Guide_inpatient_text_eng.pmd
treatment of
1Dr Sultana Khanum, former Regional Adviser, Nutrition for Health and Development, WHO South-East Asia Regional OfficeProfessor Ann Ashworth & Ms Claire Schofield, London School of Hygiene and Tropical MedicineProfessor Alan Jackson, University of Southampton
Guidelines for the inpatient treatment of severely malnourished children

WHO Library Cataloguing-in-Publication Data
Ashworth, Ann.
Guidelines for the inpatient treatment of severely malnourished children /Ann Ashworth … [et al.]
1. Child nutrition disorders – therapy 2. Starvation – therapy 3. GuidelinesI.Title 4. Manuals
ISBN 92 4 154609 3
(NLM classification: WS 115)
World Health Organization 2003
All rights reserved. Publications of the World Health Organization can be
obtained from Marketing and Dissemination, World Health Organization, 20
Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41
22 791 4857; email: [email protected]). Requests for permission to
reproduce or translate WHO publications – whether for sale or for
noncommercial distribution – should be addressed to Publications, at the
above address (fax: +41 22 791 4806; email: [email protected]).
The designations employed and the presentation of the material in this
publication do not imply the expression of any opinion whatsoever on the
part of the World Health Organization concerning the legal status of any
country, territory, city or area or of its authorities, or concerning the
delimitation of its frontiers or boundaries. Dotted lines on maps represent
approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers' productsdoes not imply that they are endorsed or recommended by the World HealthOrganization in preference to others of a similar nature that are notmentioned. Errors and omissions excepted, the names of proprietaryproducts are distinguished by initial capital letters.
The World Health Organization does not warrant that the informationcontained in this publication is complete and correct and shall not be liablefor any damages incurred as a result of its use.
Guidelines for the inpatient treatment of severely malnourished children
Preface
Acknowledgements
Introduction
A. General principles for routine care (the ‘10 Steps')
Step 1. Treat/prevent hypoglycaemia
Step 2. Treat/prevent hypothermia
Step 3. Treat/prevent dehydration
Step 4. Correct electrolyte imbalance
Step 5. Treat/prevent infection
Step 6. Correct micronutrient deficiencies
Step 7. Start cautious feeding
Step 8. Achieve catch-up growth
Step 9. Provide sensory stimulation and emotional support
Step 10. Prepare for follow-up after recovery
B. Emergency treatment of shock and severe anaemia
1. Shock in severely malnourished children
2. Severe anaemia in malnourished children
C. Treatment of associated conditions
1. Vitamin A deficiency
3. Parasitic worms
4. Continuing diarrhoea
5. Tuberculosis (TB)
D. Failure to respond to treatment
1. High mortality
2. Low weight gain during the rehabilitation phase
E. Discharge before recovery is complete
Appendix 1. Weight-for-height reference table
Appendix 2. Monitoring records
Appendix 3. Recipes for ReSoMal & electrolyte/mineral solution 33Appendix 4. Antibiotics reference table
Appendix 5. Recipes for starter and catch-up formulas
Appendix 6. Volume of F-75 to give for children of different
Appendix 7. Volume of F-75 for children with severe (+++)
Appendix 8. Range of volumes for free feeding with F-100
Appendix 9. Weight record chart
Appendix 10. Structured play activities
Appendix 11. Discharge card
Guidelines for the inpatient treatment of severely malnourished children
Guidelines for the inpatient treatment of severely malnourished children
Poor nutrition severely hinders personal, social and national development.
The problem is more obvious among the poor and disadvantaged. Theultimate consequence is millions of severely malnourished children throughoutthe world. In developing countries an estimated 50.6 million children underthe age of five are malnourished, and those who are severely malnourishedand admitted to hospital face a 30-50% case fatality rate. With appropriatetreatment, as described in these guidelines, this unacceptably high deathrate can be reduced to less than 5%. The evidence base for effectiveprevention and treatment is incontrovertible, but it is not put into practice.
Data from 67 studies worldwide show that the median case fatality ratehas not changed for the past five decades, and that one in four severelymalnourished children died during treatment in the 1990s. In any decade,however, some centres obtained good results with fewer than 5% dying,whereas others fared poorly with a mortality rate of approximately 50%.
This disparity is not due to differences in the prevalence of severe cases ofmalnutrition, but it is rather the result of poor treatment practices. Where mortalityis low a set of basic principles has been followed. High case fatality ratesand poor rates of weight gain result from a failure to appreciate that treatmenthas to be carried out in stages and that the order in which problems areaddressed is fundamental to effective care:
• firstly, severe malnutrition represents a medical emergency with an
urgent need to correct hypothermia, hypoglycaemia and silent infection;
• secondly, there is an impairment of the cellular machinery. Tissue
function cannot be restored unless the machinery is repaired, whichincludes remedying multiple specific deficiencies. These may not bevisible, and often are the consequence of multiple silent infections;
• thirdly, tissue deficits and abnormal body composition are obvious,
but cannot be safely corrected until the cellular machinery has beenadequately repaired. Rehydration with intravenous fluids can increasemortality, as can manipulation of abnormal blood chemistry.
Aggressive attempts to promote rapid weight gain from the start oftreatment is also dangerous. Many prescribe a high protein diet forchildren with kwashiorkor, but this can be fatal. Many prescribediuretics to get rid of oedema. This procedure can be fatal. Prescribingiron to treat anaemia increases deaths in the initial phase of treatment.
Guidelines for the inpatient treatment of severely malnourished children
Substantial reductions in mortality rates have been achieved by modifyingtreatment to take account of the physiological and metabolic changesoccurring in severe malnutrition. In the International Centre for DiarrhoealDisease Research, Bangladesh, after the introduction of a standardizedprotocol, based on the WHO guidelines, fatality rate decreased to 9% andsubsequently to 3.9% from an earlier 17%. In South Africa, the mortality ratedecreased from 30-40% to less than 15%. Emergency relief organizationssuccessfully use the guidelines to treat severe malnutrition in tents.Thetreatment guidelines described here are therefore applicable not only inhospitals but also in therapeutic feeding centres in emergency situations,and in nutrition rehabilitation centres after initial treatment in hospital.
Sultana Khanum
Department of Nutrition for Health and Development World Health
Organization
Guidelines for the inpatient treatment of severely malnourished children
The authors gratefully acknowledge the contributions and suggestions of DrGraeme Clugston, Dr Djamil Benbouzid, and Dr Olivier Fontaine (WHOGeneva), and Professor Michael Golden (University of Aberdeen).
Thanks are due to Professor Sally Grantham-McGregor (Institute of ChildHealth) for the play activities, and to Professor John Waterlow, ProfessorJoe Millward, Dr Harry Campbell, Ann Burgess and Patricia Whitesell fortheir advice and encouragement.
In addition, WHO wishes to thank the Canadian International DevelopmentAgency (CIDA) and the Department for International Development (DFID),U.K., for providing financial support for the production of this document.
Guidelines for the inpatient treatment of severely malnourished children
Guidelines for the inpatient treatment of severely malnourished children
Every year some 10.6 million children die before they reach their fifthbirthday. Seven out of every 10 of these deaths are due to diarrhoea,pneumonia, measles, malaria or malnutrition. The WHO manualManagement of Severe Malnutrition: a manual for physicians and othersenior health workers and the following companion guidelines have beendeveloped to improve inpatient treatment of severe malnutrition. The WHO/UNICEF strategy of Integrated Management of Childhood Illness (IMCI)also aims to reduce these deaths by improving treatment.
Special guidelines are needed because of the profound physiological andmetabolic changes that take place when children become malnourished.
These changes affect every cell, organ and system. The process of changeis called reductive adaptation. Malnourished children do not respond to medicaltreatment in the same way as if they were well nourished. Malnourishedchildren are much more likely to die, with or without complications, than theirwell nourished counterparts. With appropriate case management in hospitaland follow-up care, the lives of many children can be saved.
The following guidelines set out simple, specific instructions for thetreatment of severely malnourished children. The aim is to provide practicalhelp for those responsible for the medical and dietary management of suchchildren. Lack of appropriate care leads to diarrhoea, poor appetite, slowrecovery and high mortality. These problems can be overcome if certainbasic principles are followed.
Severe malnutrition is defined in these guidelines as the presence of
severe wasting (<70% weight-for-height or <-3SD) and/or oedema.
(Appendix 1 provides a weight-for-height reference table.)
The guidelines are divided in five sections:
General principles for routine care (the'10 steps')
Emergency treatment of shock and severe anaemia
Treatment of associated conditions
Failure to respond to treatment
Discharge before recovery is complete
Guidelines for the inpatient treatment of severely malnourished children
A. GENERAL PRINCIPLES FOR ROUTINE CARE
(the ‘10 Steps')2
There are ten essential steps:
1.Treat/prevent hypoglycaemia 2.Treat/prevent hypothermia 3.Treat/prevent dehydration 4.Correct electrolyte imbalance 5.Treat/prevent infection 6.Correct micronutrient deficiencies 7.Start cautious feeding 8.Achieve catch-up growth 9.Provide sensory stimulation and emotional support10. Prepare for follow-up after recovery
These steps are accomplished in two phases: an initial stabilisation phase
where the acute medical conditions are managed; and a longer rehabilitation
phase. Note that treatment procedures are similar for marasmus and
kwashiorkor. The approximate time-scale is given in the box below:
Weeks 2-6
1. Hypoglycaemia2. Hypothermia3. Dehydration4. Electrolytes5. Infection6. Micronutrients
7. Cautious feeding8. Catch-up growth9. Sensory stimulation10. Prepare for follow-up
2 Ashworth A, Jackson A, Khanum S, Schofield C. Ten steps to recovery: Child health dialogue,issue 3 and 4, 1996
Guidelines for the inpatient treatment of severely malnourished children
Step 1. Treat/prevent hypoglycaemia
Hypoglycaemia and hypothermia usually occur together and are signs ofinfection. Check for hypoglycaemia whenever hypothermia(axillary<35.0oC; rectal<35.5oC) is found. Frequent feeding is important inpreventing both conditions.
Treatment:
If the child is conscious and dextrostix shows <3mmol/l or 54mg/dl give:
• 50 ml bolus of 10% glucose or 10% sucrose solution (1 rounded
teaspoon of sugar in 3.5 tablespoons water), orally or by nasogastric(NG) tube. Then feed starter F-75 (see step 7) every 30 min. for twohours (giving one quarter of the two-hourly feed each time)
• antibiotics (see step 5)• two-hourly feeds, day and night (see step 7)
If the child is unconscious, lethargic or convulsing give:
• IV sterile 10% glucose (5ml/kg), followed by 50ml of 10% glucose
or sucrose by Ng tube. Then give starter F-75 as above
• antibiotics• two-hourly feeds, day and night
• blood glucose: if this was low, repeat dextrostix taking blood from
finger or heel, after two hours. Once treated, most children stabilisewithin 30 min. If blood glucose falls to <3 mmol/l give a further 50mlbolus of 10% glucose or sucrose solution, and continue feeding every30 min. until stable
• rectal temperature: if this falls to <35.5oC, repeat dextrostix• level of consciousness: if this deteriorates, repeat dextrostix
• feed two-hourly, start straightaway (see step 7) or if necessary,
• always give feeds throughout the night
Note: If you are unable to test the blood glucose level, assume all severely
malnourished children are hypoglycaemic and treat accordingly.
Guidelines for the inpatient treatment of severely malnourished children
Step 2. Treat/prevent hypothermia
Treatment:
If the axillary temperature is <35.0oC, take the rectal temperature using a low
reading thermometer.
If the rectal temperature is <35.5oC (<95.9oF):
• feed straightaway (or start rehydration if needed)• rewarm the child: either clothe the child (including head), cover with a
warmed blanket and place a heater or lamp nearby (do not use ahot water bottle), or put the child on the mother's bare chest (skin toskin) and cover them
• give antibiotics (see step 5)
• body temperature: during rewarming take rectal temperature two-hourly until it rises to >36.5oC (take half-hourly if heater is used)• ensure the child is covered at all times, especially at night• feel for warmth• blood glucose level: check for hypoglycaemia whenever hypothermia is found
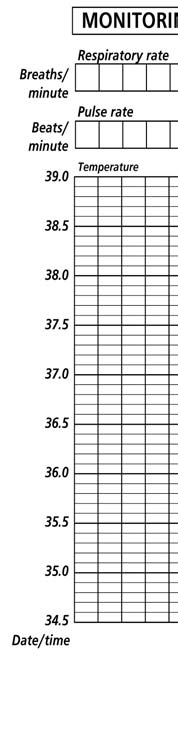
(Appendix 2 provides an example of a chart for recording temperature, pulseand respiratory rates).
• feed two-hourly, start straightaway (see step 7)• always give feeds throughout the day and night• keep covered and away from draughts• keep the child dry, change wet nappies, clothes and bedding• avoid exposure (e.g. bathing, prolonged medical examinations)• let child sleep with mother/carer at night for warmth
Note: If a low reading thermometer is unavailable and the child's temperature
is too low to register on an ordinary thermometer, assume the child has
hypothermia.
Guidelines for the inpatient treatment of severely malnourished children
Step 3. Treat/prevent dehydration
Note: Low blood volume can coexist with oedema. Do not use the IV
route for rehydration except in cases of shock and then do so with care,
infusing slowly to avoid flooding the circulation and overloading the heart
(see Section B: Emergency treatment).
Treatment:
The standard oral rehydration salts solution (90 mmol sodium/l) contains
too much sodium and too little potassium for severely malnourished children.
Instead give special Rehydration Solution for Malnutrition (ReSoMal). (For
recipe see Appendix 3).
It is difficult to estimate dehydration status in a severely malnourished childusing clinical signs alone. So assume all children with watery diarrhoeamay have dehydration and give:
• ReSoMal 5 ml/kg every 30 min. for two hours, orally or by nasogastric
• 5-10 ml/kg/h for next 4-10 hours: the exact amount to be given should
be determined by how much the child wants, and stool loss andvomiting. Replace the ReSoMal doses at 4, 6, 8 and 10 hours withF-75 if rehydration is continuing at these times, then
• continue feeding starter F-75 (see step 7)
During treatment, rapid respiration and pulse rates should slow down andthe child should begin to pass urine.
Monitor progress of rehydration:Observe half-hourly for two hours, then hourly for the next 6-12 hours,recording:
• pulse rate• respiratory rate• urine frequency• stool/vomit frequency
Return of tears, moist mouth, eyes and fontanelle appearing less sunken,and improved skin turgor, are also signs that rehydration is proceeding. It
Guidelines for the inpatient treatment of severely malnourished children
should be noted that many severely malnourished children will not showthese changes even when fully rehydrated.
Continuing rapid breathing and pulse during rehydration suggest coexistinginfection or overhydration. Signs of excess fluid (overhydration) areincreasing respiratory rate and pulse rate, increasing oedema and puffyeyelids. If these signs occur, stop fluids immediately and reassess afterone hour.
Prevention:
To prevent dehydration when a child has continuing watery diarrhoea:
• keep feeding with starter F-75 (see step 7)• replace approximate volume of stool losses with ReSoMal. As a
guide give 50-100 ml after each watery stool. (Note: it is common formalnourished children to pass many small unformed stools: theseshould not be confused with profuse watery stools and do not requirefluid replacement)
• if the child is breastfed, encourage to continue
Step 4. Correct electrolyte imbalance
All severely malnourished children have excess body sodium even thoughplasma sodium may be low (giving high sodium loads will kill). Deficienciesof potassium and magnesium are also present and may take at least twoweeks to correct. Oedema is partly due to these imbalances. Do NOT treatoedema with a diuretic.
Give:
• extra potassium 3-4 mmol/kg/d• extra magnesium 0.4-0.6 mmol/kg/d• when rehydrating, give low sodium rehydration fluid (e.g. ReSoMal)• prepare food without salt
The extra potassium and magnesium can be prepared in a liquid form andadded directly to feeds during preparation. Appendix 3 provides a recipe fora combined electrolyte/mineral solution. Adding 20 ml of this solution to 1 litreof feed will supply the extra potassium and magnesium required. The solutioncan also be added to ReSoMal.
Guidelines for the inpatient treatment of severely malnourished children
Step 5. Treat/prevent infection
In severe malnutrition the usual signs of infection, such as fever, are often
absent, and infections are often hidden.
Therefore give routinely on admission:
• broad-spectrum antibiotic(s) AND
• measles vaccine if child is > 6m and not immunised
(delay if the child is in shock)
Note: Some experts routinely give, in addition to broad-spectrum
antibiotics, metronidazole (7.5 mg/kg 8-hourly for 7 days) to hasten repair
of the intestinal mucosa and reduce the risk of oxidative damage and
systemic infection arising from the overgrowth of anaerobic bacteria in
the small intestine.
Choice of broad-spectrum antibiotics: (see Appendix 4 for antibiotic
dosage):
a) if the child appears to have no complications give:
• Co-trimoxazole 5 ml paediatric suspension orally twice daily for 5
days (2.5 ml if weight <6 kg). (5 ml is equivalent to 40 mg TMP+200mg SMX).
OR
b) if the child is severely ill (apathetic, lethargic) or has complications
(hypoglycaemia; hypothermia; broken skin; respiratory tract or urinarytract infection) give:
• Ampicillin 50 mg/kg IM/IV 6-hourly for 2 days, then oral amoxycillin 15
mg/kg 8-hourly for 5 days, or if amoxycillin is not available, continuewith ampicillin but give orally 50 mg/kg 6-hourly
AND• Gentamicin 7.5 mg/kg IM/IV once daily for 7 days
If the child fails to improve clinically within 48 hours, ADD:
• Chloramphenicol 25 mg/kg IM/IV 8-hourly for 5 days
Where specific infections are identified, ADD:
• specific antibiotics if appropriate
• antimalarial treatment if the child has a positive blood film for malaria
Guidelines for the inpatient treatment of severely malnourished children
If anorexia persists after 5 days of antibiotic treatment, complete a full 10-
day course. If anorexia still persists, reassess the child fully, checking for
sites of infection and potentially resistant organisms, and ensure that vitamin
and mineral supplements have been correctly given.
Step 6. Correct micronutrient deficiencies
All severely malnourished children have vitamin and mineral deficiencies.
Although anaemia is common, do NOT give iron initially but wait until the
child has a good appetite and starts gaining weight (usually by the second
week), as giving iron can make infections worse.
Give:• Vitamin A orally on Day 1 (for age >12 months, give 200,000 IU; for
age 6-12 months, give 100,000 IU; for age 0-5 months, give 50,000IU) unless there is definite evidence that a dose has been given inthe last month
Give daily for at least 2 weeks:• Multivitamin supplement• Folic acid 1 mg/d (give 5 mg on Day 1)• Zinc 2 mg/kg/d• Copper 0.3 mg/kg/d• Iron 3 mg/kg/d but only when gaining weight
Appendix 3 provides a recipe for a combined electrolyte/mineral solution.
Adding 20 ml of this solution to 1 litre of feed will supply the zinc and copperneeded, as well as potassium and magnesium. This solution can also beadded to ReSoMal.
Note: A combined electrolyte/mineral/vitamin mix for severe malnutrition is
available commercially. This can replace the electrolyte/mineral solution
and multivitamin and folic acid supplements mentioned in steps 4 and 6,
but still give the large single dose of vitamin A and folic acid on Day 1, and
iron daily after weight gain has started.
Guidelines for the inpatient treatment of severely malnourished children
Step 7. Start cautious feeding
In the stabilisation phase a cautious approach is required because of
the child's fragile physiological state and reduced homeostatic capacity.
Feeding should be started as soon as possible after admission and should
be designed to provide just sufficient energy and protein to maintain basic
physiological processes. The essential features of feeding in the stabilisation
phase are:
• small, frequent feeds of low osmolarity and low lactose• oral or nasogastric (NG) feeds (never parenteral preparations)• 100 kcal/kg/d• 1-1.5 g protein/kg/d• 130 ml/kg/d of fluid (100 ml/kg/d if the child has severe oedema)• if the child is breastfed, encourage to continue breastfeeding but
give the prescribed amounts of starter formula to make sure thechild's needs are met.
The suggested starter formula and feeding schedules (see below) aredesigned to meet these targets.
Milk-based formulas such as starter F-75 containing 75 kcal/100 ml and 0.9g protein/100 ml will be satisfactory for most children (see Appendix 5 forrecipes). Give from a cup. Very weak children may be fed by spoon, dropperor syringe.
A recommended schedule in which volume is gradually increased, and feedingfrequency gradually decreased is:
For children with a good appetite and no oedema, this schedule can becompleted in 2-3 days (e.g. 24 hours at each level). Appendix 6 shows thevolume/feed already calculated according to body weight. Appendix 7 givesthe feed volumes for children with severe oedema. Use the Day 1 weightto calculate how much to give, even if the child loses or gains weight inthis phase.
Guidelines for the inpatient treatment of severely malnourished children
If, after allowing for any vomiting, intake does not reach 80 kcal/kg/d (105ml starter formula/kg) despite frequent feeds, coaxing and re-offering, givethe remaining feed by NG tube (see Appendices 6 and 7 (Column 6) forintake volumes below which NG feeding should be given). Do not exceed100 kcal/kg/d in this phase.
Monitor and note:
• amounts offered and left over• vomiting• frequency of watery stool• daily body weight
During the stabilisation phase, diarrhoea should gradually diminish andoedematous children should lose weight. If diarrhoea continues uncheckeddespite cautious refeeding, or worsens substantially, see section C4(continuing diarrhoea).
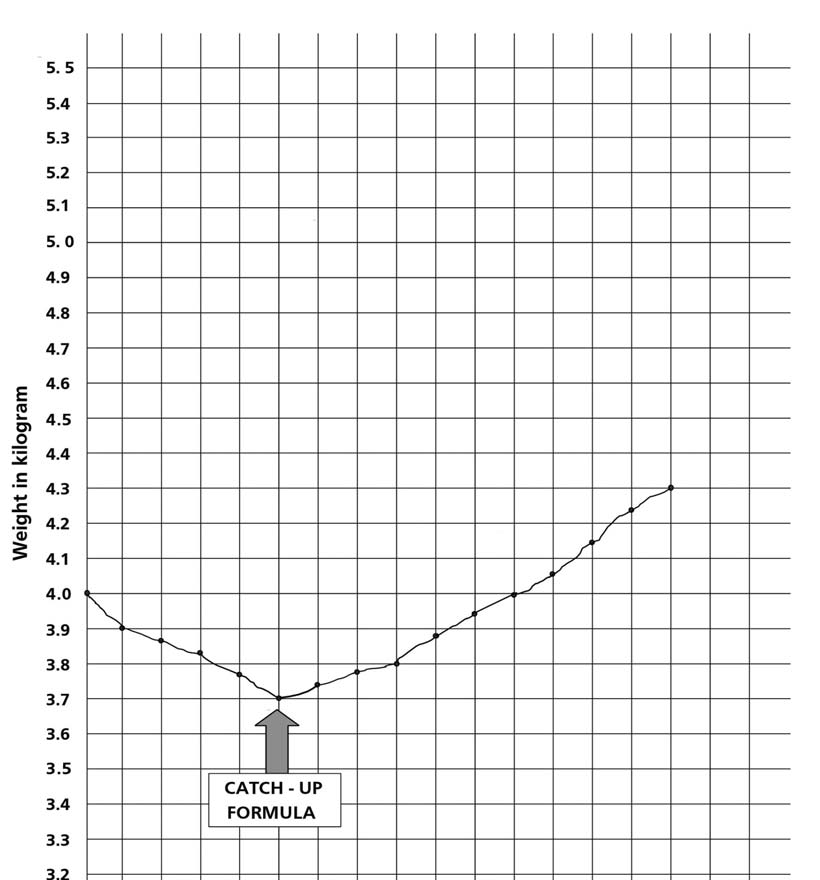
Step 8. Achieve catch-up growth
In the rehabilitation phase a vigorous approach to feeding is required toachieve very high intakes and rapid weight gain of >10 g gain/kg/d. Therecommended milk-based F-100 contains 100 kcal and 2.9 g protein/100 ml(see Appendix 5 for recipes). Modified porridges or modified family foodscan be used provided they have comparable energy and proteinconcentrations.
Readiness to enter the rehabilitation phase is signalled by a return of appetite,usually about one week after admission. A gradual transition is recommendedto avoid the risk of heart failure which can occur if children suddenly consumehuge amounts.
To change from starter to catch-up formula:
• replace starter F-75 with the same amount of catch-up formula F-
100 for 48 hours then,
• increase each successive feed by 10 ml until some feed remains
uneaten. The point when some remains unconsumed is likely tooccur when intakes reach about 30 ml/kg/feed (200 ml/kg/d).
Guidelines for the inpatient treatment of severely malnourished children
Monitor during the transition for signs of heart failure:
• respiratory rate• pulse rate
If respirations increase by 5 or more breaths/min and pulse by 25 or morebeats/min for two successive 4-hourly readings, reduce the volume perfeed (give 4-hourly F-100 at 16 ml/kg/feed for 24 hours, then 19 ml/kg/feedfor 24 hours, then 22 ml/kg/feed for 48 hours, then increase each feed by10 ml as above).
After the transition give:
• frequent feeds (at least 4-hourly) of unlimited amounts of a catch-
• 150-220 kcal/kg/d• 4-6 g protein/kg/d• if the child is breastfed, encourage to continue (Note: breast milk does
not have sufficient energy and protein to support rapid catch-upgrowth).
See Appendix 8 for range of volumes for free feeding with F-100.
Monitor progress after the transition by assessing the rate of weight
gain:
• weigh child each morning before feeding. Plot weight (Appendix 9
provides example)
• each week calculate and record weight gain as g/kg/d3
If weight gain is:
• poor (<5 g/kg/d), child requires full reassessment (see Section D)• moderate (5-10 g/kg/d), check whether intake targets are being met,
or if infection has been overlooked
• good (>10 g/kg/d), continue to praise staff and mothers
3 Calculating weight gain :
The example is for weight gain over 7 days, but the same procedure can be applied to any interval:
* substract from today's weight (in g) the child's weight 7 days earlier ;
* divide by 7 to determine the average daily weight gain (g/day) ;
* divide by the child's average weight in kg to calculate the weight gain as g/kg/day.
Guidelines for the inpatient treatment of severely malnourished children
Step 9. Provide sensory stimulation and emotional
support
In severe malnutrition there is delayed mental and behavioural development.
• tender loving care• a cheerful, stimulating environment• structured play therapy 15-30 min/d (Appendix 10 provides examples)• physical activity as soon as the child is well enough• maternal involvement when possible (e.g. comforting, feeding, bathing,
Step 10. Prepare for follow-up after recovery
A child who is 90% weight-for-length (equivalent to -1SD) can be consideredto have recovered. The child is still likely to have a low weight-for-age becauseof stunting. Good feeding practices and sensory stimulation should becontinued at home. Show parent or carer how to:
• feed frequently with energy- and nutrient-dense foods• give structured play therapy
Advise parent or carer to:
• bring child back for regular follow-up checks• ensure booster immunizations are given• ensure vitamin A is given every six months
Appendix 11 provides an example of a Discharge Card.
Guidelines for the inpatient treatment of severely malnourished children
B. EMERGENCY TREATMENT OF SHOCK AND
SEVERE ANAEMIA
1. Shock in severely malnourished children
Shock from dehydration and sepsis are likely to coexist in severelymalnourished children. They are difficult to differentiate on clinical signs alone.
Children with dehydration will respond to IV fluids. Those with septic shockand no dehydration will not respond. The amount of fluid given is determinedby the child's response. Overhydration must be avoided.
To start treatment:
• give oxygen• give sterile 10% glucose (5 ml/kg) by IV• give IV fluid at 15 ml/kg over 1 hour. Use Ringer's lactate with 5%
dextrose; or half-normal saline with 5% dextrose; or half-strengthDarrow's solution with 5% dextrose; or if these are unavailable,Ringer's lactate
• measure and record pulse and respiration rates every 10 minutes• give antibiotics (see step 5)
If there are signs of improvement (pulse and respiration rates fall):
• repeat IV 15 ml/kg over 1 hour; then• switch to oral or nasogastric rehydration with ReSoMal, 10 ml/kg/h
for up to 10 hours. (Leave IV in place in case required again); GiveReSoMal in alternate hours with starter F-75, then
• continue feeding with starter F-75
If the child fails to improve after the first hour of treatment (15 ml/kg),
assume that the child has septic shock. In this case:
• give maintenance IV fluids (4 ml/kg/h) while waiting for blood,• when blood is available transfuse fresh whole blood at 10 ml/kg
slowly over 3 hours; then
• begin feeding with starter F-75 (step 7)
Guidelines for the inpatient treatment of severely malnourished children
If the child gets worse during treatment (breathing increases by 5 breaths
or more/min and pulse increases by 25 or more beats/min):
• stop the infusion to prevent the child's condition worsening
2. Severe anaemia in malnourished children
A blood transfusion is required if:
• Hb is less than 4 g/dl• or if there is respiratory distress and Hb is between 4 and 6 g/dl
• whole blood 10 ml/kg body weight slowly over 3 hours• furosemide 1 mg/kg IV at the start of the transfusion
It is particularly important that the volume of 10 ml/kg is not exceeded inseverely malnourished children. If the severely anaemic child has signs ofcardiac failure, transfuse packed cells (5-7 ml/kg) rather than whole blood.
Monitor for signs of transfusion reactions. If any of the following signs developduring the transfusion, stop the transfusion:
• fever• itchy rash• dark red urine• confusion• shock
Also monitor the respiratory rate and pulse rate every 15 minutes. If either of
them rises, transfuse more slowly. Following the transfusion, if the Hb remains
less than 4 g/dl or between 4 and 6 g/dl in a child with continuing respiratory
distress, DO NOT repeat the transfusion within 4 days. In mild or moderate
anaemia, oral iron should be given for two months to replenish iron stores
BUT this should not be started until the child has begun to gain weight.
Guidelines for the inpatient treatment of severely malnourished children
C. TREATMENT OF ASSOCIATED CONDITIONS
Treatment of conditions commonly associated with severe malnutrition:
1. Vitamin A deficiency
If the child shows any eye signs of deficiency, give orally:
• vitamin A on days 1, 2 and 14 (for age >12 months, give 200,000 IU;
for age 6-12 months, give 100,000 IU; for age 0-5 months, give50,000 IU). If first dose has been given in the referring centre, treaton days 1 and 14 only
If there is corneal clouding or ulceration, give additional eye care to
prevent extrusion of the lens:
• instil chloramphenicol or tetracycline eye drops (1%) 2-3 hourly as
required for 7-10 days in the affected eye
• instil atropine eye drops (1%), 1 drop three times daily for 3-5 days• cover with eye pads soaked in saline solution and bandage
Note: children with vitamin A deficiency are likely to be photophobic and
have closed eyes. It is important to examine the eyes very gently to prevent
rupture.
• hypo-or hyperpigmentation• desquamation• ulceration (spreading over limbs, thighs, genitalia, groin, and behind
• exudative lesions (resembling severe burns) often with secondary
infection, including Candida
Zinc deficiency is usual in affected children and the skin quickly improveswith zinc supplementation (see step 6). In addition:
• apply barrier cream (zinc and castor oil ointment, or petroleum jelly
or paraffin gauze) to raw areas
• omit nappies so that the perineum can dry
Guidelines for the inpatient treatment of severely malnourished children
3. Parasitic worms
• give mebendazole 100 mg orally, twice daily for 3 days
4. Continuing diarrhoea
Diarrhoea is a common feature of malnutrition but it should subside duringthe first week of treatment with cautious feeding. In the rehabilitation phase,loose, poorly formed stools are no cause for concern provided weight gain issatisfactory.
Mucosal damage and giardiasis are common causes of continuing
diarrhoea. Where possible examine the stools by microscopy. Give:
• metronidazole (7.5 mg/kg 8-hourly for 7 days) if not already given
Lactose intolerance. Only rarely is diarrhoea due to lactose intolerance.
Treat only if continuing diarrhoea is preventing general improvement. Starter
F-75 is a low-lactose feed. In exceptional cases:
• substitute milk feeds with yoghurt or a lactose-free infant formula• reintroduce milk feeds gradually in the rehabilitation phase
Osmotic diarrhoea may be suspected if diarrhoea worsens substantially
with hyperosmolar starter F-75 and ceases when the sugar content is
reduced and osmolarity is <300 mOsmol/l. In these cases:
• use isotonic F-75 or low osmolar cereal-based F-75 (see Appendix 5
• introduce F-100 gradually
5. Tuberculosis (TB)
If TB is strongly suspected (contacts with adult TB patient, poor growthdespite good intake, chronic cough, chest infection not responding toantibiotics):
• perform Mantoux test (false negatives are frequent)• chest X-ray if possible
If test is positive or there is a strong suspicion of TB, treat according tonational TB guidelines.
Guidelines for the inpatient treatment of severely malnourished children
D. FAILURE TO RESPOND TO TREATMENT
Failure to respond is indicated by:
1. High mortality
Case fatality rates vary widely: >20% should be considered unacceptable,11-20% poor, 5-10% moderate, and <5% good.
If mortality is >5%, determine whether the majority of deaths occur:
• within 24 hours: consider untreated or delayed treatment of
hypoglycaemia, hypothermia, septicaemia, severe anaemia orincorrect rehydration fluid or volume
• within 72 hours: check whether the volume of feed is too high or the
wrong formulation is used
• at night: consider hypothermia from insufficient covers, no night feeds• when changing to catch-up F-100: consider too rapid a transition
2. Low weight gain during the rehabilitation phase
If weight gain is <5 g/kg/d determine:
• whether this is for all cases (need major management overhaul)• whether this is for specific cases (reassess child as for a new
Possible causes of poor weight gain are:
Check:• that night feeds are given• that target energy and protein intakes are achieved: is actual intake
(offered minus leftovers) correctly recorded? Is the quantity of feedrecalculated as the child gains weight? Is the child vomiting orruminating?
Guidelines for the inpatient treatment of severely malnourished children
• feeding technique: is the child fed frequently and offered unlimited
• quality of care: are staff motivated/gentle/loving/patient?• all aspects of feed preparation: scales, measurement of ingredients,
mixing, taste, hygienic storage, adequate stirring if the ingredientsseparate out
• that if giving family foods, they are suitably modified to provide >100
kcal/100g (if not, re-modify). If resources for modification are limited, orchildren are not inpatients, compensate by replacing F-100 with catch-up F-135 containing 135 kcal/100ml (see Appendix 5 for recipe)
Specific nutrient deficiencies
Check:• adequacy of multivitamin composition and shelf-life• preparation of electrolyte/mineral solution and whether this is correctly
prescribed and administered. If in goitrous region, check potassiumiodide (KI) is added to the electrolyte/mineral solution (12 mg/2500 ml)or give all children Lugol's iodine (5-10 drops/day)
• that, if modified family foods are substantially replacing F-100, electrolyte/
mineral solution is added to the family food (20 ml/day)
If feeding is adequate and there is no malabsorption, some hidden infectioncan be suspected. Urinary tract infections, otitis media, TB and giardiasisare easily overlooked, hence• re-examine carefully• repeat urinalysis for white blood cells• examine stools• if possible, take chest X-ray
Alter the antibiotic schedule (step 5) only if a specific infection is identified.
In children with HIV/AIDS, good recovery from malnutrition is possiblethough it may take longer and treatment failures may be common. Lactoseintolerance occurs in severe HIV-related chronic diarrhoea. Treatment shouldbe the same as for HIV negative children.
Guidelines for the inpatient treatment of severely malnourished children
Check for:• abnormal behaviour such as stereotyped movements (rocking),
rumination (self-stimulation through regurgitation) and attention seeking
Treat by giving the child extra care, love and attention. For the ruminator,firmness, but with affection and without intimidation, can assist.
Guidelines for the inpatient treatment of severely malnourished children
E. DISCHARGE BEFORE RECOVERY IS COMPLETE
A child may be considered to have recovered and be ready for dischargewhen she/he reaches 90% weight-for-length. For some children, earlierdischarge may be considered if effective alternative supervision is available.
Domiciliary care or home-based treatment should be considered only if thefollowing criteria are met:
The child
• is aged >12 months• has completed antibiotic treatment• has good appetite and good weight gain• has taken potassium/magnesium/mineral/vitamin supplement for 2
weeks (or continuing supplementation at home is possible)
• is not employed outside the home• is specifically trained to give appropriate feeding (type, amount and
• has the financial resources to feed the child• lives within easy reach of the hospital for urgent readmission if the
child becomes ill
• can be visited weekly• is trained to give structured play therapy• is motivated to follow the advice given
Local health workers
• are trained to support home care• are specifically trained to examine the child clinically at home, to decide
when to refer him/her back to hospital, to weigh the child, and giveappropriate advice
• are motivated
When children are being rehabilitated at home, it is essential to givefrequent meals with a high energy and protein content. Aim at achievingat least 150 kcal/kg/d and adequate protein intake (at least 4 g/kg/d).
This means feeding the child at least 5 times per day with foods that
Guidelines for the inpatient treatment of severely malnourished children
contain approximately 100 kcal and 2-3 g protein per 100 g. A practicalapproach would be using simple modifications of the usual home foods.
Vitamin, iron and electrolyte/mineral supplements can be continued athome. The carer should be shown how to:• give appropriate meals at least 5 times daily• give high energy snacks between meals (e.g. milk, banana, bread,
biscuits, peanutbutter)
• assist and encourage the child to complete each meal• give electrolyte and micronutrient supplements. Give 20 ml (4
teaspoons) of the electrolyte/mineral solution daily. Since it tastesunpleasant, it will probably need to be masked in porridge, or milk(one teaspoon/200 ml fluid)
• breastfeed as often as the child wants
• World Health Organization, Management of severe malnutrition: a
manual for physicians and other senior health workers. Geneva:World Health Organization, 1999.
• World Health Organization, Management of the child with a serious
infection or severe malnutrition: guidelines for care at the first-referrallevel in developing countries. Geneva: World Health Organization,2000 (WHO/FCH/CAH/00.1).
Guidelines for the inpatient treatment of severely malnourished children
Appendix 1
Weight-for-Height Reference Table
Boys' weight (kg) Lengtha(cm) Girls' weight (kg)
-4 SDb -3 SD -2 SD -1 SD Median
Median -1SD -2SD -3 SD -4 SD
(60%) (70%) (80%) (90%)
(90%) (80%) (70%) (60%)
a Length is measured for children below 85 cm. For children 85 cm or more, height is measured. Recumbent length is on
average 0.5 cm greater than standing height; although the difference is of no importance to individual children, a correction may
be made by subtracting 0.5 cm from all lengths above 84.9 cm if standing height cannot be measured.
b SD: standard deviation score (or Z-score). Although the interpretation of a fixed percent-of-median value varies across age
and height, and although generally the two scales cannot be compared, the approximate percent-of-median values for –1 and –2
SD are 90% and 80% of median, respectively (Gorstein J et al. Issues in the assessment of nutritional status using
anthropometry. Bulletin of the World Health Organization, 1994, 72:273-283).
Guidelines for the inpatient treatment of severely malnourished children
Weight-for-Height Reference Table
Boys' weight (kg) Lengtha(cm) Girls' weight (kg)
-4 SDb -3 SD -2 SD -1 SD Median
Median -1SD
-2SD -3 SD -4 SD
(60%) (70%) (80%) (90%)
(90%) (80%) (70%) (60%)
a Length is measured for children below 85 cm. For children 85 cm or more, height is measured. Recumbent length is on
average 0.5 cm greater than standing height; although the difference is of no importance to individual children, a correction may
be made by subtracting 0.5 cm from all lengths above 84.9 cm if standing height cannot be measured.
b SD: standard deviation score (or Z-score). Although the interpretation of a fixed percent-of-median value varies across age
and height, and although generally the two scales cannot be compared, the approximate percent-of-median values for –1 and –2
SD are 90% and 80% of median, respectively (Gorstein J et al. Issues in the assessment of nutritional status using
anthropometry. Bulletin of the World Health Organization, 1994, 72:273-283).
Guidelines for the inpatient treatment of severely malnourished children
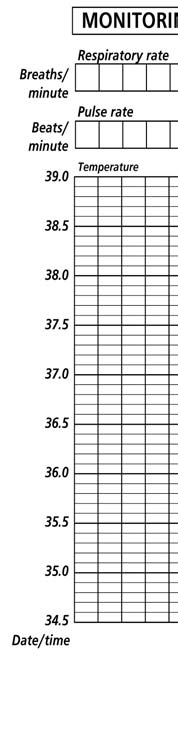
Appendix 2
Monitoring records (temperature, respiratory
rate, and pulse rate)
Monitor respiratory rate, pulse rate and temperature 2-4 hourly until after transition
to F-100 and patient is stable. Then monitoring may be less frequent (e.g., twice daily)
Danger Signs: Watch for increasing pulse and respirations, fast or difficult breathing, sudden increase or decrease in temperature, rectal temperature below 35.5° C, and other changes in condition.
Guidelines for the inpatient treatment of severely malnourished children
Appendix 3
Recipes for ReSoMal & electrolyte / mineral
solution
Recipe for ReSoMal oral rehydration solution
Water (boiled & cooled)
One 1 litre-packet*
Electrolyte/mineral solution (see below)
ReSoMal contains approximately 45 mmol Na, 40 mmol K and 3 mmol Mg/litre.
Recipe for Electrolyte/mineral solution (used in the
preparation of ReSoMal and milk feeds)
Weigh the following ingredients and make up to 2500 ml. Add 20 ml ofelectrolyte/mineral solution to 1000 ml of milk feed.
quantity g molar content of 20 ml
Potassium Chloride: KCl
Tripotassium Citrate: C H K O .H O
Magnesium Chloride: MgCl .6H O
Zinc Acetate: Zn(CH COO) .2H 0
Copper Sulphate: CuSO 5H O
Water: make up to
Note: add selenium if available (sodium selenate 0.028 g, NaSeO 10H 0)
and iodine (potassium iodide 0.012g, KI) per 2500 ml.
* 3.5g sodium chloride, 2.9g trisodium citrate dihydrate, 1.5g potassium chloride, 20g glucose.
Guidelines for the inpatient treatment of severely malnourished children
Preparation: Dissolve the ingredients in cooled boiled water. Store the solution
in sterilised bottles in the fridge to retard deterioration. Discard if it turns cloudy.
Make fresh each month.
If the preparation of this electrolyte/mineral solution is not possible and if pre-mixed sachets (see step 4) are not available, give K, Mg and Zn separately.
• Make a 10% stock solution of potassium chloride (100 g KCl in 1 litre
of water):• For oral rehydration solution, use 45 ml of stock KCl solution instead
of 40 ml electrolyte/mineral solution
• For milk feeds, add 22.5 ml of stock KCl solution instead of 20 ml
of the electrolyte/mineral solution
• If KCl is not available, give Slow K (½ crushed tablet/kg/day)
• Give 50% magnesium sulphate intramuscularly once (0.3 ml/kg up to
a maximum of 2 ml)
• Make a 1.5% solution of zinc acetate (15 g zinc acetate in 1 litre of
water). Give the 1.5% zinc acetate solution orally, 1 ml/kg/day
Guidelines for the inpatient treatment of severely malnourished children
Appendix 4
Antibiotics reference table
Summary: Antibiotics for Severely Malnourished
Children
Cotrimoxazole oral (25 mg sulfamethoxazole
+ 5 mg trimethoprim / kg) every 12 hours for 5
days
Gentamicin1 IV or IM (7.5 mg/kg), once daily
(shock, hypoglycaemia,
for 7 days, plus:
hypothermia, dermatosiswith raw skin/fissures,
Ampicillin IV or
Followed by: Amoxicillin2
respiratory or urinary tract
oral (15 mg/kg), every
infections, or lethargic/sickly
every 6 hours for 2
8 hours for 5 days
If child fails to improve within Chloramphenicol IV or IM (25 mg/kg), every
48 hours, ADD:
8 hours for 5 days (give every 6 hours ifmeningitis is suspected.)
If a specific infection
Specific antibiotic as directed on pages
requires an additional
30 - 33 of the manual Management of Severe
1 If the child is not passing urine, gentamicin may accumulate in the body and cause deafness. Do
not give the second dose until the child is passing urine.
2 If amoxicillin is not available, give ampicillin, 50 mg/kg orally every 6 hours for 5 days.
Guidelines for the inpatient treatment of severely malnourished children
Doses for specific formulations and body
weight ranges
DOSE ACCORDING TO CHILD'S WEIGHT
6 up to 8kg 8 up to 10kg
every 8 hours for Syrup, 125 mg/5ml
Syrup, 250 mg/5ml
every 6 hours for5 days
Vial of 500 mg mixed
every 6 hours for with 2.1 ml sterile water2 days
to give 500 mg/2.5 ml
Cotrimoxazole Oral: 25mg SMX + Tablet,
sulfamethoxazole 5 m g T M P / k g 100 mg SMX + 20mg TMP+ trimethoprim, every 12 hours for Syrup, 200 mg SMX
Oral: 7.5 mg/kg Suspension,
every 8 hours for 200 mg/5ml7 days
every 6 hours for5 days
Benzylpenicillin IV or IM:
IV: Vial of 600 mg mixed 2 ml
50 000 units/kg with 9.6 ml sterile waterevery 6 hours for to give 1 000 000 units/5 days
10 mlIM: Vial of 600 mg mixedwith 1.6 ml sterile water 0.4 ml
to give 1 000 000 units/2 ml
Guidelines for the inpatient treatment of severely malnourished children
Doses for selected antibiotics, for specific
formulations and body weights
DOSE ACCORDING TO CHILD'S WEIGHT
(use closest weight)
Chloramphenicol IV or IM:
mixed with 9.2 ml 0.75 1 1.25 1.5 1.75 2 2.25 2.5 2.75
every 8 hours sterile water to(or every
6 hoursif suspect of IM: vial of 1 gmeningitis)
mixed with 3.2 ml 0.3 0.4 0.5 0.6 0.7 0.8 0.9
sterile water togive 1 g/4 ml
2.25 3 3.75 4.5 5.25 6 6.75 7.5 8.25
(2 ml at 10 mg/ml),
IV/IM: vialcontaining 80 mg
2.25 3 3.75 4.5 5.25 6 6.75 7.5 8.25
(2 ml at 40 mg/ml),mixed with 6 mlsterile water togive 80 mg/8ml
IV/IM: vialcontaining 80 mg
0.5 0.75 0.9 1.1 1.3 1.5 1.7
(2 ml at 40 mg/ml),undiluted
Doses for iron syrup for a common formulation
Dose of iron syrup: ferrous fumarate100 mg/5 ml (20 mg elemental iron per ml)
Guidelines for the inpatient treatment of severely malnourished children
Appendix 5
Recipes for starter and catch-up formulas
Dried skimmed milk (g)*
Vegetable oil (g)
30 (or 35 ml) 60 (or 70 ml)
Water: make up to
Contents per 100 ml
Energy (kcal)
% energy from protein
% energy from fat
Osmolarity (mOsmol/1)
• using an electric blender: place some of the warm boiled water in
the blender, add the milk powder, sugar, oil and electrolyte/mineralsolution. Make up to 1000 ml, and blend at high speed
• if no electric blender is available, mix the milk, sugar, oil and electrolyte/
mineral solution to a paste, and then slowly add the rest of the warmboiled water and whisk vigorously with a manual whisk
• store made-up formula in refrigerator
Guidelines for the inpatient treatment of severely malnourished children
F-75 starter formulas
• full-cream dried milk 35 g, 100 g sugar, 20 g (or ml) oil, 20 ml electrolyte/
mineral solution, and make up to 1000 ml
• full-cream cow's milk (fresh or long life) 300 ml, 100 g sugar, 20 g (or
ml) oil, 20 ml electrolyte/mineral solution and make up to 1000 ml
F-100 catch-up formulas
• full-cream dried milk 110 g, 50 g sugar, 30 g (or ml) oil, 20 ml electrolyte/
mineral solution, and make up to 1000 ml
• full-cream cow's milk (fresh or long life) 880 ml, 75 g sugar, 20 g (or ml)
oil, 20 ml electrolyte/mineral solution and make up to 1000 ml
F-135 catch-up formulas
This is for use in special circumstances (see Section D2, poorweight gain) for children aged > 6 months
• full-cream dried milk 130 g, 70 g sugar, 40 g (or 45 ml) oil, 20 ml
electrolyte/mineral solution, make up to 1000 ml
• full-cream cow's milk (fresh or long life) 880 ml, 50 g sugar, 60 g (or 65
ml) oil, 20 ml electrolyte/mineral solution (this makes 1000 ml)
Isotonic and cereal based F-75
• cereal-based, low-osmolar F-75 (334 mOsmol/l). Replace 30 g of the
sugar with 35 g cereal flour in F-75 recipes above. Cook for 4 min.
This may be helpful for children with osmotic diarrhoea
• isotonic versions of F-75 (280 mOsmol/l) are available commercially
from Nutriset. In these, maltodextrins replace some of the sugar, andall the extra nutrients (K, Mg and micro-nutrients) are incorporated
Guidelines for the inpatient treatment of severely malnourished children
Appendix 6
Volume of F-75 to give for children of different weights
(see Appendix 7 for children with severe (+++ oedema)
Volume of F-75 per feed (ml)a
80% of daily totala
of child Every 2 hoursb Every 3 hoursc
a Volumes in these columns are rounded to the nearest 5 ml.
b Feed 2-hourly for at least the first day. Then, when little or no vomiting, modest diarrhoea (<5 watery stools per day),
and finishing most feeds, change to 3-hourly feeds.
c After a day on 3-hourly feeds: If no vomiting, less diarrhoea, and finishing most feeds, change to 4-hourly feeds.
Guidelines for the inpatient treatment of severely malnourished children
Appendix 7
Volume of F-75 for children with severe (+++) oedema
Volume of F-75 per feed (ml)a
+++ oedema Every 2 hoursb Every 3 hoursc
a Volumes in these columns are rounded to the nearest 5 ml.
b Feed 2-hourly for at least the first day. Then, when little or no vomiting, modest diarrhoea (<5 watery stools per day),
and finishing most feeds, change to 3-hourly feeds.
c After a day on 3-hourly feeds: If no vomiting, less diarrhoea, and finishing most feeds, change to 4-hourly feeds.
Guidelines for the inpatient treatment of severely malnourished children
Appendix 8
Range of volumes for free feeding with F-100
Range of volumes per 4-hourly feed
Range of daily volumes of F-100
of F-100 (6 feeds daily)
a Volumes per feed are rounded to the nearest 5 ml.
Guidelines for the inpatient treatment of severely malnourished children
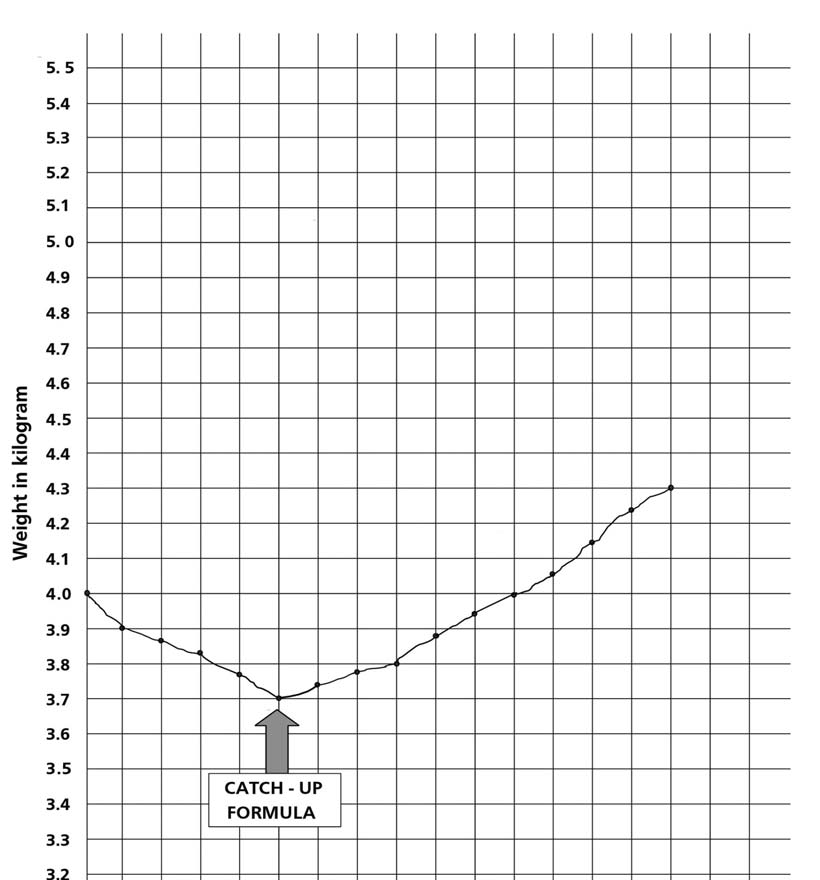
Appendix 9
Weight record chart
Name: Sipho age 14 months, sex: male, wt on admission: 4 kg, ht: 65 cm, oedema ++
Guidelines for the inpatient treatment of severely malnourished children
Appendix 10
Structured play activities
Play therapy is intended to develop language skills and motor activitiesaided by simple toys. It should take place in a loving, relaxed and stimulatingenvironment.
Language skills
At each play session:
• teach local songs and finger and toe games• get child to laugh and vocalise, repeat what (s)he says• describe all activities• teach action words with activities e.g. ‘bang bang' as (s)he beats a
drum, ‘bye bye' as (s)he waves etc.
• teach concepts at every opportunity, examples are in italics in the
Motor activities
Encourage the child to perform the next motor milestone e.g.:
• bounce the child up and down and hold him/her under the arms so
that the feet support the child's weight
• prop the child up, roll toys out of reach, encourage the child to crawl
• hold hand and help the child to walk• when starting to walk alone, give a ‘push-along' and later a ‘pull-
along' toy
Activities with toys
Simple toys can easily be made from readily available materials. These
toys can be used for a variety of different motor activities:
‘Ring on a string'
• Swing the ring within reach and tempt the child to grab it• suspend ring over the crib and encourage the child to knock it and
• let child explore the ring, then place it a little distance from child with
the string stretched towards him/her and within reach. Teach the childto retrieve the ring by pulling on the string horizontally
• sit child on lap, then holding the string, lower the ring towards the
ground. Teach child to get the ring by pulling up on the string vertically.
Also teach child to dangle the ring.
Guidelines for the inpatient treatment of severely malnourished children
‘Rattle and drum'
• Let the child explore rattle. Show child how to shake it saying ‘shake
• encourage child to shake the rattle by saying ‘shake' but without
• teach child to beat drum with shaker saying ‘bang bang'• roll drum out of reach and let child crawl after it, saying ‘fetch it'• get child to say ‘bang bang' as (s)he beats drum
‘In and Out' toy with blocks
• Let the child explore blocks and container. Put blocks into container
and shake it, then teach child to take them out, one at a time, saying‘out' and ‘give me'
• teach the child to take out blocks by turning container upside down• teach the child to hold a block in each hand and bang them together• let the child put blocks in and out of container saying ‘in' and ‘out'• cover blocks with container saying ‘where are they, they are under
the cover'. Let the child find them. Then hide them under two and thenthree covers (e.g. pieces of cloth)
• turn the container upside down and teach the child to put blocks on
top of the container
• teach the child to stack blocks: first stack two then gradually increase
the number. Knock them down saying, ‘up up' then ‘down'. Make agame of it
• line up blocks horizontally: first line up two then more; teach the child
to push them along making train or car noises. Teach older childrenwords such as stop and go, fast and slow and next to. After thisteach to sort blocks by colour, first two then more, and teach high andlow building. Make up games
• Put an object in the bottle, shake it and teach the child to turn the
bottle upside down and to take the object out saying ‘can you get it?'Then teach the child to put the object in and take it out. Later try withseveral objects
Guidelines for the inpatient treatment of severely malnourished children
Stacking bottle tops
• Let the child play with two bottle tops then teach the child to stack
them saying ‘I'm going to put one on top of the other'. Later, increasethe number of tops. Older children can sort tops by colour and learnconcepts such as high and low
• Sit the child on your lap. Get the child to turn the pages, pat pictures
and vocalise. Later, let the child point to the picture you name. Talkabout pictures, obtain pictures of simple familiar objects, peopleand animals. Let older children name pictures and talk about them
• Teach the word ‘baby'. Let the child love and cuddle the doll. Sing
songs whilst rocking the child
• teach the child to identify his/her own body parts and those of the doll
when you name them. Later (s)he will name them
• put the doll in a box as a bed and give sheets, teach the words ‘bed
and sleep' and describe the games you play
Guidelines for the inpatient treatment of severely malnourished children
Appendix 11
Discharge card
Guidelines for the inpatient treatment of severely malnourished children
Recommendations for Feeding During Sickness and Health* A good daily diet should be adequate in quantity and include an energy-rich food (for example, thick cereal with added oil); me fish, eggs, or pulses; and fruits and vegetables
Guidelines for the inpatient treatment of severely malnourished children
Guidelines for the inpatient treatment of severely malnourished children
Publications of the World Health Organization can be obtained from:
World Health Organization
Regional Office for South-East Asia
World Health House
Indraprastha Estate
New Delhi - 110 002, India
Telephone : 91-11-23370804
Fax : 91-11-23370197
website : [email protected]
Marketing and Dissemination
World Health Organization
20 Avenue Appia,
1211 Geneva 27, Switzerland
Telephone : +41-22-791 2476
Fax : +41-22-791 4857
website : [email protected]
For further information please contact:
Dr Sultana Khanum
Department of Nutrition for Health and Development
World Health Organization
20 Avenue Appia, 1211 Geneva 27, Switzerland
Telephone : +41-22-791 2624
Fax : +41-22-791 4156
website : www.who.int.org
Guidelines for the inpatient treatment of severely malnourished children
Source: http://www.imtf.org/_uploads/who-guidelines-english.pdf
Safe harbor This presentation may include forward-looking statements that are based on our management's beliefs andassumptions and on information currently available to our management.The inclusion of forward-looking statements should not be regarded as a representation by Cosmo that any ofits plans will be achieved. Actual results may differ materially from those set forth in this presentation due tothe risks and uncertainties inherent in Cosmo's ability to develop and expand its business, successfullycomplete development of its current product candidates and current and future collaborations for thedevelopment and commercialisation of its product candidates and reduce costs (including staff costs), themarket for drugs to treat IBD diseases, Cosmo's anticipated future revenues, capital expenditures and financialresources and other similar statements, may be "forward-looking" and as such involve risks and uncertaintiesand risks related to the collaboration between Partners and Cosmo, including the potential for delays in thedevelopment programs for Budesonide MMX® and Rifamycin SV MMX®. No assurance can be given that theresults anticipated in such forward looking statements will occur. Actual events or results may differ materiallyfrom Cosmo's expectations due to factors which include, but are not limited to, increased competition, Cosmo'sability to finance expansion plans, the results of Cosmo's research and development activities, the success ofCosmo's products, regulatory, legislative and judicial developments or changes in market and/or overalleconomic conditions. Cosmo assumes no responsibility to update forward-looking statements or to adapt themto future events or developments.You are cautioned not to place undue reliance on these forward-looking statements, which speak only as ofthe date hereof, and Cosmo undertakes no obligation to revise or update this presentation.
ResearchOnline@GCU Glasgow Caledonian University Short-term therapy with rosiglitatzone, a PPAR-¿ agonist improves metabolic profileand vascular function in non-obese lean wistar rats Naderali, Mohammad M.; Itua, Imose; Abubakari, Abdul-Razak; Naderali, Ebrahim K. Published in: ISRN Pharmacology Publication date: Document Version