Londonkneeclinic.com


London Knee Clinic
Partial Knee Joint ReplacementPatient information brochure
New mobility with a partial knee replacement


This brochure has been written for patients, family mem-bers and all those who wish to know more about the partial replacement of a knee joint. It will answer basic questions, explain the principle of the implantation of a partial knee joint as well as the procedure, and relieve you of any misgiv-ings or fears you may have.
Please note that this information cannot replace a conver-sation with a specialist.
You are most likely reading this brochure because your con-sultant has already diagnosed osteoarthritis affecting part of the knee in you or in someone close to you. We are sure that your doctor has prescribed other methods of treat-ment, such as drugs, physiotherapy or remedial excercise. Yet such treatment methods rarely have a long-term, last-ing effect when a part of the joint is severely damaged by arthritis.
Pain – especially chronic pain – can become a major prob-lem, and may restrict both quality of life and mobility. When part of the knee is severely damaged it is often the case that only a partial or in some cases a complete knee replacement can bring relief. After such an operation, nearly all patients completely recover their lost mobility, their freedom from pain, and thus their quality of life.
Glyn Evans
Consultant Orthopaedic Surgeon
London Knee Clinic

1. The knee joint
2. What is arthritis?
3. How does arthritis occur?
4. Treatment methods
5. The partial knee replacement
6. Prior to the hospital
7. What happens at the hospital?
8. The operation
9. Risks and complications
10. After the operation
11. The follow-up treatment
12. Sports
13. The implant passport
14. Tips and exercises at home
15. Frequently asked questions
16. Epilogue


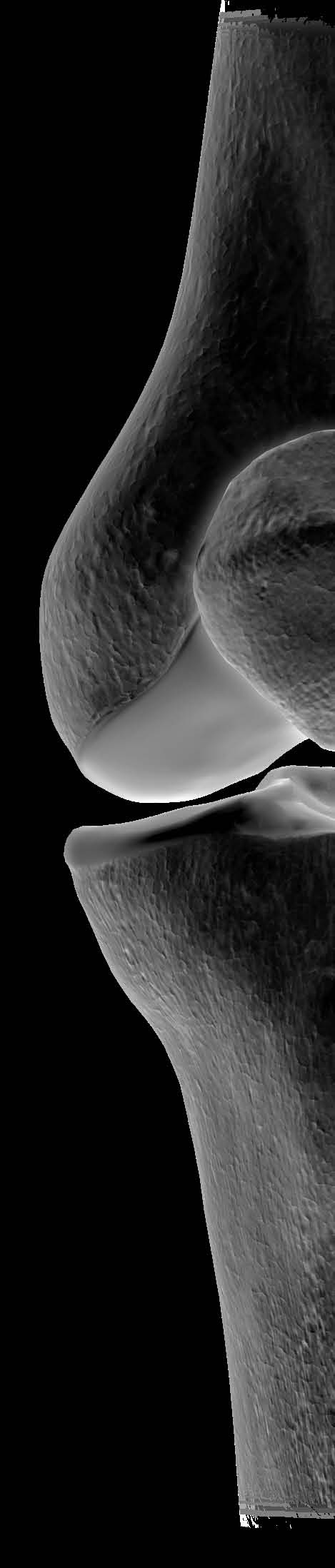
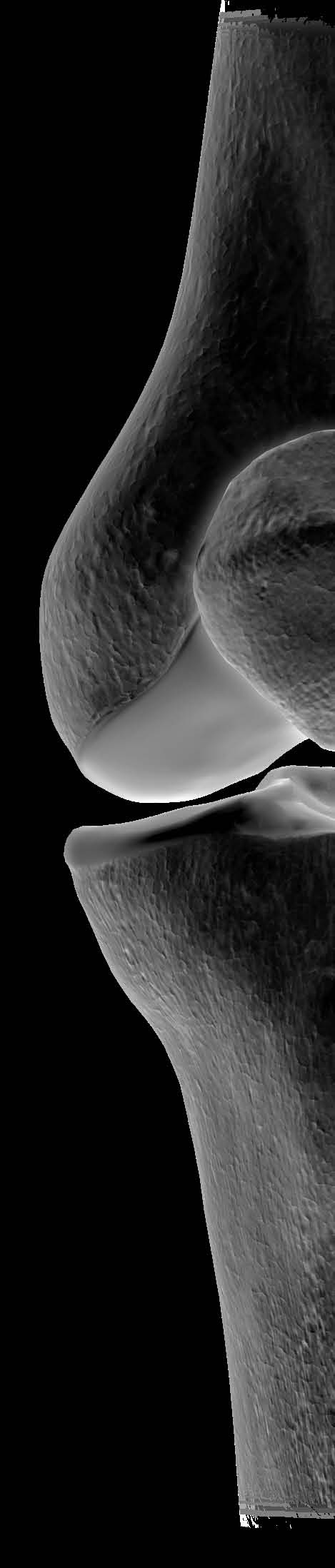
1. The knee joint
The knee joint is the largest joint in the
Thigh bone (femur)
human body and consists of three bones, the movements of which are guided exclu-sively by muscles, ligaments and tendons. Two crescent-shaped cartilaginous discs are located between the femoral bone and the tibial bone on the inner and outer side of the knee joint. These discs distribute the load on the joint over a large area and act as a buffer or shock-absorber system. Their structure is clearly different from that of the articular cartilage. The latter is a 1–2mm layer that covers the entire bone surface within the
Medial femoral condyle
joint. An elastic and aqueous tissue, the ar-ticular cartilage provides a low-friction gliding surface.
Medial surface of tibia
Tibia (shin bone)
Left knee seen from in front
Lateral femoral condyle
Lateral surface of the tibia
Injury or damage to these structures is often irreparable and can over the medium to long term lead to articular wear – better known as arthritis.
The knee joint is divided into three
The medial femoral condyle and medial
surface of the tibia.
The lateral femoral condyle and lateral
surface of the tibia.
The deep surface of the patella and the
corresponding surface of the front of the femur.
2. What is osteoarthritis?
Arthritis is a degenerative joint disease which
Thigh bone (femur)
causes inflammation and damage to the sur-
face of the joint.
The wearing down ( ) of the articular carti-lage is a natural symptom of aging and may involve articular wear. Like other types of tis-
sue in the human body (such as the skin), ar-ticular cartilage is able to heal or repair itself, however, articular cartilage heals only slowly. If the rate of wear exceeds the rate of repair,
progressive loss of the articular cartilage oc-curs and this leads to painful functional im-
As a consequence, the cartilage gets thinner and increasingly uneven and the fluid that lu-bricates the joint, increases in quantity caus-
ing the knee joint to swell.
Mobility worsens steadily and the person con-cerned suffers from more severe pain.
In addition, the joint can form osteophytes otherwise called ‘bony spurs'. This is the body's attempt to heal, a process that is, how-ever, not entirely effective.
Pain is the main symptom of arthritis. The pain frequently causes the sufferer to rest the joint. This in turn causes the condition of the carti-lage, which needs movement for its nutrition, to deteriorate.
The most frequent form of knee arthritis is osteoarthritis. This is currently considered a typical symptom of old age, but can also arise as a consequence of injury. The disease develops slowly over the course of years. In many cases the cartilage is already irremedi-ably damaged by the time pain and restricted movements occur.
3. How does arthritis occur?
The complex process of the formation of arthritis has yet to be clarified. Orthopaedic surgeons are able to treat the symptoms, but preventing the causes of the disease is not always possible.
It is known that factors such as overweight or inappropriate straining of a joint, due for instance to a congenital malposition or frequent bearing of heavy loads, favour the formation of arthritis. People who constantly and excessively overstrain their joints (such as competitive athletes), or those who suffer from injuries involving damage to the joint, are especially at risk.
Severe medial joint compartment wear
Especially in the knee, the shape and the align-ment of the bones must be correct. Changes in the shape or alignment and in the mus-culature or in the ligamentous apparatus will tend to give rise to arthritis. In principle, any disease of the articular cartilage, the synovial membrane or the synovial fluid can lead to arthritis.
4. Treatment methods
Before considering a partial knee replace-ment, doctors use other non-operative treat-ment methods to alleviate pain:
Analgesic, anti-inflammatory drugs
(e.g. Voltarol®, Brufen®, etc.)
A change of lifestyle (with regard to sports,
weight, nutrition etc.)
The use of orthopaedic aids such as a
crutch, a stick or an elasticated support
Physiotherapy and regular gentle exercise
Arthroscopy (smoothing down of the
surfaces and removal of debris etc.)
Hyaluronan injection into the knee
None of these measures, however, have a long term and lasting effect. All too frequent-ly, only an artificial joint replacement either partial or total can really alleviate the problem and restore mobility.
5. The partial knee replacement
Your surgeon has recommended that you have a partial knee replacement (or unicom-partmental knee) operation because you have arthritis that has caused damage to one part of your knee joint.
The aim of the implantation of the partial knee joint is to alleviate pain, restore the nat-
Femoral component
ural function and mobility of the knee and to return the patient to near normal activities. Nevertheless, a partial knee replacement will never be able to completely replicate the
function of the natural joint.
Thigh bone (femur)
Femoral component
Your doctor will explain the operation and itscourse in advance, and tell you as well what type of knee implant will be used. The exact
Insertof the tibial
condition of the joint, however, will only be-
come evident during the intervention itself.
It is therefore possible that your doctor wil
have to deviate from the operating procedure
The partial knee replacement
A partial knee procedure only replaces the
damaged compartment* of the knee and
preserves the healthy structures such as bone,
cartilage and ligaments that have been unaf-
fected by the disease process.
By treating the arthritis at an early stage, where it has not progressed to the entire joint, functional outcomes and natural knee move-ment can be more completely restored.
* Surgeons tend to consider knees as having three compartments:
the medial compartment: the femur and
the tibia on the inside of the knee
the lateral compartment: between the
femur and the tibia on the outside of the knee
and the patellofemoral compartment:
between the back of the patella/knee cap and the front of the femur or trochlea
6. Prior to the hospital
You can prepare your home optimally
for the time after the operation:
Remove rugs and mats, obtrusive cables
and any other objects on which the crut- ches might get caught or which could cause you to slip.
Place objects you use daily (tableware,
clothes, drugs etc.) at a reachable height.
Place various aids in the bathroom:
handholds, a non-skid shower mat, increase the height of your toilet seat if necessary.
6. Prior to the hospital
Place an electric torch close to your bed,
if you cannot activate the light switch from there. This will prevent you from tripping over things when you have to get up at night.
Prepare your food by deep-freezing it so
that you need only heat it up later. You can save yourself a lot of kitchen work in the first days.
You will be examined thoroughly before the operation. This will help to identify any pos-sible risks early on and allow medical staff to take the necessary prophylactic measures. Your doctor will inform you about drugs and anaesthetics.
7. What happens at the hospital?
Your examination may include the
following questions and items of
information:
Do you suffer from cardiovascular prob-
lems or high blood pressure? If so, are your medications well regulated? The nursing staff will measure them and possibly conduct an ECG.
Are you prone to infection? If you suffer
from diabetes, how well does your thera- py work? A blood sample may be taken before the operation to clarify these ques- tions.
Your weight has an influence on the
success of the operation. Are you over- weight? You may be offered a session with a nutritionist.
Smoking is a general risk factor – you
might like to take the operation as an opportunity to quit. Smoker counselling is available in the hospital.
Do you take anticoagulant or platelet
inhibiting drugs (Aspirin® or Warfarin)? If so, they will be stopped prior to the operation and, if necessary, you will receive a substitute by injection.
The anaesthetist will inform you about
the best form of anaesthesia for you.
You will always have the opportunity to
pose your own questions to the operating surgeon or to a ward physician.
8. The operation
In the operation of partial knee replacement, the diseased bone and tissue are removed and the remaining bone is shaped with the operating instruments to allow the components to fit exactly.
Operating on the joint comprises the following four steps:
Step 1
The surgeon makes an appropriate length in-
cision down the front of the knee and flexes
the joint. The surgeon removes the meniscus
and any other structures that are impairing the
normal movement of the joint and any pos-
sible osteophytes. Using the implant specific
instruments supplied by the manufacturer of
the prosthesis, the surgeon cuts and shapes
the bone to the correct shape to match the
internal geometry of the components to be
implanted.
The knee joint is prepared for the prosthesis; the defect can be seen clearly.
Step 2
After the final cut has been made and all the
holes drilled, a trial prosthesis is inserted. This
allows the exact size and optimal position of
the implant to be determined. This step is de-
cisive for subsequent mobility and stability.
The femur and tibia are trimmed in such a way that the implant will fit exactly.
Step 3
The surgeon implants the components and
fixes them with bone cement. It is a stable
connection between the surface of the im-
plant and the bone. The bone cement is very
compatible and hardens fully in a few min-
utes.
The two individual components of thepartial knee replacement are put into place; the knee is once again fully functional.
Step 4
The surgeon sutures the joint layer by layer
before applying a compression dressing.
X-ray check of the implant following asuccessful operation: the fit is optimal.
9. Risks and complications
Strictly speaking, every operation involves
both general and specific risks. The surgical
team always endeavours to treat you in the
best possible way and to avoid any complica-
tion. The best possible state of health helps to
reduce the risks.
The general risks include:
The formation of a leg-vein thrombosis
(vascular occlusion by a blood clot)
The formation of a pulmonary embolism
(partial or complete occlusion of a pulmonary vessel by a blood clot)
Infections In rare cases, injury to blood vessels or
The administration of blood-thinning drugs (such as Heparin) reduces the risk of a leg-vein thrombosis or pulmonary embolism.
Risks specific to a knee operation are adhe-sions and joint stiffness, which can occur if the knee is not moved sufficiently in the days im-mediately following the operation. Intensive physiotherapy helps to prevent this.
Please inform your surgeon or hospital imme-diately if you experience any new onset of pain in the area of the operation, there is any swelling, the wound is not healing properly, there is any discharge of fluid from the scar or you have an unexplained fever.
10. After the operation
After your operation you will be transferred to the recovery ward and once you are fully awake, you will return to the ward where you will have an x-ray to check the position of the knee replacement.
The day following your surgery, the physi-otherapist will help you to start walking with the help of crutches or a walking frame. You will be able to go home two days after your surgery unless there is a medical reason for you to stay longer.
If you have any worries or queries while you are in the hospital, ask a member of the healthcare team who will be able to offer re-
Abide by the following precautionary
assurance or treat any complication you may
measures in order not to put the healing
process at risk:
Do not carry excessively heavy objects! A
rucksack for a better load distribution is recommended particularly during the period in which you are using crutches.
Long periods standing, excessive stair-
climbing and long walks put increased strain on your knee – keep such activities to a reasonable minimum.
Do not cross your legs when sitting.
Avoid heavy physical work as well as risky
situations (climbing a ladder etc.).
Do not kneel down in the first month! Good shoes protect the joint from
overload and keep you safe.
11. The follow-up treatment
Regular follow-ups by a specialist help to verify your recovery. You will receive new instructions if necessary.
Contact your doctor as soon as possible if you experience problems between follow-up controls.
It is quite normal to experience some limi-tations up to a year after the operation – improvement occurs gradually, but steadily.
You may require to use crutches for a peri-od after your operation as advised by your specialist. As long as you depend on them, you will need assistance in the household or for shopping. If you live alone you can enlist the aid of a nursing service. The hospital will inform you about the various services on offer.
We recommend physical exercise, as it im-proves the quality of your social and physical life and prevents illness.
Aspire to good mobility and increased musclestrength following the insertion of your par-tial knee replacement. Well-developed thigh muscles stabilise the knee joint considerably.
It is important that you increase your physi-cal load appropriately and that you take pain seriously: as a warning sign. It is generally ac-cepted that a lack of exercise has a negative influence on a partial knee replacement.
Perhaps you were already involved in sports activities before the operation. If so, your phy-sician can tell you whether you should con-tinue with them now that you have a partial knee replacement. It is generally advisable toabstain from sports which place inordinate stress on joints, or which pose a high risk of in-jury (such as football, martial arts and skiing).
Your safety is the top priority! Joint injuries
and fractures in people who have an implant often have serious consequences. Train your-self to move somewhat more slowly and pre-pare for a gentler sequence of movements. You may still do Nordic walking and gymnas-tics, go bowling, golfing, biking etc., and play team sports, but with restrictions. In case of doubt, please ask your specialist or the ope-rating clinic.
Always keep in mind that your new freedom from pain can quickly lead to an overload!
13. The implant passport
You will receive an implant passport when you leave the hospital. Please always carry this passport on you! It can be very helpful in case
of injuries of the joint or complications out-
side of your usual surroundings (on vacation
or at airport controls, for instance).
TownTelephoneSurgeon NameDate of Surgery
Item no. 336.040.022 1/1 2/2010
Mathys Ltd Bettlach Printed in Switzerland
14. Tips and exercises at home
In the first six to eight weeks following the operation the new joint is still unprotected, as the musculature has atrophied. It is now necessary to build it up again and to strengthen it, so as to restore the necessary stability and protect your knee against the wrong movements.
The following pages include tips and practical advice on how to pursue your daily routine. The aim is to restore your freedom of movement as quickly as possible, hence your active cooperation is indispensable.
Please consult your attending physician or your physiotherapist if you are uncertain about the following exercises or if you do not fully understand them.
Use the crutches correctly
To stand, place the two crutches a bit in
front and to the side of your feet.
Keep your hips as straight as possible.
A slightly bent elbow will permit you to do so.
Support yourself firmly on the handles of
the crutches when walking.
Important: carry your weight on your
hands – and not on your forearms!
Always load the operated knee as you
were shown at the clinic, but walk as nor- mally as possible. This means that each step should be of the same length, as in normal walking. Load the operated leg with no more than the permitted load.
If you are permitted to use one single
crutch, use it on the healthy side.
Going up and down the stairs
Important: do not attempt your first trials on
the stairs alone!
Set the healthy leg on the first step of the
Push your weight with the healthy leg and
with your hands, so that you are able to lift the operated leg to the same step.
Repeat this until you have reached the
halfway mark or landing.
Proceed exactly the same way even if the
stairs have banisters.
Place both crutches on the first step.
Put the operated leg on the same step.
Take care to put as much weight as
possible on the crutches.
Place the healthy leg on the same step.
If your healthy leg is strong enough, you
can try to put the crutches and the opera- ted leg on the next step at the same time and to make the healthy leg follow.
Abstain from sitting in deep armchairs,
especially during the early days.
Ideal are high, stable chairs with armrests.
If necessary, you can increase the height of your seat with a pillow.
To sit down: move backwards to the chair
until you feel its edge.
Move both crutches to the side of the
healthy leg.
Support yourself on the armrests to sit
down – stretch the operated leg slightly forward.
Angle your legs slightly and sit upright.
Slip forward to get up. Use the armrests
to stand on your healthy leg. Continue to stretch out the operated leg slightly.
Take the crutches in both hands to stand
on the operated leg.
Going to the bathroom
Move both crutches to the healthy side.
Grip either an armrest on the toilet (if available) or a handhold next to the toilet.
Sit down slowly and stretch out the
operated leg slightly.
Get up as from a chair: support yourself
on the armrests or on the handhold. Put the operated leg slightly forward.
Having a shower
To keep your balance, use an anti-skid
mat (not illustrated) and a handhold on the wall.
Mix the water to the right temperature
before taking a shower.
Start by putting the healthy leg into the
shower. The crutches remain outside the shower, but close by.
A sponge with a long handle keeps you
from having to bend forward.
Leave the shower with the operated leg
Taking a bath
Bathing is not recommended in the first 2-3
weeks following the operation. If you do not
have a shower, the following tips will show
you how to get in and out of the bathtub.
Go to the broad side of the bathtub on
your crutches.
Mix the water to the right temperature
before entering the tub.
To get into the tub, sit down on the edge
or on a chair (not illustrated) which is higher than the bathtub and positioned directly next to it.
Lift the operated leg first and then the
healthy one over the edge. If possible, sit down opposite the water tap when you are on the edge of the tub. Place your hands under the femur to lift the leg in the tub.
Lift your legs carefully over the edge to
leave the bathtub.
Going to bed
Sit down backwards on the bed in the
vicinity of the head end.
Move your bottom slightly backwards and
lift the healthy leg onto the bed.
The operated leg is next: if you do not
yet have enough strength to lift it yourself, support it with the healthy leg or place your hands under the femur for support. Now you can lie on your back.
Important: move your pelvis and legs
evenly. Keep your legs slightly spread.
Stand first on the operated leg. Use your
hands to assist you. Stretch the leg slightly forward to get your balance. Now lift the healthy leg from the bed.
The best thing is to sleep on your back.
If you prefer to sleep on your side, place
a pillow between your legs to prevent them from crossing in your sleep and your hip from turning on one side.
Getting dressed
Select comfortable clothing.
You will need help from others at first, or
a dressing aid. If you choose a dressing aid, use the hook to grasp the waistband of your clothing and pull it first over the operated leg and up over the knee.
Use a crutch to stand on the healthy leg
and then finish putting on the item of clothing.
Remove the clothing from the healthy leg
Flat, firm shoes that are easily slipped on
and do not have shoelaces are best, as you do not have to bend over to put them on.
Pay attention to good soles. Leather soles
are unsuitable, as they are very hard and do not absorb shocks.
Use a dressing aid or a shoehorn with an
extra long handle.
In the kitchen
An apron with several pockets can be of
Transport hot fluids in containers with a lid. Slide things on the counter or working
surface instead of carrying them.
Take small steps instead of turning your
body; do this when walking as well.
Use gripping pliers to pick up objects.
Do not bend when reaching for something
in a lower drawer or in an oven – keep the operated leg extended.
You may also sit on a chair. Position it so
that the operated leg is turned toward the drawer or the oven.
Use a trolley to transport tableware. It will
also help you avoid unnecessary extra trips.
In the car
Do not drive a car until your doctor per-
Get into the car on the side with the most
legroom (normally the passenger side).
Sit down backwards on the car seat.
Lift your legs carefully and slowly into the
car. Support your legs with your hands under the femur or with the healthy leg.
Important: move your pelvis and legs as
uniformly as possible and keep your body as straight as possible.
Taking a walk
Begin taking regular walks on well-con-
structed paths soon after the operation. Start with a short walk of five to ten minutes.
Gradually increase your walking distance.
Important: avoid uneven and slippery
roads. Always wear sturdy shoes.
Move your knee joint as much as possible.
Sit down on a chair and place a towel on the smooth floor. «Mop» the floor by moving the towel back and forth.
If you have a home exercise cycle and
achieve sufficient flexion of the knee joint, then use it daily for about ten minutes on low resistance. Keep the seat up high.
15. Frequently asked questions
On the following pages, you will find the answers to questions frequently asked by patients. Some of the answers may be of assistance to you.
How can I help to make the operation a success?
If you can, stop smoking as far in advance of your surgery as possible. This will reduce the chances
of you having any complications whilst under anaesthetic and will also benefit your health in the
long term. Help and advice are available from www.nhs.uk/smokefree or your GP.
If you are overweight you are at a higher risk of developing complications. Advice on following a healthy diet is available from www.eatwell.gov.uk or your GP.
Taking regular exercise improves lung function, boosts the immune system, helps control weight and improves your mood. It also helps to reduce the risk of some medical conditions and heart disease. Advice is available from www.nhs.uk/livewell/fitness but consult your GP before you start any exercise program.
How long will my implant last?
It is possible that your partial knee replacement will wear out with time, depending on your weight
and how physically active you are. Eventually a worn knee replacement will need to be replaced
although most partial knee replacements will last between 10 and 15 years.
Have a check x-ray of your partial knee replacement every two years to check for any problems
such as loosening of the joint.
I occasionally have an allergic reaction to metal. Is that a problem?
Inform your consultant of your allergies. If available, provide him with your allergy passport. The
materials used for the implants and the coatings very rarely cause an allergic reaction. Special ma-
terials or coatings are required in only a few cases.
I feel very well after the operation – do I have to go to the follow-ups anyway?
You should observe your follow-up dates without fail, even if you are not in pain and feel well.
They allow your specialist to keep track of your rehabilitation and to recognise complications early
on. In the first year after the operation, several follow-up examinations will take place. Later, these
examinations will be required only once a year, then every two or three years. Your doctor will
determine the ideal interval.
I am in great pain – yet I was told to wait a bit longer before the implantation of a partial
knee joint. Is this correct?
Although it is ultimately up to the patient whether and when to have a partial knee replacement,
the decision should be taken in consultation with a specialist. The essential factors that influence
such a decision are as follows:
In your medical checkups and X-ray pictures, your specialist has found advanced arthritis of
Pain interferes so much with your quality of life that you are no longer able to cope with the
daily routine without daily and permanent discomfort. Your walking distance and mobility are clearly reduced.
Alternative treatment methods (physiotherapy) will no longer be successful.
You depend on a constant intake of drugs. These are no longer sufficient despite increased
If these factors apply to you, an operation should be considered regardless of your age.
If the above circumstances do not apply to you, it is advisable to postpone an operation and to look for further non-operative treatment methods.
What risks do the implantation of a partial knee replacement involve?
In Europe, an average of 550,000 artificial hip joints and 230,000 knee joints are implanted per
year. Today, the operation is a routine intervention.
However, risks of such things as bleeding, drug allergies, deep vein thromboses, pulmonary em-
bolisms or infections cannot be fully excluded.
Preventive measures, such as the administration of drugs and physiotherapy, limit these risks to a
large extent. Your doctor will provide you with further information on the subject.
When will I be able to drive a car again?
You should only get behind the wheel when you feel fit to drive. You are the one responsible for
this! We recommend that you consult with your attending specialist first. Never drive under the
influence of strong pain relievers!
When can I be sexually active again?
You should not make any strong knee-bends in the first six to twelve weeks after the operation,
in order to prevent an irritation of the joint or a feeling of strain.
Other than that there is nothing else that interferes with sexual intercourse. Your doctor will be
happy to answer any questions.
In conclusion
Arthritis of the knee is a degenerative disease, although occasionally it is caused by an earlier injury.
A partial knee replacement can relieve pain and stiffness and make walking easier. In the majority
of cases, surgery is safe and effective, but complications can arise and if you know about them,
this can help you to prevent them or enable you to seek help if they do occur.
If you have any queries or questions about any of the information contained within this brochure,
then please contact the London Knee Clinic on 020 7407 3069. Further information is available
on our website www.londonkneeclinic.com.
Along with the practitioners of the medical arts, you are responsible for your partial knee joint and can contribute a great deal to your therapeutic success. Your cooperation is of the utmost importance. We hope that this brochure has explained the most important factors and procedures.
Acknowledgments: Our thanks to Mathys Orthopaedics who have produced and supported this publication (www.mathysmedical.com).
Published by:
Presented by:
London Knee ClinicLondon Bridge HospitalSt Olaf House
Mathys Ltd Bettlach
P.O. Box2544 Bettlach
Source: http://www.londonkneeclinic.com/data/documents/Partial%20Knee%20Brochure.pdf
Relations Homme-Animal Quoi de neuf ? Glasgow en Ecosse est depuis des siècles un lieu de rencontres et d'échanges, centré notamment autour de son université (1450) et du célèbre Collège de Médecine Vétérinaire (1863), devenu faculté en 1949. Glasgow fut aussi l'un des centres importants de l'Art Nouveau, grâce à ses architectes-décorateurs, dont le célèbre Mackintosh. La ville, qui porte toujours les traces de son riche passé industriel (notamment naval), se donne peu à peu un nouveau visage, à grands coups de rénovations urbaines. Ainsi en est-il du « Scottish Exhibition and Conference Centre », bâti sur les anciens docks le long de la rivière Clyde et dont la structure audacieuse ne va pas sans rappeler celle de l'Opéra de Sydney. C'est là que s'est tenue, du 6 au 9 octobre dernier, la 10ème Conférence Internationale sur les Relations Homme-Animal, avec pour thème
of dietary supplements labeled as ephe- 5. James, W.P. et al. Effect of sibutramine on as demonstrated by imatinib (Gleevec)1 cardiovascular outcomes in overweight and dra free is an example of important and gefitinib (Iressa),2 and it has raised obese subjects. N. Engl. J. Med. 363, 905–917 work that protects the public by helping expectations for the majority of drug