Immediateearly function of neoss implants placed in maxillas and posterior mandibles: an 18month prospective case series study
Immediate/Early Function of Neoss Implants
Placed in Maxillas and Posterior Mandibles:
An 18-Month Prospective Case Series Study
Leonardo Vanden Bogaerde, MD, DDS;* Giorgio Pedretti, MD, DDS;† Lars Sennerby, DDS, PhD;‡
Neil Meredith, DDS, PhD§
Background: An increasing number of studies show that immediate/early function of dental implants can be as successfulas two-stage procedures. However, the results may not be universal for all implant types and it is important that newimplants are tested for this treatment modality.
Purpose: The aim was to evaluate an immediate/early function protocol in the maxilla and in the posterior mandible usingNeoss implants (Neoss Ltd., Harrogate, UK).
Materials and Methods: A total of 21 patients were provided with 69 Neoss implants (4 mm in diameter and 9–15 mm inlength) and a provisional bridge within 7 days (mean 4.6 days). Sixteen implants were placed in immediate extraction siteswhere seven were treated with autologous bone grafts (
n = 6) or bone grafts + resorbable membrane (
n = 1). A final fixedprosthesis was made 3 to 6 months later. The patients were followed-up with clinical examinations for 18 months. Inaddition, the implants were monitored with resonance frequency analysis (RFA) measurements at surgery and after 1, 2,and 6 months. Intraoral radiographs were taken after surgery and after 1, 6, and 18 months.
Results: One implant in an extraction site in the maxilla failed after 1 month, giving a survival rate of 98.5% after 18 months.
The mean marginal bone loss was 0.7 mm (SD 0.7) after 18 months. RFA showed a mean implant stability quotient (ISQ)value of 68.1 (SD 8.8) at surgery, which increased to 73.7 (SD 5.7) after 6 months. The primary stability for maxillary andmandibular implants was similar, although mandibular implants showed slightly higher values with time. Implants inextraction sockets showed a lower initial stability than in healed sites, ISQ 65.8 (SD 7.5), which increased to ISQ 67.5 (SD6.9) after 6 months. The failed implant showed an ISQ of 74 at placement, which decreased to 42 1 month after surgery.
Conclusion: Within the limitations of the present study, it is concluded that immediate/early function with Neoss implantsis a reliable method with an implant survival rate comparable to that of the traditional two-stage protocol.
KEY WORDS: clinical study, dental implants, immediate/early function, radiography, resonance frequency analysis
traditional healing period of 3 to 6 months. However,
Immediate loading is today a commonly used term in
the applied load is often reduced or even absent; there-
the dental field and indicates the possibility of applying
fore, it is more correct to use the term "immediate/early
an occlusal load to dental implants earlier than the
function" rather than "immediate/early loading." More-over, the subdivision between "immediate function" –
*Private practice, Concorezzo, Italy; †private practice, Lecco, Italy;
when the prosthesis is applied within hours from the
‡Professor, Department of Biomaterials, Institute of Surgical Sciences,
implant insertion – and "early function" – when the
Sahlgrenska Academy, Gothenburg University, Sweden; §Professor,
prosthesis is applied earlier than the traditional period
Bristol Dental School and Hospital, Bristol University and Neoss Ltd.,Harrogate, UK
of 3 to 6 months – has been accepted at a previousconsensus conference.1
Reprint requests: Dr. Leonardo Vanden Bogaerde, Via Dante 32, 20049Concorezzo, Italy; e-mail:
[email protected]
The possibility to rehabilitate the aesthetics of a
2008, Copyright the Authors
patient in a very short period and avoiding a removable
Journal Compilation 2010, Wiley Periodicals, Inc.
prosthesis are without any doubt the main reasons for
which the immediate function therapy is performed.
Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
Moreover, occlusal loading of the implants can be
96.8% after 18 months. The result obtained in that study
allowed to assure a certain degree of masticatory func-
was significantly better than those obtained in previous
tion in accurately evaluated and monitored patients. Not
studies in which cylindrical implants were used.6,7A
to be disregarded is the observation that early function
perspective clinical study confirmed the possibility to
may have a favorable effect on bone formation and
use implants with favorable geometry in the posterior
mineralization,2 determining a higher degree of bone–
regions of the maxillas, obtaining a survival rate of 98%,
implant contact.3
after 1 to 2 years.11
The first procedures of immediate function were
The mechanical anchorage of the implant in the
carried some 20 years ago and essentially considered the
bone (primary stability) tends to decrease during the
chin symphysis, an area of the mandible characterized
first weeks following the positioning12 and is progres-
by a high bone density. The results of many clinical
sively replaced by an anchorage of biological type, tied to
studies have confirmed the validity of the technique
the implant surface (secondary stability). During the last
applied to the anterior mandible.4–5 Afterward, the pos-
years, a progressive abandon of the smooth surface
sibility to intervene also in areas where the bone quality
(machined) in favor of a rougher surfaces has been
is less favorable, like the upper arch or, in some cases, the
observed. While the surface does not seem to have any
posterior mandible areas, was investigated. Glauser and
particular influence on the primary stability,8,13 on the
colleagues6 treated different areas of the arches with an
secondary stability, it does influence it in a determining
immediate loading procedure, obtaining a survival rate
way, accelerating the osseointegration process. A con-
of 66% in the posterior maxilla; while in the other areas
trolled study was carried out in a dog mandible,14 com-
the survival was up to 91%. Grunder and colleagues7
paring implants with machined surface (control side)
inserted 48 implants in totally edentulous upper and
with implants with oxidized rough surface (test side),
lower arches. At the follow-up after 2 years, six implants
with a resonance frequency (resonance frequency analy-
failed in the posterior areas, resulting in a survival rate of
sis [RFA]) monitoring. After 3 weeks, the test implants
showed a value of implant stability quotient (ISQ)
It was then understood that the primary stability of
greater than that of the control implants. Another his-
the implant is fundamental to obtain the successful
tomorphometrical and biomechanical study performed
outcome of immediate function in areas with poor bone
on rabbits15 put in evidence that implants with a rough
quality. Apart from the bone density, the primary stabil-
(oxidized) surface showed after 6 weeks higher values of
ity seems to be related to the surgical technique (under-
bone–implant contact (BIC) and of "removal torque"
preparation of the site) and particularly to the geometry
than those of implants with machined surface. Such
of the implant.
results have also been confirmed by Henry and col-
In an experimental study, Glauser and colleagues8
leagues16 in a study on a dog in which implants with
inserted implants with a different geometry and ana-
rough surface showed, after 6 weeks, an extraction
lyzed the initial stability by the insertion torque and the
torque higher than that of implants with machined
resonance frequency. The authors concluded that the
positioning of slightly tapered implants in a cylindrical
Vanden Bogaerde and colleagues17 carried out a
site gives a greater stability in comparison with cylindri-
multicenter study with a protocol similar to the one of
cal implants. These data have been clinically confirmed
the previous study of the same authors,10 except for the
by a study in which the survival rate of implants in soft
use of implants with rough (oxidized) surface. One
bone has been higher than that obtained with cylindrical
hundred eleven implants were positioned in edentulous
implants.9 It seems that the implant tapered design
areas of the maxillas and posterior mandibles and early
creates bone compression at the moment of the implant
loaded within 9 days from the insertion. The follow-up
insertion and therefore a better stability.
after 18 months showed the failure of one implant only,
In a multicenter perspective study, Vanden Bogaerde
with a survival rate of 99.1%. The average marginal bone
and colleagues10 installed 124 slightly tapered implants
resorption has been 0.8 mm with a loss mainly concen-
with a smooth surface in upper arches and posterior
trated in the first 6 months. The effectiveness of the use
mandibles and loaded them within 15 days from the
of the rough, oxidized surface has been confirmed by a
surgery. The total survival rate of the implants was
1 year perspective clinical research.18 The authors
Immediate/Early Function of Neoss Implants
positioned 102 implants with rough surface, mainly in
the posterior areas of the maxillas and in the presence of
(OPGs) and/or computed tomography scans.
soft bone, obtaining an implant survival rate of 97.1%.
Inclusion criteria were (1) need of implant-
Once more, a comparative study19 using implants with
supported crown or bridge in the partially edentulous
smooth surface (machined) and implants with rough
mandible or maxilla; (2) available bone for at least
surface (oxidized), inserted in posterior mandibles and
9-mm long and 4-mm wide implants; (3) minimal peak
early loaded, showed a greater success for the rough
insertion torque of 30 Ncm; (4) minimal ISQ value of 50
implants (10% more) compared with the machined
(Osstell™, Osstell AB, Gothenburg, Sweden); and (5)
ones. The same authors histologically investigated the
signed informed consent to participate and to follow a
osseointegration process in implants subjected to early
maintenance and observation program for 18 months.
loading, inserting nine supplementary implants in five
The exclusion criteria were (1) noncompensated dis-
voluntary patients.20 Such implants were extracted after
eases; (2) poor oral hygiene; and (3) the presence of a
5 to 9 months of function and the histological analysis
"deep bite" in the superior central incisors.
revealed a BIC rate of 84.5%.
Smoking, bruxism, and periodontal disease were
The aim of the present work is to evaluate the
considered only as risk factors. Patients with periodon-
immediate/early loading in the maxilla and in the man-
titis were treated before implant surgery. Immediate
dible with a new type of implant (Neoss Implant
placement of implants in extraction sockets was allowed.
System) with rough surface (bimodal) and a geometry
All patients were carefully informed about the
slightly tapered in its apical part.
procedure and gave their written consent to partici-pate. They could at any time point refuse further
MATERIAL AND METHODS
Patient Selection
A total of 21 patients (12 females and nine males; mean
age 60 years, range 32–79) coming from two clinical
Neoss™ implants (Neoss Ltd., Harrogate, UK) were used
centers were consecutively included in the study.
in the study (Figure 1). This implant is characterized by
Twenty-seven partially edentulous areas were treated; 16
a positive tolerance, signified by a slightly tapered geom-
situated in the upper arch and 11 in the lower arch
etry. The implant has a modified surface obtained by
double particle blasting (Bimodal™ surface, Neoss Ltd.),
The preoperative assessments included clinical
first with larger ceramic particles to obtain a macror-
oughness and then with smaller particles to obtain a
TABLE 1 Position and Length of the Implants (4 mm in Diameter) Used in
the Study

Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
3.0 mm, and 3.4 mm). In the presence of very soft bone,an under-preparation technique was used with 3.0 or3.2 mm as final diameter.
To preserve the cortical bone as much as possible,
the use of countersink was avoided. Thus, the implantswere generally placed with the implant collar above thebone crest.
In the immediate postextractive sites, careful curet-
tage of the socket was performed just after the extractionof the tooth to remove any residual inflammatory tissueor periodontal ligament. The postextraction siteswere divided into groups according to the followingclassifications21:
ESND (extraction socket, no defect) – When thediameter of the socket was smaller than that ofthe implant and no defect remained adjacent to theimplant.
ESCD (extraction socket, closed defect) – When thediameter of the socket was larger than that ofthe implant and one defect remained adjacent to theimplant but with bone walls preserved (closeddefect). This was treated with autologous bone
Figure 1 Design of the Neoss™ implant used in the study. The
grafts taken from the neighboring areas with a bone
implant has a 1.9-mm high collar and a threaded body with a
scraper (Micross®, Meta, Reggio Emilia, Italy).
positive tolerance and vertical flutes. The Bimodal™ surface isachieved by blasting with two different sizes of ceramic
ESOD (extraction socket, open defect) – When the
diameter of the socket was larger than that ofthe implant and one defect remained adjacent to theimplant but without bone walls (open defect). This
microroughness. According to the manufacturer, the
was treated with autologous bone and a resorbable
roughness is higher on the body and less at the neck of
polyglycolid acid (PGA)-trimethylene carbonate
the implant.
(TMC) membrane (WL Gore & Associates Inc.,
A total of 69 implants were inserted: 41 in the upper
Flagstaff, AZ, USA) was used.
arch and 28 in the posterior area of the mandible(Table 2). Implants with lengths of 9 to 15 mm and a
TABLE 2 Number of Patients, Prostheses, and
diameter of 4 mm were inserted (Tables 1 and 2).
Implants Used in the Study
Sixteen implants were positioned in immediate pos-
textraction sites.
Surgical and Prosthetic Procedures
The patients were given 2 g of amoxicillin (Zimox®,
Pfizer, Italy Srl) before implant surgery. The implant
sites were exposed via a midcrestal incision followed by
a releasing distal incision. A full thickness flap was
elevated and the positions of the implants were marked
with a round bur. Then, the receiving sites were prepared
with cylindrical burs of increasing diameter, accordingto the recommendations of the manufacturer (2.2 mm,
GBR = guided bone regeneration.
Immediate/Early Function of Neoss Implants
After the complete positioning of the implants,
sterile impression transfers were connected and the flapswere sutured. Impressions were taken with an open trayusing Impregum NF® (ESPE, Seefeld, Germany).
Healing abutments were attached to the implants.
A bite registration was taken in centric relation
with occlusion waxes. The impressions were sent to thelaboratory for the manufacturing of the temporaryprosthesis.
The patients were treated with a postsurgical anti-
biotic therapy (amoxicillin, Zimox®, Pfizer, Italy Srl), 1 gtwice a day for 6 days, starting just before surgery, an
Figure 2 Edentulous space in the lower posterior arch.
anti-inflammatory therapy, (nimesulide, Aulin®, Roche,Milan, Italy), twice a day for 4 days, and they wereinstructed to rinse with 2% solution of chlorexidine,
implants two ISQ values, one low and one high. Of the
twice a day for 10 days.
two values, only the greater one was registered as recom-
A temporary prosthesis made of acrylic with a metal
mended by the manufacturer.
reinforcement, without distal extensions, with a reduced
As previously mentioned, a baseline threshold value
platform, and flattened cusps was delivered within 7
of 50 ISQ was scheduled as a minimum stability quo-
days (average 4, 6 days, range 0–7 days). In the wait-
tient in order to perform the procedure of immediate
ing period, the patients did not use any removable
The occlusion was in centric, with light contacts,
Implant Survival Criteria
possibly avoiding lateral and protrusion contacts. The
An implant was considered surviving if it is clinically
occlusion marking paper had to leave less marked
stable and if it complies with the function of supporting
impressions on the prosthesis and on the implants com-
the prosthesis and is causing no discomfort to the
pared to those of the adjacent teeth. A fixed final pros-
patient. Failure was defined as removal of an implant
thesis made of porcelain casted on golden alloy was
due to any reason.
made after 3 to 6 months.
Radiographic Examination
Twenty of the patients were followed up for a period
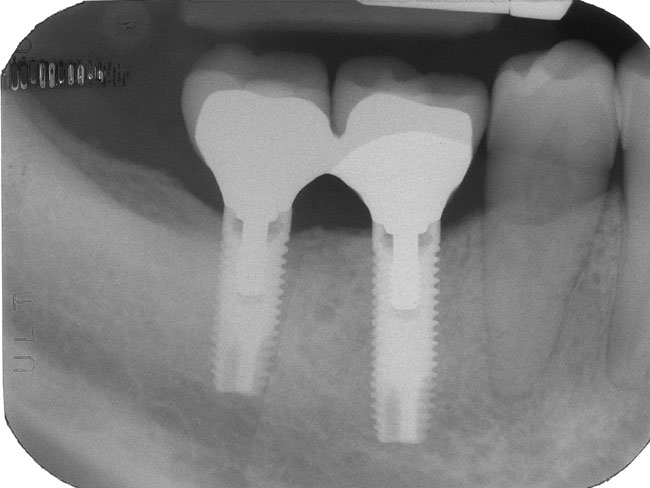
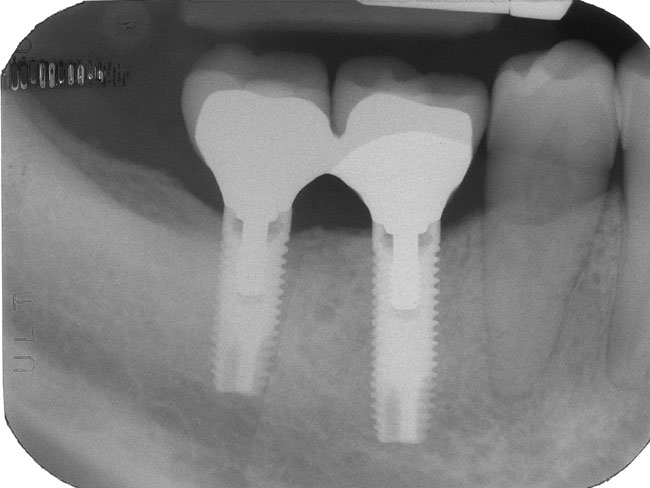
Intraoral radiographs were taken after insertion of the
of 18 months and only one patient discontinued the
implant (baseline), and then after 1, 6, and 18 months
treatment. Figures 2 to 6 show a clinical case of partial
from the installation of the implant using a parallelingtechnique (Dentsply RINN, Elgin, IL, USA).
The radiographs were examined by an independent
radiologist. The upper corner of the coronal shoulder ofthe implant was used as reference point. Measurementsfrom the reference point to the first bone contact at themesial and distal aspects of the implant were performed.
A mean value was calculated for each implant and timepoint.
Implant stability measurements were performed at base-line and after 1, 2, and 6 months using RFA measure-ments (Osstell Mentor™, Osstell AB) expressed in ISQunits. This novel wireless RFA technique gives for many
Figure 3 Two implants positioned with a full thickness flap.
Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
Figure 4 After connecting the transfers to the implants, the
flaps were sutured and an impression taken.
Figure 6 The follow-up after 18 months shows an optimal
maintenance of the bone marginal level.
edentulism in the posterior lower arch. Figures 7 to 11show a case of partial edentulism in the maxilla with the
some particulate autologous bone. One case presented
presence of a high bone deficiency.
an "open" defect with no walls (ESOD group) and wastreated with bone grafts and a resorbable membrane
Clinical Examination
One of the 69 implants was diagnosed as a failure, giving
Radiographic Examination
a survival rate of 98.5% after 18 months. The failureoccurred 4 weeks after placement in an immediate pos-
The radiographic measurements showed that the base-
textraction site in the anterior maxilla in a patient
line bone level was situated 0.8 mm (SD 0.2) (n = 58)
affected by serious periodontitis.
from the top of the collar and 1.7 mm (SD 0.3) (n = 47)
Sixteen implants were inserted in immediate pos-
and 1.4 mm (SD 0.6) (n = 57) after 6 and 18 months,
textraction sites (Table 1). In nine cases, the implant
respectively (Table 2). Thus, a marginal bone resorption
diameter was equal or larger than that of the postextrac-
of 0.9 mm (SD 0.3) (n = 47) after 6 months and 0.7 mm
tion socket and filled the receiving site completely
(SD 0.7) (n = 53) after 18 months were seen (Table 3).
(ESDN group). In seven cases, a "gap" remained between
The proportion of implants showing more than 2-mm
bone and implant and regenerative therapy was per-
bone resorption was 13.2% and no implant showed
formed. In six of these cases, the defects were of the
more than 3-mm bone loss over 18 months (Table 4).
"closed" type (ESCD group) and they were filled with
Figure 7 Two implants positioned in the superior maxilla, in
immediate postextraction sites. The distal implant shows a large
Figure 5 The final gold-ceramic prosthesis after 3 months.
surface and exposed implant threads.
Immediate/Early Function of Neoss Implants
Figure 8 The bone defect has been filled with a mixture of
Figure 11 After 6 months, the surgical reentry shows complete
autologous bone/bovine bone deproteinized and then covered
coverage with new bone of the previously exposed implant area.
with a reabsorbable membrane.
The resonance frequency reveals a significant increase (implantstability quotient [ISQ] 61), compared with the baseline (ISQ51).
A total of 59 implants were systematically analyzed with
8.8), 66.0 (SD 8.5), 69.1 (SD 6.9), and 73.6 (SD 5.7) at
RFA measurements. The mean ISQ values were 68.1 (SD
baseline and after 1, 2, and 6 months, respectively.
There was no major difference in stability between
the maxilla, although mandibular implants showedslightly higher values with time (Figure 12).
The implants positioned in the postextraction sites
with "closed" defects (n = 6) showed an average ISQ of65.8 (SD 7.5) at baseline, which increased to 67.5 (SD6.9) after 6 months (Figure 13).
The only implant associated with an "open" defect
showed a rather low starting value, ISQ 51, which
TABLE 3 Results from Radiographic Measurements
Based on Mean Values of Distal and Mesial Aspects
Figure 9 The flaps were sutured around the transfers and an
impression was taken.
0.8 (SD 0.2) (n = 58)
1.7 (SD 0.3) (n = 47)
0.9 (SD 0.3) (n = 47)
1.4 (SD 0.6) (n = 57)
0.7 (SD 0.7) (n = 53)
TABLE 4 Distribution of Marginal Bone Loss after
18 months in Function
Figure 10 After 4 days, the temporary prosthesis was applied.
Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
Figure 12 Graph showing the stability of maxillary and
Figure 14 Graph showing the development of seven implants
mandibular implants with time. ISQ = implant stability
showing falling stability from baseline to 1 month. Hatched line
showing the mean stability of the seven implants. ISQ = implantstability quotient.
remained unchanged during 4 weeks (ISQ 52) and then
significantly increased after 8 weeks to 56 and finally 64
The present study confirms the results from previous
after 6 months (Figure 13).
clinical investigations that good outcomes can be
The implant that failed (position 12) was installed
obtained with early loading of implants positioned in
in an immediate postextractive site and, at the moment
the upper arch and in the posterior lower arch, regions
of the insertion, it had an ISQ 74. After 4 weeks, the
which often are characterized by poor quality
patient reported pain in that area and the analysis with
bone.9,10,11,17–19,21 There are many advantages with this
the resonance frequency showed a value of ISQ 42
method such as (1) preservation of the aesthetics; (2)
associated with an initial mobility of the implant and the
early occlusion loading, even if often reduced; (3) very
appearance of bone peri-implant rarefaction. With these
rapid procedure and therefore less discomfort for the
clinical conditions, it was impossible to save the implant,
patient; (4) lower number of operating stages for the
and a decision was reached to remove it.
dentist; (5) probable less bone marginal resorption;22
Some implants (n = 7) showed a significant
and (6) possible advantages for the peri-implant bone
decrease of their stability at 1 (n = 3) and after 2 months
generation. Concerning the latter, it has been observed
(n = 4), maintaining, however, the anchoring in the
that cylindrical implants with machined surface sub-
bone and showing even a significant recovering after 6
jected to immediate function have a positive effect on
months (n = 5) (Figure 14). Only two implants showed a
the osteogenesis.2 When implants are loaded for 12
continuous decrease of stability up to 6 months.
weeks, the presence of peri-implant osteoid tissue andthe BIC increase significantly. Another study on pri-mates confirmed that immediately loaded implantsshow a greater BIC (62.4%) compared with that of notloaded implants (56.3%).3
According to our protocol, immediate postextrac-
tion sites (n = 16) were included with the purpose topreserve the bone ridge level as much as possible. It hasbeen observed that after the extraction of the tooth, abone ridge resorption of even 50% takes place after 1year, with 2/3 of this process occurring during the first3 months.23 Maintenance of the ridge is particularlyimportant in those situations where the height of theavailable bone is limited and the implant can help to
Figure 13 Graph showing development of stability for implants
maintain the existing bone. Even more important is
in healed sites, in closed extraction defects, and in one case withan open extraction defect. ISQ = implant stability quotient.
the need to maintain the marginal bone level and,
Immediate/Early Function of Neoss Implants
consequently, the soft tissue level too, in the front areas
interesting to observe the progressive increase of the
of the arches where the aesthetics play a fundamental
implant stability (Figure 12), probably proportional to
role. It has been demonstrated that the positioning of an
the bone regeneration. The second surgical phase after 6
implant in a fresh extraction site can prevent the resorp-
months (Figure 11) showed an almost total coverage of
tion, especially on the buccal side where the bone is
the implant surface, which was previously exposed,
demonstrating that the guided bone regeneration can
In a study using immediate function in the front
take place also in case of implants subjected to immedi-
areas of the maxilla, implants were positioned also in
immediate postextractive sites.26 The authors observed
A noninvasive method for the evaluation of the
that all implant failures occurred in the postextractive
implant stability has been proposed by Meredith and
sites and concluded that such sites represented a risk
colleagues28 Such device measures the resonance fre-
factor for the immediate function protocol. On the con-
quency of a transducer tied to the implant or to the
trary, an 18-month perspective clinical study demon-
abutment. The transducer transmits the vibrations of
strated the possibility to carry out an immediate
sinusoidal type which are received by a second frequency
function protocol with success also in postextractive
analysis element. The stability values are expressed in
sites, provided the respect for a rigorous clinical proto-
ISQ. According to the authors, the resonance frequency
col.21 The authors positioned 50 implants in 22 edentu-
is determined by the rigidity of the implant/tissues inter-
lous areas in the maxilla or in the posterior mandible,
face and by the distance between the transducer and
classifying the defects according to the preservation or
the first bone contact. In following studies, the same
not of the surrounding bone walls. The peri-implant
researchers have been able to confirm the correlation
defects were treated with particulate autologous bone
between the measurements with the resonance fre-
grafts or grafts associated with resorbable membranes.
quency and the rigidity of the implant inside the bone
All the implants had to have a sufficient primary stability
tissue.29–30 Glauser and colleagues31 carried out a study
as evaluated by the resonance frequency. At the end of
on 23 patients subjected to the procedure of immediate
the follow-up period, all the implants resulted to be
function, monitoring for 1 year the stability of the
stable, with a total survival rate of 100%.
implant by means of the resonance frequency. The
The healing of peri-implant defects, following the
authors observed that the implants subjected to a suc-
implant insertion in postextractive sites, depends also on
cessive failure showed a continuous drop of stability up
the dimension of the residual "gap." Wilson and col-
to the loss of the implant. Moreover, low stability values
leagues27 evaluated the bone healing around implants
after 1–2 months seemed to indicate an increased risk of
inserted just after the tooth extraction and retrieved
failure. In another experimental study, some implants
after 6 months for histological analysis. The BIC was
with machined and rough surface were positioned in
72% on the control side (not postextractive areas), 50%
dog mandible.32 Around the implants, in subgingival
for implants with an initial defect equal or less than
position, some ligatures were applied for 3 months with
1.5 mm, and 17% for implants with an initial defect of
the purpose to cause an experimental peri-implantitis.
4 mm. Therefore, the bigger the initial defect, the smaller
Afterward, a regenerative therapy was started, including
debridement and cleaning of the implant surface. For
In the present study, 16 implants were inserted in
the monitoring of the implant stability, the resonance
fresh postextractive sites. Nine of these implants com-
frequency was used. During the peri-implantitis phase,
pletely filled the sockets (ESND group), and did not
it has been possible to observe a loss of bone associated
require a regenerative therapy. Near to six implants,
to the drop of implant stability. Later, such stability
there were defects with preserved walls (ESCD group),
tended to increase during the healing phase and it was
and a regenerative treatment was executed with particu-
more pronounced in the case of implants with rough
late autologous bone taken from the neighboring areas
surface. The authors concluded that there is a direct
with a "scraper." Only one implant presented a serious
correlation between the marginal bone level and the
defect with the lack of walls (ESOD group), and this
resonance frequency values.
area was treated with autologous bone covered with a
According to some authors, a significant drop of
resorbable membrane (Figure 8). In this last case, it was
stability occurs after some weeks from the implant
Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
insertion. According to some authors, this period can be
the implant from the occlusion. The successive control
quantified in 2 to 4 weeks12–33 and according to others up
after 6 months showed a recovery of stability with an ISQ
to 2 months.31 The reason for such decrease could be
value greater than the initial one. In the present study, the
attributed to the bone relaxation after the compression
implant that failed had an extremely rapid drop of stabil-
due to the insertion and to the bone adaptation during
ity and it has been impossible to intervene before losing
the healing phase. Other authors30–34 have instead
the integration. After 4 weeks, the patient reported pain,
noticed a maintaining of the bone stability during the
swelling, and a bone rarefaction in the interested area.
first weeks or even a small increase.34 In the present
This was probably due to an infection that occurred
study, the mean ISQ values at baseline remained
because of bacteria trapped during the implant insertion;
unchanged at 1 and 2 months. This behavior could indi-
as a matter of fact, it concerned an immediate postextrac-
cate that the initial stability of the Neoss implants
tive site in a patient affected by a serious form of
(Neoss Ltd.) is not tied to the excessive compression of
periodontitis. However, as observed also in a precedent
the bone tissue at the moment of the implant insertion.
study,21 a drop of stability during the first weeks does not
The mean resonance frequency values, registered at
necessarily signify an imminent risk of implant loss. In
baseline (mean ISQ 68.1) indicate that the implants uti-
the present study, on some implants (n = 7) a decrease of
lized a sufficient level of primary stability also in the
stability was observed after 4 weeks (n = 3) and 8 weeks
maxillary regions where the bone quality is less favor-
(n = 4), without any clinical signs from the implants
able. No significant differences were observed between
regarding a loss of anchorage. Some of them (n = 5), after
the upper arch (mean ISQ 68.8) and the lower arch
6 months, showed a significant increase of the resonance
(mean ISQ 67.3). These values are higher than those
value (Figure 13).
reported for Straumann implants34 (mean ISQ 57.4)
The marginal bone level measurements showed an
and comparable with those reported for Branemark35
average bone loss of 0.7 mm over 18 months, which is
implants (mean ISQ 67.4). In the present work, the
similar to the value that have been reported from our
analysis at 6 months evidenced a consistent increase of
group for other implant designs10,17,21 The bone level
stability (mean ISQ 73.6), indicating a successful process
after 18 months was on average still situated on the
of implant osseointegration. It has been noticed that the
collar, ie, 1.4 mm below the reference point on the 1.9-
lower the initial value of ISQ, the larger the growth
mm-high collar. More than 20% of the implants showed
registered at 6 months.
an increase of the bone level, which may be explained by
In the immediate postextraction sites ESCD, even
the fact that many implants were placed in extraction
though there was a residual defect, stability at baseline of
sockets. About 13% of the implants showed more than
ISQ 65.8 was obtained, which is comparable to that of
2-mm bone loss, but no implants lost 3 mm or more
implants positioned in healthy bone. Only, at the level
over 18 months in function.
of the implant positioned in a site ESOD, the initialvalue was rather low (ISQ 51), probably because of the
extensive lack of the surrounding bone. After 8 weeks,
Within the limitations of the present study, it is
the resonance frequency was already giving a signifi-
concluded that immediate/early function with Neoss
cantly increased value (ISQ 56), indicating that a regen-
implants (Neoss Ltd.) is a reliable method, with an
erative process was taking place. After 6 months, the
implant survival rate comparable with that of the tradi-
value was further increased (ISQ 64), and the second
tional two-stage protocol.
surgical intervention confirmed that the bone regenera-tion had occurred (Figure 10).
CONFLICT OF INTEREST STATEMENT
Sometimes, the resonance frequency enables to dis-
The authors have no conflicts of interest to declare.
cover a dangerous drop of stability before having an
[Correction added after online publication 24 May
implant failure. In a perspective clinical study, Vanden
2010: Conflict of Interest Statement added.]
Bogaerde and colleagues,21 with the resonance frequency,evidenced a significant and progressive loss of stability of
an implant. Such decrease of stability progressed up to
1. Aparicio C, Rangert B, Sennerby L. Immediate/early loading
the sixth week, after which a decision was made to remove
of dental implants: a report from the Sociedad Española de
Immediate/Early Function of Neoss Implants
Implantes World Congress consensus meeting in Barcelona,
implant design with turned or oxidized surface. An experi-
Spain, 2002. Clin Implant Dent Relat Res 2003; 5:57–60.
mental resonance frequency analysis study in the dog man-
2. Vandamme K, Naert I, Geris L, Sloten JV, Puers R, Duyck J.
dible. Applied Osseointegration Research 2000; 1:18–20.
Histodynamics of bone tissue formation around immedi-
15. Albrektsson T, Johansson C, Lundgren AK, Sul YT, Gottlow
ately loaded cylindrical implants in the rabbit. Clin Oral
J. Experimental studies on oxidized implants. A histomor-
Impl Res 2007; 18:471–480.
phometrical and biomechanical analysis. Applied Osseoin-
3. Suzuki JB, Misch CE, Sharawy M, et al. Clinical and histo-
tegration Research 2000; 1:21–24.
logical evaluation of immediate-loaded posterior implants
16. Henry PJ, Tan A, Hall J, Johansson C. Removal torque com-
in nonhuman primate. Implant Dent 2007; 16:176–186.
parison of TiUnite and turned implants in the greyhound
4. Henry P, Rosemberg J. Single-stage surgery for rehabilitation
dog mandible. Applied Osseointegration Research 2000;
of the edentulous mandible: preliminary results. Pract Peri-
odontics Aesthet Dent 1994; 6:1–8.
17. Vanden Bogaerde L, Pedretti G, Dellacasa P, Mozzati M,
5. Ericsson I, Randow K, Nilner K, Petersson A. Immediate
Rangert B, Wendelhag I. Early function of splinted implants
functional loading of Brånemark dental implants. A 5-year
in maxillas and posterior mandibles, using Brånemark
clinical follow-up study. Clin Impl Dent Relat Res 2000;
System® TiUnite™ implants: an 18-month prospective clini-
cal multicenter study. Clin Oral Impl Res 2004; 6:121–129.
6. Glauser R, Rèe A, Lundgren AK, Gottlow J, Hämmerle C,
18. Glauser R, Lundgren AK, Gottlow J, et al. Immediate
Schärer P. Immediate occlusal loading of Brånemark
occlusal loading of Brånemark TiUnite implants placed pre-
implants applied in various jawbone regions: a prospective,
dominantly in soft bone: 1-year results of a prospective clini-
1-year clinical study. Clin Impl Dent Relat Res 2001; 4:204–
cal study. Clin Impl Dent Relat Res 2003; 5:47–56.
19. Rocci A, Martignoni M, Gottlow J. Immediate loading
7. Grunder U. Immediate functional loading of immediate
of Brånemark System® TiUnite™ and machined surface
implants in edentulous arches: two-year results. Int J Peri-
implants in the posterior mandible: a randomized open-
odontics Restorative Dent 2001; 21:545–551.
ended clinical trial. Clin Impl Dent Relat Res 2003; 5:57–
8. Glauser R, Portmann M, Ruhstaller P, Gottlow J, Schärer P.
Initial implant stability using different implant designs and
20. Rocci A, Martignoni M, Burgos PM, Gottlow J, Sennerby L.
surgical techniques. A comparative clinical study using inser-
Histology of retrieved immediately and early loaded oxi-
tion torque and resonance frequency analysis. Applied
dized implants: light microscopic observations after 5 to 9
Osseointegration Research 2001; 1:6–8.
months of loading in the posterior mandible. Clin Impl Dent
9. Åstrand P, Billstromm C, Feldmann H, et al. Tapered
Relat Res 2003; 88–98.
implants in jaws with soft bone quality: a clinical and radio-
21. Vanden Bogaerde L, Rangert B, Wendelhag I. Immediate-
graphic 1-year study of the Branemark System Mark IV
early function of Brånemark System® TiUnite™ implants in
fixture. Clin Impl Dent Relat Res 2003; 5:213–218.
fresh extraction sockets in maxillae and posterior mandibles:
10. Vanden Bogaerde L, Pedretti G, Dellacasa P, Mozzati M,
an 18-month prospective clinical study. Clin Implant Dent
Rangert B. Early function of splinted implants in maxillas and
Relat Res 2005; 7(Suppl 1):121–130.
posterior mandibles using Brånemark System® machined-
22. Engquist B, Arstrad P, Anzen B, et al. Simplified method of
surface implants: an 18-month prospective clinical multi-
implant treatment in the edentulous lower jaw: a 3-year
center study. Clin Impl Dent Relat Res 2003; 5:21–28.
follow-up report of a controlled prospective study of one-
11. Calandriello R, Tomatis M, Rangert B. Immediate functional
stage versus two-stage surgery and early loading. Clin Impl
loading of Brånemark System® implants with enhanced
Dent Relat Res 2005; 2:95–104.
initial stability: a prospective 1- to 2-year clinical and radio-
23. Schropp L, Kostopoulos L, Wenzel A. Bone healing following
graphic study. Clin Impl Dent Relat Res 2003; 5:10–20.
immediate versus delayed placement of titanium implants
12. Barewal RM, Oates TW, Meredith N, et al. Resonance fre-
into extraction sockets: a prospective clinical study. Int J Oral
quency measurements of implant stability in vivo on
Maxillofac Implants 2003; 18:189–199.
implants with a sandblasted and acid-etched surface. Int J
24. Nemcovsky CE, Artzi Z, Moses O, Gelernter I. Healing of
Oral Maxillofac Implants 2003; 18:641–651.
marginal defects at implants placed in fresh extraction
13. Rompen E, DaSilva D, Hockers T, et al. Influence of implant
sockets or after 4–6 weeks of healing. A comparative study.
design on primary fit and stability. A RFA and histological
Clin Oral Implants Res 2002; 13:410–419.
comparison of MKIII and MKIV Brånemark implants in the
25. Nir-Hadar O, Palmer M, Soskolne WA. Delayed immediate
dog mandible. Applied Osseointegration Research 2001; 1:9–
implants: alveolar bone changes during the healing period.
Clin Oral Implants Res 1998; 9:26–33.
14. Rompen E, DaSilva D, Lundgren AK, Gottlow J, Sennerby L.
26. Malò P, Rangert B, Dvärsäter L. Immediate function of
Stability measurements of a double-threaded titanium
Brånemark implants in the esthetic zone: a retrospective
Clinical Implant Dentistry and Related Research, Volume 12, Supplement 1, 2010
clinical study with 6 months to 4 years of follow-up. Clin
31. Glauser R, Sennerby L, Meredith N, et al. Resonance fre-
Impl Dent Relat Res 2000; 3:138–146.
quency analysis of implants subjected to immediate or early
27. Wilson TG, Schenk R, Buser D, Cochran D. Implants placed
functional occlusal loading. Successful vs. failing implants.
in immediate extraction sites: a report of histologic and his-
Clin Oral Impl Res 2004; 15:428–434.
tometric analysis of human biopsies. Int J Oral Maxillofac
32. Sennerby L, Persson LG, Berghlund T, Wennerberg A,
Implants 1998; 13:333–341.
Lindhe J. Implant stability during initiation and resolution
28. Meredith N, Alleyne D, Cawley P. Quantitative determina-
of experimental periimplantitis: an experimental study in
tion of the stability of the implant-tissue interface using
the dog. Clin Impl Dent Relat Res 2005; 3:136–140.
resonance frequency analysis. Clin Oral Impl Res 1996;
33. Portmann M, Glauser R. Report of a case receiving full-arch
rehabilitation in both jaws using immediate implant loading
29. Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Reso-
protocols: a 1-year resonance frequency analysis follow-up.
nance frequency measurements of implants stability in vivo.
Clin Impl Dent Relat Res 2006; 1:25–31.
A cross-sectional and longitudinal study of resonance fre-
34. Bischof M, Nedir R, Smukler-Moncler S, Bernard JP, Samson
quency measurements on implants in the edentulous and
J. Implant stability measurement of delayed and immedi-
partially dentate maxilla. Clin Oral Impl Res 1997; 8:226–
ately loaded implants during healing. A clinical resonance-
frequency analysis study with sandblasted-and-etched ITI
30. Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawlay P.
implants. Clin Oral Impl Res 2004; 15:529–539.
The application of resonance frequency measurements to
35. Ostman PO, Hellman M, Wendelhag I, Sennerby L. Reso-
study the stability of titanium implants during healing in the
nance frequency analysis measurements of implants at
rabbit tibia. Clin Oral Impl Res 1997; 8:234–143.
placement surgery. Int J Prosthodont 2006; 19:77–83.
Source: http://neoss.be/documents/publications/Vanden_Bogaerde_et_al_2010.pdf
RULES AND REGULATIONS GOVERNING THE BUSINESS OF SPORTS SCUBA DIVING IN THE PHILIPPINES PURSUANT TO THE PROVISIONS OF (1) LETTER OF INSTRUCTION 745 WHICH CREATED THE PHILIPPINE COMMISSION ON THE PROMOTION AND DEVELOPMENT OF SPORTS SCUBA DIVING IN 1978, WHICH CONSEQUENTLY OUTLINED ITS PRIMARY MANDATES, WITH REFERENCE TO (2) MALACAÑAN MEMORANDUM ORDER
C -DIDP LOCAL GOVERNANCE AND RURAL EMPOWERMENT PROJECT FOR DAVAO REGION For Inquiry: Project Management Office (PMO) Davao Integrated Development Program Ground Flr., JFM Corporate Center 848 Atis St., Juna Subd. Matina, 8000 Davao City Tel : (82) 297-0058 No. 17 (December 2008) Fax : (82) 297-1258 E-mail : [email protected] WATER SUPPLY CONSTRUCTION IN BRGY. WAAN BEGUN