels (FIGURE 3). One of the first requirements
of hoof balance is hoof–pastern alignment. Proper hoof–
pastern alignment is assumed if a straight line can be drawn
through the dorsal pastern and dorsal hoof wall (FIGURE
3). The foot should be trimmed to maintain heel mass and
shorten the toe to facilitate breakover if the hooves are char-
acterized by long toes. Use of the so-called four-point or
natural-balance trim has recently been favored by some clinicians, but the same principles of breakover can prob-
ably be achieved with more traditional trimming if the toe is shortened sufficiently. Radical changes in foot trimming
Surgical Views is a col aborative series between the American
may temporarily increase lameness; therefore, correct foot
Col ege of Veterinary Surgeons (ACVS) and Compendium.
balance may need to be achieved in stages.
All Surgical Views articles are peer-reviewed by ACVS
In principle, a hoof with proper hoof–pastern alignment
has the appropriate amount of tension or force exerted on the navicular bone by the DDFT. In horses with low heels,
To locate a diplomate, ACVS has an online directory that includes practice
setting, species emphasis, and research interests (acvs.org/Veterinary
correct alignment can be established with selective trimming
or, more commonly, by elevating the heels with a wedge-heel
E2 Compendium: Continuing Education for Veterinarians® January 2011 Vetlearn.com
Advanced imaging modalities such as MRI and CT have helped veterinarians
realize that navicular syndrome involves more than just the navicular bone in horses.
(A) MRI of the navicular region. Cross-sectional and longitudinal
views are shown. (B) CT scan of the navicular region. Based on
the visible asymmetry, an erosive lesion is noted in the navicu-
lar bone.
balance. This is determined either by obtaining a dorsopal-mar radiograph of the foot or watching the horse walk to ensure that the medial and lateral aspects of the hoof hit the ground simultaneously. If the hoof cannot be trimmed to establish normal hoof–pastern alignment or lateromedial balance, shoes can be applied to encourage the hoof to grow correctly. Many types of shoes have been recommended for horses with navicular syndrome. Full-bar, egg-bar, natural balance, and wide-web aluminum or steel shoes with or
without elevated heels have been used to support the heels
and move the weightbearing axis in a palmar direction in
horses with low, collapsed, and underrun heels (FIGURE 4).
A recent study showed that using egg-bar shoes with no
heel elevation in clinically normal Dutch Warmblood horses
shoe.9 In a study of normal Dutch Warmblood horses, heel with well-conformed feet did not reduce the force on the elevation with a 6° wedge reduced the maximal force on the navicular bone compared with using regular flat shoes.10 navicular bone by 24% compared with use of flat shoes.10 In However, these findings cannot necessarily be translated to another study, force-plate analysis indicated that lameness sig- lame horses with less-than-ideal foot conformation. In the nificantly decreased in horses with navicular syndrome that same study, heel wedges did reduce the force on the navic-
were shod to produce a 3° heel elevation alone or in com- ular bone compared with flat shoes.10 In a study evaluat-
bination with phenylbutazone administration.11 Lateromedial ing 55 horses with clinically diagnosed navicular syndrome, radiographs may be necessary to demonstrate whether a 53% had permanent relief of lameness 12 to 40 months after horse needs more or less heel elevation. If the horse's lame- application of egg-bar shoes.12 In another study, horses shod ness worsens after elevation of the toe using the wedge test, with egg-bar shoes showed histomorphometric evidence of some degree of heel elevation may be beneficial.
altered navicular bone modeling compared with untreated
The hoof should also be maintained in medial-to-lateral controls.13 In any case, shoes should be set (1) beyond the
Vetlearn.com January 2011 Compendium: Continuing Education for Veterinarians® E3

Unbalanced hooves and proper hoof–pastern alignment.
(A) Unbalanced hooves (long toes and low, underrun heels) of a horse with navicular syndrome. Note the medial-to-lateral imbal-
ance in the horse's feet. One of the first requirements for hoof balance is hoof–pastern alignment. (B) Proper hoof–pastern align-
ment is assumed if a straight line can be drawn through the bony column of the phalanges. The dorsal hoof wall should be parallel
to the dorsal aspect of the pastern. A line bisecting the third metacarpal bone should reach the ground at the weightbearing part of
the heel.
heels to provide heel support and (2) full or wide to allow nolone acetonide, betamethasone sodium phosphate) have proper hoof expansion.7,10
been injected into the navicular bursa and the distal inter-
phalangeal joint (DIPJ) to treat navicular syndrome, and the
results have varied.7,14 These powerful antiinflammatories
Anti nflammatories
are routinely used in combination with sodium hyaluronate
to control clinical signs associated with navicular syndrome.
Corticosteroids (e.g., methylprednisolone acetate, triamci- Most clinicians medicate the DIPJ when treating navicular syn-
E4 Compendium: Continuing Education for Veterinarians® January 2011 Vetlearn.com


drome.15 Medications injected into the
DIPJ, which is near the navicular bursa, have been shown to diffuse to the navicular region. A study by Pauwels et al15 showed that clinically effective concentrations of methylprednisolone and triamcinolone diffused between
the DIPJ and the navicular bursa. This
is also supported by the response to
treatment of clinical cases of navicular syndrome.
Over time, some horses stop
responding to intraarticular therapy of the DIPJ. Intrabursal therapy may provide another option for reducing inflammation in the navicular region of the foot. One study showed that 80% of horses that no longer responded to traditional therapy for navicular syndrome (i.e., corrective shoeing, administration of systemic antiinflam-matories, intraarticular therapy of the DIPJ) were sound 2 weeks after intrabursal injections of corticoster-oids, sodium hyaluronate, and amika-cin.16 The mean duration of soundness
Full-bar, egg-bar, and wide-web aluminum or steel shoes have been used to
support the heels and move the weightbearing axis in a palmar direction in horses with
in this study was 4.5 months.
low, collapsed, and underrun heels.
In recent years, interleukin-1 recep-
tor antagonist protein (IRAP) therapy
(Vet Arthrex Biosystems, Bonita Springs, FL) has been used ical situations. NSAID toxicosis may develop with long-term
increasingly in veterinary practices to treat osteoarthri- use of certain NSAIDs because of the nonselective inhibi-
tis in horses. Several studies have investigated the effects tion of cyclooxygenases 1 and 2. In a study comparing oral
of IRAP therapy for this purpose.17–19 While the efficacy of firocoxib (a highly selective cyclooxygenase-2 inhibitor) IRAP therapy for treating navicular syndrome has not been and oral phenylbutazone in controlling pain associated with investigated, some clinicians have noted positive effects naturally occurring osteoarthritis, there was no statistically from IRAP injections either in the DIPJ or directly in the significant difference.24navicular bursa. IRAP is a naturally occurring protein that Other drugs with potential antiinflammatory proper-works by occupying receptor sites on the membrane of car-
ties that may be useful for treating navicular syndrome are
tilage cells, preventing the normal cytokine-initiated inflam- glucosamine–chondroitin sulfate compounds, polysulfated matory cascade.19,20 Blockage of matrix metalloproteinases glycosaminoglycans (PSGAGs), and sodium hyaluronate.16,25 and cytokines (e.g., interleukin-1) reduces their degenerative Glucosamine–chondroitin sulfate compounds are given
effects on cartilage, preventing degenerative joint disease orally, sodium hyaluronate can be given intravenously or and osteoarthritis.18,19,21–23
intrasynovially, and PSGAGs can be given intrasynovially or intramuscularly. Administration of glucosamine–chondroitin
sulfate compounds and intramuscular PSGAGs has been
NSAIDs have been the mainstay of navicular syndrome shown to reduce clinical signs associated with navicular
therapy for many years.7,8,11 The analgesic and antiinflamma- syndrome.25–27 These medications are effective only while tory properties of NSAIDs make them attractive therapeutic they are administered. Lameness reappears after the therapy agents. Phenylbutazone is the most commonly used NSAID. is discontinued. The bioavailability of glucosamine–chon-
Flunixin meglumine, diclofenac, carprofen, naproxen, keto- droitin sulfate compounds in horses had been questioned, profen, meclofenamic acid, and aspirin are also used in clin- but it has now been documented.28
Vetlearn.com January 2011 Compendium: Continuing Education for Veterinarians® E5

in treating navicular syndrome, the
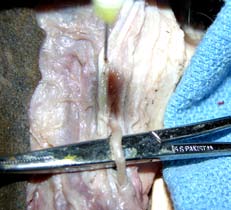
Anatomy surrounding the palmar digital nerve.
lameness scores of horses receiv-ing propentofylline significantly im-
proved.35 In a study evaluating the oral administration of pentoxifylline,
therapeutic levels were achieved in horses.36 This was not supported in an earlier study in which oral admin-
istration of pentoxifylline had no significant effects on digital blood flow to the equine foot.30 The find-ings in these two studies may be due
to the use of different dosages of
Bone Metabolism Medications
(A) The lateral aspect of the phalangeal
Bisphosphonates, such as tiludronate,
region of the distal limb. The needle is in the
are used to normalize bone metab-
ligament of the ergot, which can be incor-
rectly identified as the palmar digital nerve
olism through inhibition of bone
during neurectomy. (B) The needle is in the
resorption; however, bisphospho-
palmar digital nerve adjacent to the palmar
nates approved for horses are not
digital artery, which is elevated by the surgi-
available in the United States. Areas
cal instrument. The ligament of the ergot is
of increased bone resorption and
just dorsal to the palmar digital artery and
formation are common on radio-
graphs of horses with navicular syn-drome. Delguste et al37 showed that
tiludronate reduces bone resorption
Isoxsuprine hydrochloride (a β agonist) is a peripheral and prevents long-term osteopenia in healthy horses. Several vasodilator that has been successfully used in relieving studies have evaluated the dosages (0.1 mg/kg q24h IV for 10
the clinical signs of navicular syndrome.29,30 The drug can days versus 1 mg/kg IV in a single dose), bioavailability, and also decrease blood viscosity and platelet aggregation.31 pharmacologic effects of tiludronate in horses.38,39 In a clini-
Isoxsuprine is given orally, and numerous dosages have cal trial by Denoix et al,38 horses treated with tiludronate (1
been recommended. The specific mode of action of isoxsu- mg/kg IV in a single dose) showed significant improvement
prine in treating navicular syndrome is unknown. In a study in lameness and returned to their normal level of activity
by Ingle-Fehr and Baxter,30 oral isoxsuprine did not increase within 2 to 6 months after treatment.
blood flow to the equine foot. Isoxsuprine also binds strongly
to α adrenoreceptors and, therefore, may be active despite Surgical Therapy
insignificant but measurable levels in plasma.32,33 The drug Palmar Digital Neurectomy
may also have antiinflammatory and hemorheologic prop- Palmar digital neurectomy (PDN) involves disrupting the
erties, which may be the source of its beneficial effects in nerve supply to the palmar one-third of the hoof to alleviate
horses with navicular syndrome. A clinical trial that evalu- heel pain (FIGURES 5 and 6). PDN is considered a palliative
ated the clinical efficacy of isoxsuprine for treating navicular procedure because it only alleviates the pain associated with
syndrome in horses demonstrated a decrease in lameness.29 navicular syndrome and does not prevent or retard progres-
The length of the treatment period varies, with some horses sion of the damaging processes. The various PDN meth-
showing clinical improvement for months after discontinu- ods share the common goal of atraumatically sectioning the ing therapy. One author noted that some horses that did not nerve to minimize the likelihood of the most common com-respond to an isoxsuprine dosage of 0.6 mg/kg PO q12h did plication: neuroma formation.40–45 Research suggests that the respond satisfactorily to 0.9 mg/kg PO q12h.34
simple guillotine technique results in the longest period
Pentoxifylline and propentofylline are other hemo- of desensitization and least chance of neuroma formation
rheologic agents that have been used for treating navicular compared with epineural capping and carbon dioxide laser syndrome. In one study on the efficacy of propentofylline division.40,43,44 The guillotine technique can be performed in
E6 Compendium: Continuing Education for Veterinarians® January 2011 Vetlearn.com

several different ways. Some clinicians make a 1- to 2-cm
incision over the nerves for each affected foot, just proxi-mal to the collateral cartilages, and remove approximately
1 cm of palmar digital nerve.41 Other clinicians make either
a 3- to 4-cm incision per nerve or two 1-cm incisions (one
just proximal to the collateral cartilage, and the other just
distal to the proximal sesamoid bones)34,42,45 (FIGURE 6). In
this method, approximately 3 to 4 cm of each palmar digital
nerve is removed.42,45
Postoperative care is extremely important in the success
of this procedure. Horses are confined to a stall and hand-walked for 1 month. Support bandages are maintained while
the horse is on stall rest. Some clinicians support postopera-tive perineural injection of the proximal transected nerve root with a corticosteroid to reduce postoperative inflam-mation. Limited exercise, bandaging, and an atraumatic sur-
gical procedure all have a significant effect on preventing
neuroma formation.
Clinical interpretation of the long-term resolution of lame-
ness after PDN varies, as do reported success rates. Published reports indicate that up to 92% of horses were in work 1 year after PDN.43 In the same study, 77% of horses in work 1 year after surgery were sound.43 In another study, 74% of horses
were sound 1 year after PDN; however, this percentage decreased to 63% after 2 years.41 Complications associated with PDN include failure to alleviate lameness due to remain-ing accessory branches of the palmar digital nerve, rupture of the DDFT, subluxation or luxation of the DIPJ, and deep
hoof infection; therefore, PDN should not be recommended casually. Recurrence of lameness is most commonly associ-ated with reinnervation or neuroma formation. Development of a painful neuroma may be managed with surgical excision or perineural injections of Sarapin (High Chemical Company, Levittown, PA) and triamcinolone acetate.
Alternative Surgical Options
Navicular bursoscopy is usually a diagnostic tool but may be
used for treatment, depending on the pathology noted on endoscopic examination.46,47
Desmotomy of the collateral (suspensory) ligaments of
the navicular bone has been recommended as a surgical treatment for navicular syndrome.48 In a study evaluating
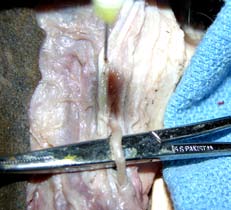
Palmar digital neurectomy using Black's technique,
in which the guillotine technique is used for the proximal and
118 horses, 76% of treated horses were sound 6 months after
distal incisions to remove 3 to 4 cm of the palmar digital nerve.
surgery, but only 43% remained sound after 3 years.49 In a study from New Zealand, 12 of 17 horses were sound at least 6 months after surgery.50
clinical trials have been performed to date, but anecdotal
Surgical drilling of cyst-like lesions involving the navicu- evidence suggests that this may be a treatment option in
lar bone via an arthroscopic approach has been described, horses with severe bone edema identified on MRI. but no follow-up data are available at this time.51
Desmotomy of the accessory ligament of the DDFT has
Some clinicians advocate core decompression of the been described as a treatment for navicular syndrome in
navicular bone in horses with navicular syndrome.52 No horses with a markedly upright foot conformation.53
Vetlearn.com January 2011 Compendium: Continuing Education for Veterinarians® E7
3. Wright IM, Kidd L, Thorp BH. Gross, histological and histomorphometric features
of the navicular bone and related structures in the horse. Equine Vet J 1998;30:220-
Key Facts
4. Pool RR, Meagher DM, Stover SM. Pathophysiology of navicular syndrome. Vet
Clin North Am Equine Pract 1989;5:109-129.
• Navicular syndrome is a chronic, progressive
5. Pleasant RS, Baker GJ, Foreman JH, et al. Intraosseous pressure and pathologic
condition affecting the navicular bone and bursa,
changes in horses with navicular disease. Am J Vet Res 1993;54:7-12.
deep digital flexor tendon, and associated soft tissue
6. Honnas C. Navicular syndrome: non-surgical management. Am Coll Vet Surg
structures composing the navicular apparatus.
7. Crisman M, Pleasant RS. Treating navicular disease. Vet Med 1997:454-459.
8. Trotter G. Therapy of navicular disease. Compend Contin Educ Pract Vet
• Because of the wide range of pathologic changes
associated with navicular syndrome and lack of a cure
9. Turner TA. Proper shoeing and shoeing principles for the management of navicular
for it, treatment is directed toward palliative care.
syndrome. Proc AAEP 1988:299-305.
10. Wil emen MA, Savelberg HH, Barneveld A. The effect of orthopaedic shoeing on
• Treatment of navicular syndrome should focus
the force exerted by the deep digital flexor tendon on the navicular bone in horses.
on managing clinical signs, alleviating stress on
Equine Vet J 1999;31:25-30.
11. Schoonover MJ, Jann HW, Blaik MA. Quantitative comparison of three common-
the navicular region, and preventing or retarding
ly used treatments for navicular syndrome in horses. Am J Vet Res 2005;66:1247-
degenerative changes in the navicular bursal region.
12. Ostblom LC, Lund C, Melsen F. Navicular bone disease: results of treatment using
egg-bar shoeing technique. Equine Vet J 1984;16:203-206.
13. Ostblom L, Lund C, Melsen F. Navicular bone disease: a comparative histomorpho-
These alternative surgical therapies need further research metric study. Equine Vet J 1989;21:431-433.
and clinical evaluation to determine their merit.
14. Verschooten F, Desmet P, Peremans K, et al. Navicular disease in the horse: the ef-
fect of controlled intrabursal corticoid injection. J Equine Vet Sci 1990;10:316.
15. Pauwels FE, Schumacher J, Castro FA, et al. Evaluation of the diffusion of cortico-
steroids between the distal interphalangeal joint and navicular bursa in horses. Am J
Temporary resolution of palmar foot pain can be achieved Vet Res 2008;69:611-616.
by chemical ablation of sensory fibers in the palmar digi- 16. Dabareiner RM, Carter GK, Honnas CM. Injection of corticosteroids, hyaluronate,
and amikacin into the navicular bursa in horses with signs of navicular area pain unre-
tal nerves. Some products (Sarapin [a plant alkaloid that is sponsive to other treatments: 25 cases (1999-2002). JAVMA 2003;223:1469-1474.
thought to alter transmission in type-C fibers] and cobra 17. Morisset S, Frisbie DD, Robbins PD, et al. IL-1ra/IGF-1 gene therapy modulates
repair of microfractured chondral defects. Clin Orthop Relat Res 2007;462:221-228.
venom35) can cause temporary loss of sensation and are usu- 18. Nixon AJ, Haupt JL, Frisbie DD, et al. Gene-mediated restoration of cartilage matrix
ally injected in combination with a corticosteroid. Liquid by combination insulin-like growth factor-I/interleukin-1 receptor antagonist therapy. nitrogen can be injected percutaneously to freeze the digital Gene Ther 2005;12:177-186.
19. Kato H, Ohashi T, Matsushiro H, et al. Molecular cloning and functional expression
of equine interleukin-1 receptor antagonist. Vet Immunol Immunopathol 1997;56:221-
The combination of nontraditional therapies (e.g., acu-
20. Howard RD, McIlwraith CW, Trotter GW, et al. Cloning of equine interleukin 1 re-
puncture) with traditional ones (e.g., rest, corrective shoe- ceptor antagonist and determination of its full-length cDNA sequence. Am J Vet Res
ing) may be beneficial.55
Several studies have evaluated the efficacy of extracor-
21. Frisbie DD, McIlwraith CW. Evaluation of gene therapy as a treatment for equine
traumatic arthritis and osteoarthritis. Clin Orthop Relat Res 2000:S273-S287.
poreal shock wave therapy for treating navicular syndrome, 22. Frisbie DD, Ghivizzani SC, Robbins PD, et al. Treatment of experimental equine
and the results have varied.56–58
osteoarthritis by in vivo delivery of the equine interleukin-1 receptor antagonist gene.
Gene Ther 2002;9:12-20.
23. Frisbie DD, Kawcak CE, Werpy NM, et al. Clinical, biochemical, and histologic ef-
fects of intra-articular administration of autologous conditioned serum in horses with
Currently, there is no standardized treatment for navicular experimentally induced osteoarthritis. Am J Vet Res 2007;68:290-296.
24. Doucet MY, Bertone AL, Hendrickson D, et al. Comparison of efficacy and safety of
syndrome. The response to various therapies indicates that paste formulations of firocoxib and phenylbutazone in horses with natural y occurring
affected horses most likely experience pain from several osteoarthritis. JAVMA 2008;232:91-97.
different sources, and many of the therapies improve the 25. Crisman M. Evaluation of polysulfated glycosaminoglycan for the treatment of
navicular disease: a double blind study. Proc AAEP 1995:219-220.
associated lameness to some degree. Treatment is often 26. Hanson RR, Hammad TA, Brawner WR. Evaluation of the clinical efficacy of a
directed at pain relief rather than preventing further damage. nutraceutical in the treatment of navicular syndrome: a double-blinded placebo-con-
trolled randomized clinical trial. Vet Surg 1997:416-417.
Focusing on maintaining a balanced hoof through proper 27. Carter GK, Dabareiner R. Therapeutic considerations for horses presenting lame-
trimming and shoeing in combination with improved diag- ness from palmar foot pain. Proc AAEP 2006:203-208.
nostic techniques during the period of soft tissue inflamma-
28. Du J, White N, Eddington ND. The bioavailability and pharmacokinetics of glu-
cosamine hydrochloride and chondroitin sulfate after oral and intravenous single dose
tion may help prevent this devastating condition.
administration in the horse. Biopharm Drug Dispos 2004;25:109-116.
29. Turner A, Tucker C. The evaluation of isoxsuprine hydrochloride for the treatment
of navicular disease: a double blind study. Equine Vet J 1989;21:338.
1. Widmer WR, Buckwalter KA, Fessler JF, et al. Use of radiography, computed to-
30. Ingle-Fehr JE, Baxter GM. The effect of oral isoxsuprine and pentoxifylline on digi-
mography and magnetic resonance imaging for evaluation of navicular syndrome in
tal and laminar blood flow in healthy horses. Vet Surg 1999;28:154-160.
the horse. Vet Radiol Ultrasound 2000;41:108-116.
31. Erkert RS, Macallister CG. Isoxsuprine hydrochloride in the horse: a review. J Vet
2. Dyson S, Murray R, Schramme M, et al. Magnetic resonance imaging of the equine
Pharmacol Ther 2002;25:81-87.
foot: 15 horses. Equine Vet J 2003;35:18-26.
32. Belloli C, Carcano R, Arioli F, et al. Affinity of isoxsuprine hydrochloride for the
E8 Compendium: Continuing Education for Veterinarians® January 2011 Vetlearn.com
treatment of navicular disease: a double blind study. Equine Vet J 2000;32:119.
33. Deumer J, de Haan F, Tulp M, et al. Effect of isoxsuprine-resin preparation on blood
46. Cruz AM, Pharr JW, Bailey JV, et al. Podotrochlear bursa endoscopy in the horse:
flow in the equine thoracic limb. Vet Rec 1991;129:427.
a cadaver study. Vet Surg 2001;30:539-545.
34. Madison JB, Dyson SJ. Treatment and prognosis of horses with navicular disease.
47. Smith MR, Wright IM, Smith RK. Endoscopic assessment and treatment of lesions
In: Ross MW, Dyson SJ, eds. Diagnosis and Management of Lameness in the Horse. of the deep digital flexor tendon in the navicular bursae of 20 lame horses. Equine Vet
St. Louis: Saunders; 2003:299-304.
35. Kirker-Head K. Use of propentofylline for the treatment of equine navicular disease.
48. Wright I. Navicular suspensory desmotomy in the treatment of navicular disease:
Proc Eur Coll Vet Surg 1993;2:10.
technique and preliminary results. Equine Vet J 1986;18:1986.
36. Liska DA, Akucewich LH, Marsella R, et al. Pharmacokinetics of pentoxifylline and
49. Wright IM. A study of 118 cases of navicular disease: treatment by navicular sus-
its 5-hydroxyhexyl metabolite after oral and intravenous administration of pentoxifyl-
pensory desmotomy. Equine Vet J 1993;25:501-509.
line to healthy adult horses. Am J Vet Res 2006;67:1621-1627.
50. Bell B, Bridge I, Sullivan S. Surgical treatment of navicular syndrome in the horse
37. Delguste C, Amory H, Doucet M, et al. Pharmacological effects of tiludronate in
using navicular suspensory desmotomy. N Z Vet J 1996;44:26.
horses after long-term immobilization. Bone 2007;41:414-421.
51. Zierz J, Schad D, Heeb D, et al. Chirurgische moglichkeitenzurversorgung von
38. Denoix JM, Thibaud D, Riccio B. Tiludronate as a new therapeutic agent in the
strahlbeinzysten sowie strukturdefekten im strahlbein. Pferdheilkunde 2000;16:171.
treatment of navicular disease: a double-blind placebo-controlled clinical trial. Equine
52. Schramme MC. Recent advances in the treatment of palmar foot pain. Auburn Uni-
Vet J 2003;35:407-413.
versity Equine Fall Conference 2008.
39. Delguste C, Amory H, Guyonnet J, et al. Comparison pharmacokinetics of two in-
53. Turner T. Inferior check desmotomy as a treatment for navicular disease. Proc Int
travenous administration regimens of tiludronate in healthy adult horses and effects
Symp Podotrochlosis 1993.
on the bone resorption marker CTX-1. J Vet Pharmacol Ther 2008;31:108-116.
54. Tate LP. Cryoneurectomy in the horse. JAVMA 1980;177:423.
40. Dabareiner RM, White NA, Sullins KE. Comparison of current techniques for pal-
55. Schoen AM. Navicular disease. In: Schoen AM, ed. Veterinary Acupuncture: An-
mar digital neurectomy in horses. Proc AAEP 1997:231-232.
cient Art to Modern Medicine. Goleta, CA: American Veterinary Publications; 1994:520-
41. Jackman BR, Baxter GM, Doran RE, et al. Palmar digital neurectomy in horses. 57
cases (1984-1990). Vet Surg 1993;23:285-288.
56. McClure S, Evans RB, Miles KG, et al. Extracorporeal shock wave therapy for treat-
42. Maher O, Davis DM, Drake C, et al. Pul -through techniques for palmar digital
ment of navicular syndrome. Proc AAEP 2004:316-319.
neurectomy: forty-one horses (1998-2004). Vet Surg 2008;37:87-93.
57. Brown KE, Nickels FA, Caron JP, et al. Investigation of the immediate analgesic
43. Matthews S, Dart AJ, Dowling BA. Palmar digital neurectomy in 24 horses using
effects of extracorporeal shock wave therapy for treatment of navicular disease in
the guillotine technique. Aust Vet J 2003;81:402-405.
horses. Vet Surg 2005;34:554-558.
44. Evans LH. Procedures used to prevent painful neuromas. Proc AAEP 1970:103.
58. Blum N, Kreling K, Litzke LF. The use of extracorporeal shock wave therapy in
45. Black JB. Palmar digital neurectomy: an alternative surgical approach. Proc AAEP
horses with navicular disease. Pferdheilkunde 2005;21:29-38.
Vetlearn.com January 2011 Compendium: Continuing Education for Veterinarians® E9
CE TEST This article qualifies for 3 contact hours of continuing education credit from the Auburn University College of Veterinary
Medicine. Subscribers must take individual CE tests online and get real-time scores at Vetlearn.com. Those who wish to apply this credit
to fulfil state relicensure requirements should consult their respective state authorities regarding the applicability of this program.
1. Which change(s) has/have been associ-
b. In one study, 80% of horses that no
a. isoxsuprine hydrochloride
ated with the navicular bone and sur-
longer responded to traditional therapy
rounding soft tissue structures in horses
for navicular syndrome were sound 2
with navicular syndrome?
weeks after intrabursal injections of
a. erosions and fibril ation of the
corticosteroids, sodium hyaluronate,
and amikacin.
8. Regarding PDN, which surgical
b. remodeling of the underlying subchon-
c. Administration of glucosamine–
technique(s) best minimizes the poten-
dral and trabecular bone
chondroitin sulfate compounds and
tial for neuroma formation?
c. palmar cortical bone erosion
intramuscular PSGAGs is reported to
a. the guillotine technique
d. all of the above
alter the clinical signs associated with
b. epineural capping
navicular syndrome.
c. carbon dioxide laser division
2. Which medical treatment(s) is/are used
in horses with navicular syndrome?
a. systemic anti nflammatories
5. Which medication(s) can be injected
9. Which potential complication(s) is/are
b. corrective shoeing
into the DIPJ or navicular bursa to con-
associated with PDN?
c. systemic hemorheologic medications
trol clinical signs in horses with navicu-
a. failure to al eviate lameness due to
d. all of the above
remaining accessory branches of the
palmar digital nerve
3. The goal of shoeing a horse with navicu-
b. rupture of the DDFT
lar syndrome is to reduce forces on the
c. sodium hyaluronate
c. fracture of the third phalanx
navicular region by
a. establishing the correct hoof balance
and hoof–pastern axis.
6. Which medication(s) can be adminis-
10. Which product(s) can be used in chemi-
b. permitting an easier breakover of the
tered to minimize pain and inflammation
cal ablation of sensory fibers in the
associated with navicular syndrome?
palmar digital nerves?
c. moving the weightbearing surface of
a. Sarapin
the hoof forward away from the heel.
b. flunixin meglumine
b. liquid nitrogen
c. carprofen
c. cobra venom
d. all of the above
d. all of the above
4. Which statement(s) regarding treatment
of navicular syndrome is/are true?
7. Which medication(s) has/have been
a. Injecting steroids into the DIPJ does
shown to decrease the clinical signs
not treat the navicular region of the
associated with navicular syndrome
(clinically or in studies)?
E10 Compendium: Continuing Education for Veterinarians® January 2011 Vetlearn.com
Copyright 2011 MediMedia Animal Health. This document is for internal purposes only. Reprinting or posting on an external website without written permission from MMAH is a violation of copyright laws.
Source: http://assets.prod.vetlearn.com.s3.amazonaws.com/14/d3c47053df11e0a4050050568d17ce/file/PV0111_waguespack_Surgical.pdf
Medicine County Herbs Herbal medicine from Madison County, North Carolina Herbal Tincture Formulas L X : milky oat seed, passionflower, wood betony. calms the mind & relaxes the body. great for sleep, anxiety, nervous agitation. M R: st. john's wort, lemon balm, rose. "In the depth of winter I found there was, within me, an invincible summer." –Albert Camus. for sadness, depression, the blues. elevates mood, restores confidence.
Fighting Image Spam The Issue Spammers are developing more and more sophisticated methods to avoid filters. Generally, this entails attempts at sending out e-mail "waves" in which each and every e-mail is in some way unique and different from its predecessors. The relative success of each wave is then analyzed by the